Primary Prevention of Heart Failure
David W. Baker
Stephen D. Persell
The American Heart Association (AHA) estimates that 5 million Americans have symptomatic heart failure (1), and 15 million people are affected worldwide (2). Each year another half-million Americans develop the condition (1). Persons who develop heart failure have markedly impaired quality of life and physical functioning (3), and the majority of patients will die within 5 years of their diagnosis (4,5). Despite tremendous advances in the care of patients with heart failure (6) and improvements in their survival (7,8), their prognosis remains poor. For example, the mortality rate was still approximately 6% to 9% per year in randomized controlled trials of patients with heart failure and moderate to severe left ventricular systolic dysfunction (LVEF ≤0.40) who were treated with both an angiotensin-converting enzyme (ACE) inhibitor and a β-blocker (9,10).
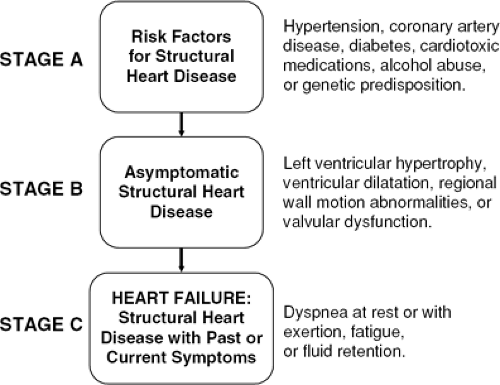
While there remain many promising new therapies for heart failure on the horizon, more attention must be given to prevention. The need for emphasis on prevention is underscored by the increasing number of older Americans and the fact that the incidence and prevalence of heart failure increase exponentially with age (11,12,13). Without improvements in prevention, the prevalence of heart failure and its health and economic consequences will certainly worsen. In recognition of this, the most recent guidelines from the AHA and the American College of Cardiology (ACC) for the evaluation and management of heart failure included a staging system to emphasize the risk factors for heart failure and the need to intervene early to prevent the development of heart failure (Fig. 30-1) (14). Stage A includes patients with risk factors for developing heart failure, including hypertension, coronary artery disease (CAD), diabetes mellitus, previous exposure to cardiotoxic agents, heavy alcohol intake, and possible genetic predisposition to cardiomyopathy (i.e., a family history of idiopathic heart failure). If left untreated, these risk factors will often produce structural heart disease. As individuals develop structural heart disease, patients will usually go through a period when they remain asymptomatic, which is classified as Stage B. Even at this point, it is still possible to intervene to prevent further progression to overt, symptomatic heart failure, which is Stage C.
Primary Prevention of Risk Factors for Heart Failure
Heart failure is a symptom complex that is the final common pathway for a wide array of diseases and pathophysiological processes. Thus, any intervention that reduces cardiovascular disease in a population will ultimately help reduce the incidence of heart failure. In the United States, these key public health targets are prevention of the development of hypertension, diabetes, and ischemic heart disease through lowering average salt intake, increasing intake of fruits and vegetables, increasing physical activity levels, decreasing obesity, reducing tobacco use, and control of dyslipidemias (15,16,17,18). Lifestyle and medical therapy to treat hyperlipidemia in accordance with the National Cholesterol Education Program guidelines are aimed primarily at reducing atherosclerotic cardiovascular disease. Controlling hyperlipidemia and preventing myocardial infarctions will ultimately lead to substantial reductions in individuals’ subsequent risk of heart failure. Likewise, the use of antiplatelet agents to prevent myocardial infarction would be expected to reduce incident heart failure (19,20,21).
Prevention of obesity deserves special comment because it is an independent risk factor for hypertension, diabetes,
and the lipid abnormalities associated with the metabolic syndrome, and recent studies suggest that obesity may directly increase the risk of developing heart failure (22,23). A full discussion of these public health measures has been reviewed by others and is beyond the scope of this chapter.
and the lipid abnormalities associated with the metabolic syndrome, and recent studies suggest that obesity may directly increase the risk of developing heart failure (22,23). A full discussion of these public health measures has been reviewed by others and is beyond the scope of this chapter.
