Fig. 2.1
Airspace disease due to bacterial pneumonia. (a) Frontal chest radiograph reveals poorly defined lower lobe consolidation (C) with air bronchograms (arrow) and no volume loss indicating an airspace-filling process. (b) Axial CT image reveals two separate forms of airspace disease: (1) dense anterior segmental consolidation (C) and (2) bronchopneumonia pattern as evidenced posteriorly by centrilobular nodules (arrows)
Air trapping can be seen on expiratory images as an accentuation of density between adjacent areas of the lungs. When attenuation is measured, areas of air trapping maintain their low attenuation values, whereas normal lung increases in density. This is typically a manifestation of small airway disease but can result from either luminal obstruction or concentric bronchial wall thickening [3].
Architectural distortion refers to the displacement of normal lung structures with disruption of the usual lung parenchyma. It is generally associated with a fibrosing lung process (Fig. 2.2).


Fig. 2.2
Architectural distortion and honeycomb lung. Axial TSCT reveals distortion of the inferior lingular segment (arrows) and extensive honeycomb change in the right lower lobe (H)
Atelectasis is the loss of air and volume caused by the collapse of the airspaces (Fig. 2.3). It is therefore the opposite of airspace disease.
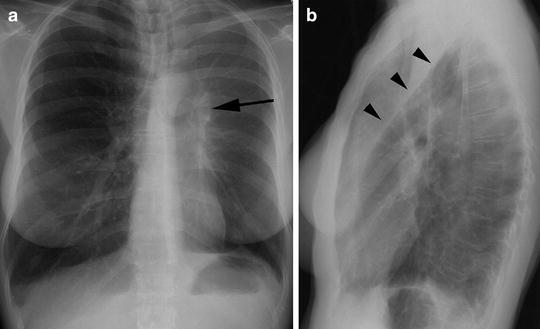
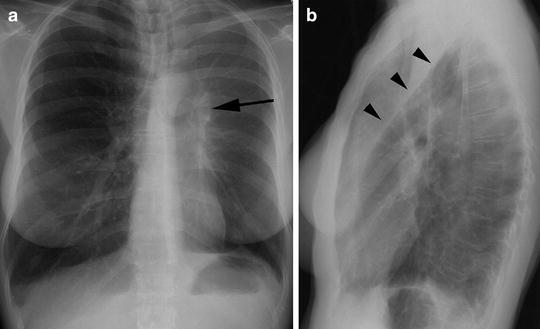
Fig. 2.3
Lobar collapse. (a) Frontal radiograph reveals volume loss in left hemithorax with elevation of left diaphragm due to left hilar neoplasm (arrow). (b) Lateral radiograph confirms collapse with anterior displacement of the major fissure (arrowheads)
Bronchiectasis is defined as irreversible dilation of the airways usually measured as 1.5× the size of the adjacent artery [4]. It can be cylindrical (long and tubular), varicoid (variable lumen size), or cystic (large gas-filled spaces) (Fig. 2.4). The relatively small artery next to a dilated bronchus has been referred to as the “signet ring sign.”
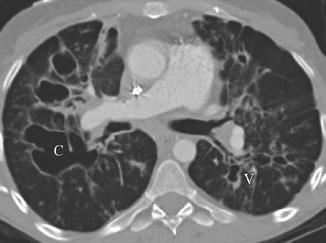
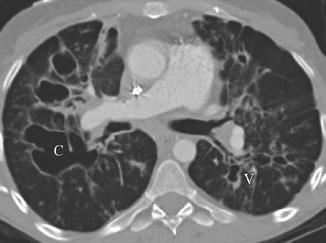
Fig. 2.4
Bronchiectasis. Axial CT in patient with cystic fibrosis reveals cystic bronchiectasis (C) in the right lung and varicoid (V) bronchiectasis in the left lung
Traction bronchiectasis is a unique subset of bronchiectasis and is related to underlying parenchymal fibrosis [5]. As opposed to bronchiectasis described above, the dilation is the result of external retractile forces. When severe, it can be quite difficult to segregate out from honeycomb lung.
Centrilobular nodules are hazy, ill-defined nodules that are centered around the central bronchus and artery in the secondary pulmonary lobule (Fig. 2.5). These nodules do not extend out to the interlobular septum and are classically associated with subacute hypersensitivity pneumonitis and respiratory bronchiolitis [1].


Fig. 2.5
Subacute hypersensitivity pneumonitis. Axial TSCT reveals both the heterogeneous generalized increase in density of ground-glass opacity and ill-defined faint nodular opacities centered in the secondary pulmonary lobule
Consolidation refers to generalized increased density within the lung parenchyma. As such it is less specific than airspace disease or atelectasis and encompasses both of those possibilities.
Crazy-paving pattern combines ground-glass opacity superimposed upon interlobular septal thickening somewhat resembling paved cobblestones. Although classically associated with alveolar proteinosis, it can occur as part of any disease process that involves both interstitium and air spaces [6].
Emphysema, like its pathological counterpart, is the irreversible destruction of alveolar walls. It can be manifest as predominately lucency of the secondary pulmonary lobule (centrilobular emphysema) or more widespread destruction of the lung parenchyma (panacinar emphysema).
Ground-glass opacity is used to describe a hazy increase in lung attenuation that does not obscure the underlying lung architecture (see Fig. 2.5) [7]. It can be associated with airspace-filling process or fibrosis that is below the resolution of CT. Because of this, the moniker of “active alveolitis” is discouraged, although this may represent reversible cellular change in the setting of interstitial lung disease.
Honeycombing is a late radiographic finding of underlying fibrosis with stacked thick-walled cystic structures (see Fig. 2.2). In the classic basal and peripheral distribution, it helps to define a usual interstitial pneumonitis pattern and obviates the need for open lung biopsy [8]. It is important to recognize that honeycombing present within a pathologic specimen may not always be evident at TSCT.
Infiltrate, as a term, should no longer be part of the imaging lexicon as it means too many different things to too many people. It should be understood as a nonspecific term in the vein of opacity and may be used with appropriate descriptors (air space, interstitial, etc.).
Interlobular septal thickening refers to any process that results in increased conspicuity of the walls of the secondary pulmonary lobule [1]. This may alternatively be described as reticular or reticulonodular opacities depending on morphology. Best seen perpendicular to the pleural surface, smooth interlobular septal thickening (Fig. 2.6) or reticular opacities are a classic manifestation of hydrostatic pulmonary edema. A beaded or reticulonodular appearance can be seen with such conditions as sarcoidosis and lymphangitic carcinomatosis.
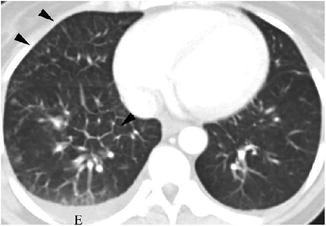
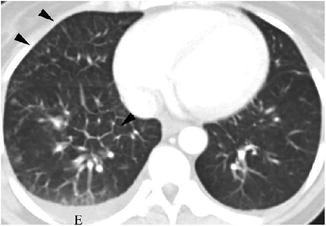
Fig. 2.6
Lymphangitic carcinomatosis. Axial CT image reveals smooth interlobular septal thickening (arrowheads) on the left compared with contralateral lung. Note also small left pleural effusion (E)
Miliary pattern is a form of interstitial disease with small nodules (1–3 mm) confined to the interstitium often in a random distribution without septal thickening. Diagnoses classically associated with this pattern include disseminated infection, particularly tuberculosis and sarcoidosis.
Mosaic attenuation is a general term used to describe differing lung densities. As such it can be due to a mixture of ground-glass opacity and normal areas of air trapping and normal lung or areas of differential (mosaic) perfusion [9]. The former two possibilities can be sorted out with expiratory images as both ground-glass disease and normal lung will both increase in density, whereas air trapping will manifest as persistent low density. Mosaic perfusion can be differentiated by looking at the underlying vessels with larger vessels going to areas of increased density and small or diminutive vessels going to areas of decreased density as in cases of chronic thromboembolic pulmonary hypertension.
Opacity, like infiltrate, should denote a nonspecific increase in density and should be preceded by an appropriate descriptor such as air space or interstitial.
Peribronchovascular nodule describes small nodules (1–3 mm) that are discretely related to the bronchial wall or peribronchial structures (Fig. 2.7). It therefore may be associated with disease of the bronchus, adjacent vessels, or lymphatics. Nodules of this variety may also be described as bronchocentric.
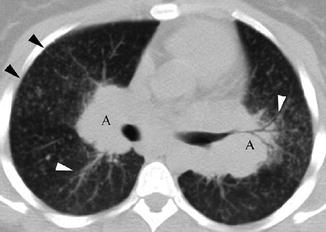
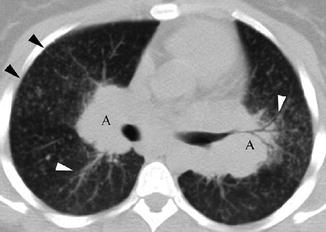
Fig. 2.7




Sarcoidosis. Axial CT reveals both subpleural/perilymphatic nodules (black arrowheads) and thickening along bronchovascular bundles (white arrowheads). Note also bilateral hilar adenopathy (A)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