In many developing countries, hypertension and ischemic heart disease have become common problems. For example, in India 32% of all deaths in 2000 were due to cardiovascular disease, and the prevalence of hypertension and diabetes is increasing in South Asian countries (24). In these countries, targets for preventing heart failure are similar to those in the United States. However, several other antecedents to heart failure are relevant to specific geographic regions. Heart failure resulting from valvular disease secondary to rheumatic fever remains common among Native Americans in the United States (25) and indigenous peoples in many developing countries (26,27). The incidence of rheumatic fever is related to socioeconomic conditions (25,28). Prevention of heart failure associated with rheumatic fever includes antibiotic treatment of primary streptococcal infections, continuous antibiotic prophylaxis in patients with prior rheumatic fever, and the prevention of infectious endocarditis in persons with rheumatic valvular disease (28,29).
Chagas disease, caused by the protozoa Trypanosoma cruzi, remains a common cause of cardiomyopathy in South America (30,31,32,33). Chronic Chagas disease occurs predominantly in individuals exposed to the triatomine insect vectors, usually in poor-quality housing, or directly to the T. cruzi through blood transfusion. Prevention efforts in South American countries, including the use of insecticides, health education, and surveillance for the insect vectors, have greatly reduced the incidence of Chagas disease since the 1970s (34).
The remainder of this chapter will concentrate on therapies and other strategies to treat the main modifiable risk factors for heart failure in the United States: hypertension (and secondarily, left ventricular hypertrophy [LVH]), CAD (particularly myocardial infarction), diabetes, and valvular heart disease. Improved care for these conditions can substantially reduce the incidence of symptomatic heart failure among patients in stages A and B.
Treatment of Hypertension
Although hypertension is a less-potent risk factor for developing heart failure than myocardial infarction (11), hypertension is so common that it is a major cause of heart failure in the United States. In the 1999–2000 National Health and Nutrition Examination Survey (NHANES), 28.7% of all participants and 65.4% of persons above age 60 had hypertension (35). The Framingham Heart Study estimated that 39% of all heart failure cases in men and 59% of cases in women were attributable to hypertension (36). Uncontrolled hypertension leads to LVH, CAD, and myocardial infarction. Thus, it predisposes patients to heart failure due to both systolic and diastolic dysfunction (37).
Studies have consistently shown that treatment of hypertension dramatically lowers the incidence of heart failure across a wide range of blood pressures (Fig. 30-2) (38,39,40). The benefits of blood pressure reduction vary across different health outcomes, with an approximately 46% risk reduction for heart failure, a 31% risk reduction for stroke, and a 14% risk reduction for incident coronary
heart disease. The fact that antihypertensive therapy reduces the incidence of heart failure far more than the incidence of coronary heart disease suggests a direct effect of lowering blood pressure that is not mediated through a reduction in the rate of myocardial infarction.
heart disease. The fact that antihypertensive therapy reduces the incidence of heart failure far more than the incidence of coronary heart disease suggests a direct effect of lowering blood pressure that is not mediated through a reduction in the rate of myocardial infarction.
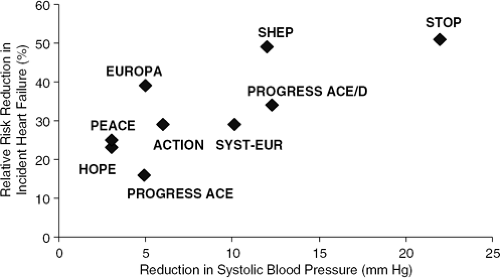 Figure 30-2 Heart failure risk reduction in major, placebo-controlled trials of antihypertensive drugs. ACE, angiotensin-converting enzyme inhibitor; D, diuretic. ACTION, A Coronary Disease Trial Investigating Outcome with Nifedipine GITS (79). EUROPA, European Trial on Reduction of Cardiac Events with Perindopril in Patients with Stable Coronary Artery Disease (76). HOPE, Heart Outcomes Prevention Evaluation Study (77); PEACE, Prevention of Events with Angiotensin-Converting Enzyme Inhibition Trial (75); PROGRESS, Perindopril Protection Against Recurrent Stroke Study (52); SHEP, Systolic Hypertension in the Elderly Program (42); STOP, Swedish Trial in Old Patients with Hypertension (41); SYST-EUR, Systolic Hypertension in Europe Trial (43). |
Several placebo-controlled studies deserve comment to exemplify the significant health benefits of treating hypertension (Table 30-1). The earliest studies focused on patients with very severe hypertension. The Swedish Trial in Old Patients with Hypertension (STOP-Hypertension) randomized patients with (a) systolic blood pressure 180 to 230 mm Hg and diastolic blood pressure greater than 90 mm Hg, or (b) diastolic blood pressure 105 to 120 mm Hg to receive either a β-blocker (atenolol, metoprolol, or pindolol at the investigator’s discretion) or placebo (41). If the blood pressure remained elevated, hydrocholorothiazide could be added. At the end of the trial, the average blood pressure was 167/87 mm Hg in the active treatment group versus 186/96 mm Hg in the placebo group. The risk of developing heart failure was reduced from 4.8% to 2.3%, a 51% relative reduction. The incidence of stroke and cardiovascular mortality were also markedly reduced. Although β-blockers were the first drug initiated in the intervention group, two-thirds of patients were receiving both a β-blocker and hydrocholorothiazide by the study end; therefore, it is not possible to distinguish which drug contributed the most to the blood pressure reduction and the improvements in outcomes.
The Systolic Hypertension in the Elderly Program (SHEP) studied patients with isolated systolic hypertension that was less severe than in STOP (Table 30-1) (42). Patients were eligible if their systolic blood pressure at enrollment was 160 to 219 mm Hg and diastolic blood pressure was less than 90 mm Hg. However, these entry criteria are somewhat misleading. At the time of the first follow-up, the mean blood pressure was 157 mm Hg in the placebo group. Patients randomized to active treatment were first given chlorthalidone with the addition of atenolol as needed for persistently elevated blood pressure (reserpine was used if atenolol was contraindicated). Half of all patients were receiving two agents at the final follow-up visit. At follow-up the difference in the mean pressure between active and control patients in SHEP was only about half of that seen in STOP (Table 30-1). Nevertheless, the benefits in SHEP were strikingly similar to STOP, with the risk of heart failure being cut in half.
The SHEP trial is also noteworthy because investigators conducted stratified analyses for patients with a prior myocardial infarction (by history or electrocardiogram). For this group, the benefits of treating hypertension were even more dramatic, with an 81% reduction in the incidence of heart failure. The enormous benefits of tight blood pressure control for patients with a prior myocardial infarction remain underappreciated, possibly because these results were reported as a subgroup analysis within the main results.
Placebo-controlled trials with dihydropyridine calcium-channel blockers (CCBs) have also been conducted among general hypertensive patient populations (i.e., not restricted to patients with previous cardiovascular disease or diabetes). The Systolic Hypertension in Europe (Syst-Eur) study had similar entry criteria to SHEP (Table 30-1) (43). Patients in Syst-Eur had similar baseline blood pressure to those in SHEP, although their diastolic blood pressure was substantially higher. The active treatment group received nitrendipine initially, which was combined with or replaced by enalapril or hydrochlorothiazide as needed. The blood pressure reduction compared to controls was similar to that in SHEP, and the absolute risk reduction and number needed to treat were nearly identical. However, the relative risk reduction for heart failure was only 29%, substantially less than in STOP and SHEP, and this reduction was not statistically significant. However, a much higher proportion of the placebo group
was treated with enalapril or hydrochlorothiazide during the study (60% versus 37% at year 3), which could partially account for the lower than expected reduction in the risk of heart failure. A similar study of nitrendipine conducted in China (Syst-China) found a 58% reduction in heart failure, although the incidence of heart failure was low and the difference in rates again did not reach statistical significance (44).
was treated with enalapril or hydrochlorothiazide during the study (60% versus 37% at year 3), which could partially account for the lower than expected reduction in the risk of heart failure. A similar study of nitrendipine conducted in China (Syst-China) found a 58% reduction in heart failure, although the incidence of heart failure was low and the difference in rates again did not reach statistical significance (44).
Table 30-1 Relative Risk Reduction (RRR) of Incident Heart Failure in Major Placebo-Controlled Randomized Clinical Trials of Treatment for Hypertension | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Thus, treatment of hypertension dramatically reduces the incidence of heart failure, and untreated and uncontrolled hypertension is a major contributor to heart failure in the United States. Even among individuals aged 80 years and older, treatment for hypertension dramatically reduces the incidence of heart failure (45). Older patients have the highest risk of heart failure but they are less likely to have their blood pressure controlled (46). It is never too late to initiate antihypertensive therapy to prevent heart failure.
How Low Is Low Enough?
The studies described above show that modest reductions in blood pressure among patients with mostly stage 1 and 2 hypertension have tremendous benefits. Although we have good data supporting the benefits of reducing systolic blood pressure into the range of 145 mm Hg, we do not know whether the incidence of heart failure can be decreased even more by reducing the blood pressure to the target of < 140/90 mm Hg currently recommended by the Seventh Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC 7) for patients with hypertension who do not have comorbid conditions (47). The Hypertension Optimal Treatment (HOT) trial randomized patients to three different diastolic blood pressure treatment goals: ≤90 mm Hg, ≤85 mm Hg, and ≤80 mm Hg (48). The lowest risk point for major cardiovascular events occurred at 138.5 mm Hg systolic and 82.6 mm Hg diastolic. However, the number of patients who developed heart failure was too small to draw conclusions.
More data are available about the benefits of trying to reach the blood pressure goal of < 130/80 mm Hg recommended by JNC for patients with diabetes. The UK Prospective Diabetes Study (UKPDS) found that patients randomized to tighter blood pressure control (mean, 144/82 mm Hg) versus less-tight control (mean, 154/87 mm Hg) had a 60% lower risk of heart failure (95% CI 20% to 80%) (49). The HOT trial found a 51% lower risk of major cardiovascular events among diabetics randomized to a target of ≤80 mm Hg compared to those with a target of ≤90 mm Hg (48). The Appropriate Blood Pressure Control in Diabetes (ABCD) Trial also showed benefits of tighter blood pressure control, including lower rates of myocardial infarction for patients with hypertension randomized to a target diastolic blood pressure of < 75 mm Hg versus a target of 80 to 89 mm Hg (50). The ABCD Trial also found lower stroke rates among diabetics without a history of hypertension who were randomized to a target diastolic blood pressure 10 mm Hg below their baseline versus a target of 80 to 89 mm Hg. However, the number of cases of incident heart failure was small in these studies and no conclusions could be drawn.
Patients with hypertension who have suffered a stroke are at high risk for other cardiovascular events, and one study suggests that tight blood pressure control in this group may reduce the risk of heart failure. In the Perindopril Protection Against Recurrent Stroke Study (PROGRESS) patients with prior stroke or transient cerebral ischemia were randomized to placebo or one of two active treatments: the ACE inhibitor perindopril alone or perindopril plus the thiazide diuretic indapamide (51,52). Pretreatment blood pressure was 147/86 mm Hg. Active treatment resulted in a 9/4 mm Hg reduction in blood pressure and a 26% reduction in incident heart failure. The group receiving both the diuretic and the ACE inhibitor had more pronounced blood pressure lowering (12.3/5.0 mm Hg versus 4.9/2.8 mm Hg), and this group had greater reductions in heart failure and major cardiovascular events than did the ACE inhibitor group alone (52,53).
In summary, reducing blood pressure to below 140/90 mm Hg has incremental benefits for reducing heart failure incidence among patients with diabetes and prior stroke. For patients who do not have diabetes or a previous stroke, achieving this blood pressure goal probably reduces cardiovascular disease, although we do not know with certainty whether the incidence of heart failure is also decreased.
Differences Between Antihypertensive Medications
The choice of an antihypertensive agent obviously depends on the drug’s ability to reduce overall cardiovascular risk, so choosing an agent because it is best at reducing heart failure risk would make no sense if it is not equally beneficial with respect to other endpoints. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) found that patients treated with the diuretic chlorthalidone, the dihydropyridine CCB amlodipine, and the ACE inhibitor lisinopril had similar rates of cardiovascular events and cardiovascular deaths (54). Meta-analyses have generally reached similar conclusions and other indirect evidence suggests there is a linear relationship between blood pressure reduction and the reduction in cardiovascular events for the most commonly used antihypertensive medications.
Since antihypertensive agents generally result in equivalent rates of cardiovascular events, the antihypertensive drug class that is more successful at preventing heart failure should be preferred over others because of the importance of heart failure as a public health problem. In the ALLHAT study, the 6-year rate of developing heart failure was lowest among patients treated with chlorthalidone (7.7%), intermediate among those treated with lisinopril (8.7%), and highest among those treated with amlodipine (10.2%, p <0.001 for amlodipine and lisinopril compared to chlorthalidone) (54). One meta-analysis that excluded ALLHAT found diuretics to be superior to CCBs for preventing heart failure, but diuretics were not found to be superior compared to ACE inhibitors (39), although other studies have reached different conclusions (55).
β-blockers and adrenergic receptor binders (ARBs) were not included in ALLHAT, so we know much less about these agents. However, a United Kingdom Prospective Diabetes Study (UKPDS) found similar rates of heart failure between the ACE inhibitor captopril and the β-blocker atenolol (56), and the LIFE study found similar rates of heart failure between patients treated with atenolol and the ARB losartan (57). Thus, β-blockers and ARBs are likely to be as beneficial as ACE inhibitors, although their equivalence to diuretics has not been studied.
The ALLHAT trial is the only large, comparative trial of antihypertensive medications that randomized patients to primary treatment with a peripheral α-blocker. The α-blocker arm of the study was terminated early because, compared to treatment with the diuretic cholorthalidone, the group assigned doxazosin had a doubling in heart failure risk as well as a higher risk of stroke (19% increased risk) and combined cardiovascular disease events (25% increased risk) (58). The twofold difference in heart failure observed with doxazosin is comparable in magnitude to the difference seen in early hypertension trials comparing diuretic or β-blocker treatment with placebo. The higher rate of heart failure in the doxazosin group occurred despite only a small blood pressure difference between the diuretic and α-blocker groups (systolic blood pressure 3 mm Hg higher for the doxazosin group). This evidence suggests that blood pressure lowering with a peripheral α-blocker probably has no benefit in reducing heart failure, which is consistent with the results of the VA Cooperative Heart Failure Trial that found the α-blocker prazosin was no more effective than placebo in the treatment of patients with established heart failure (59).
Although debate continues to rage on the optimal firstline antihypertensive, the available evidence suggests that expanding use of thiazide-type diuretics for the treatment of hypertension will help reduce the incidence of heart failure. It is unknown whether diuretics are actually superior at altering the underlying disease processes that lead to ventricular injury and dysfunction, or whether diuretics simply control symptoms of heart failure among patients with early disease. Chlorthalidone and other thiazide-type diuretics appear to achieve similar outcomes for cardiovascular events and mortality but there are no data available for comparative rates of heart failure (60). ACE inhibitors, ARBs, and β-blockers may be somewhat less effective than diuretics, and CCBs and α-blockers are clearly inferior. However, the majority of patients will require more than one drug for blood pressure control, and the optimal therapeutic regimen to prevent heart failure for an individual patient is likely to be the one that lowers blood pressure the most with the least side effects.
Prevention of Heart Failure Among Patients with Left Ventricular Hypertrophy
Poorly controlled hypertension can eventually lead to LVH, a form of asymptomatic left ventricular dysfunction (Stage B, Fig. 30-1). LVH can ultimately cause symptomatic heart failure due to diastolic dysfunction from poor ventricular compliance (Stage C, Fig. 30-1). When present, LVH portends a worse cardiovascular prognosis overall and an increased risk of heart failure (13). Strict control of hypertension is, therefore, extremely important for individuals with LVH. Reduction of left ventricular mass has been observed in patients receiving antihypertensive drug treatment (except for the direct vasodilators) (61,62), and the declining prevalence of severe hypertension and LVH corresponds well with increased use of antihypertensive medications (63). Lifestyle modifications to promote weight loss, reduce salt intake, and increase physical activity also reduce LV mass (64). Furthermore, the regression or lack of development of LVH while taking antihypertensive therapy is a favorable prognostic sign (65,66). There is, however, insufficient clinical evidence to warrant using an individual patient’s change in LV mass to guide therapeutic decision making.
It is uncertain whether some antihypertensive medications are better than others for preventing heart failure among patients with LVH. There are theoretical reasons to choose drugs that block the renin-angiotensin-aldosterone system (RAAS) since these agents may have neurohumoral antihypertrophic effects on LV mass that are independent of blood pressure lowering. However, the Treatment of Mild Hypertension Study (TOMHS) does not support this hypothesis. In this trial, individuals with mild hypertension were randomized to placebo, acebutolol, amlodipine, chlorthalidone, doxazosin, or enalapril. All patients received a lifestyle intervention to promote increased physical activity, reduction in salt intake, and weight loss. After 1 year, the groups assigned the thiazide diuretic and the CCB had significantly greater reductions in LV mass than the β-blocker, ACE inhibitor, α-blocker, and placebo groups (64). A meta-analysis of predominantly small studies that excluded TOMHS suggested that LV mass was reduced to a greater extent in patients treated with CCBs, ACE inhibitors, and ARBs compared to β-blockers. Diuretics did not significantly differ from any of the other medication classes (61). In the Losartan Intervention for Endpoint Reduction in Hypertension Study, a large trial in which all participants had LVH by electrocardiogram (ECG) criteria, the ARB losartan reduced LVH more than atenolol and major cardiovascular events were also reduced (57,67). Notably, incident heart failure was similar in both groups. One explanation for this finding is that atenolol slows the heart rate and allows more time in diastole for filling. Thus, even though atenolol had a less-beneficial effect on LVH regression, its other cardiac and neurohormonal effects may have helped prevent heart failure through other pathways, ultimately resulting in equal benefits compared to losartan.
We believe that the debate about which single drug is best for promoting regression of LVH and preventing heart failure is misguided because it directs our attention away from the central clinical problem. Most patients with LVH have blood pressure that is hard to control and will require multiple medications. The main goal for patients with LVH should be to reduce the blood pressure to recommended targets (i.e., <140/90 mm Hg) with whatever combination of medications is effective, tolerated, and affordable for a given patient. We are unaware of any studies that have compared different combinations of drugs to see which are most effective at reducing incident heart failure. Based on
the limited amount of data previously described, a reasonable approach would be to start with a combination of a thiazide-type diuretic and either an ACE inhibitor or an ARB and then add a β-blocker or a CCB as needed to reach the appropriate blood pressure target.
the limited amount of data previously described, a reasonable approach would be to start with a combination of a thiazide-type diuretic and either an ACE inhibitor or an ARB and then add a β-blocker or a CCB as needed to reach the appropriate blood pressure target.
Prevention Strategies for Patients with Coronary Artery Disease
Ischemic heart disease and myocardial infarction are the predominant causes of heart failure due to left ventricular systolic dysfunction (68). Each year in the United States approximately 1.2 million people are hospitalized with a first (700,000) or recurrent (500,000) infarction (69), and many more have silent myocardial infarctions (1). Approximately 14% of people who suffer a heart attack will develop heart failure over the 5 years after their infarction, and the incidence rises to 22% after 10 years (70). Preventing coronary disease and myocardial infarction is obviously a critical goal if we are to reduce the incidence of heart failure. Although in many cases evidence from randomized, controlled trials is lacking, interventions that successfully reduce the overall risk of CAD and myocardial infarction are all likely to reduce the incidence of heart failure.
This section discusses the importance of treatment of hypercholesterolemia and the use of ACE inhibitors to prevent heart failure. Another important concern for patients with CAD is asymptomatic left ventricular systolic dysfunction (ALVSD). Patients with this condition are at risk for progressive ventricular remodeling and development of heart failure. Because ALVSD is not unique to patients with CAD, treatment of this condition is discussed in the following section.
Treatment of Hypercholesterolemia
Control of hyperlipidemia prevents CAD and myocardial infarction (MI) and in some studies has been proven to reduce the incidence of heart failure. Cholesterol-lowering therapy with a statin in patients with CAD, in addition to the beneficial effects on other cardiovascular events and mortality, has been proven to reduce incident heart failure by 20% in the Scandinavian Simvasatin Survival Study (absolute risk reduction 2% over 5 years) (71). In the A to Z Trial, performed in patients with acute coronary syndromes, high-intensity statin therapy was associated with a 28% reduction in heart failure compared with lower-intensity statin therapy (1.3% absolute risk reduction over 2 years) (72). Reduction in heart failure is not limited to treatment with statins. Use of gemfibrozil in the Veterans’ Affairs Cooperative Studies Program High-Density Lipoprotein Cholesterol Intervention Trial reduced the rate of heart failure hospitalization in men with CAD by 22% (2.7% absolute risk reduction over 5.1 years) (73). Several other lipid-lowering medication studies did not show a significant reduction in heart failure events or did not report heart failure as an outcome. However, these reports very likely underestimate the impact of treating hyperlipidemia on heart failure. Since the primary mechanism by which lipid-lowering agents reduce the incidence of heart failure is by reducing the rate of myocardial infarction, demonstration of a significant reduction in heart failure with lipid-lowering drugs may require larger studies with longer follow-up than what is needed to detect reductions in cardiovascular events.
Renin-Angiotensin System Blockade and Reducing Blood Pressure
Patients with established atherosclerotic disease are at increased risk for the development of heart failure. The effects of ACE inhibitors have been tested in patients at high risk of heart failure due to pre-existing cardiovascular disease who had minimal or no elevation in blood pressure. Three large, placebo-controlled trials of ACE inhibitors enrolled predominantly patients with stable CAD without evidence of heart failure (Table 30-2) (74,75,76). Mean baseline blood pressures for these three
trials were 139/79 mm Hg in the Heart Outcomes Prevention Evaluation Study (HOPE), 137/82 mm Hg in the European Trial on Reduction of Cardiac Events with Perindopril in Patients with Stable Coronary Artery Disease (EUROPA) and 133/78 mm Hg in the Prevention of Events with Angiotensin-Converting Enzyme Inhibition Trial (PEACE). Thus, the majority of patients had systolic blood pressure below the recommended target of 140 mm Hg. In these trials, systolic blood pressure was reduced by 3 to 5 mm Hg in the ACE inhibitor groups compared to controls receiving placebo.
trials were 139/79 mm Hg in the Heart Outcomes Prevention Evaluation Study (HOPE), 137/82 mm Hg in the European Trial on Reduction of Cardiac Events with Perindopril in Patients with Stable Coronary Artery Disease (EUROPA) and 133/78 mm Hg in the Prevention of Events with Angiotensin-Converting Enzyme Inhibition Trial (PEACE). Thus, the majority of patients had systolic blood pressure below the recommended target of 140 mm Hg. In these trials, systolic blood pressure was reduced by 3 to 5 mm Hg in the ACE inhibitor groups compared to controls receiving placebo.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree