Patients with drug-induced type 1 Brugada electrocardiograms (BrECGs) are considered to have good prognosis. Spontaneous type 1 is, instead, considered a risk factor; however, it is probably underestimated because of the BrECG fluctuations. The aim of this study was to analyze, in a large population of patients with Br, the real prevalence of type 1 BrECG using 12-lead 24-hour Holter monitoring (12L-Holter) and its correlation with the time of the day. We recorded 303 12L-Holter in 251 patients. Seventy-five (30%) patients exhibited spontaneous type 1 BrECG at 12-lead ECG (group 1) and 176 (70%) had only drug-induced type 1 (group 2). Type 1 BrECG was defined as “persistent” (>85% of the recording), “intermittent” (<85%), or “absent.” In group 1, 12% showed persistent type 1 at 12L-Holter, 57% intermittent type 1%, and 31% never had type 1; in group 2, none had persistent type 1, 20% had intermittent type 1%, and 80% never showed type 1. To evaluate the circadian fluctuations of BrECG, 4 periods in the day were considered. Type 1 BrECG was more frequent between 12-noon and 6 p.m. (52%, p <0.001). In conclusion, in patients with drug-induced type 1, spontaneous type 1 BrECG can be detected more frequently with 12L-Holter than with conventional follow-up with periodic ECGs and this has important implications in the risk stratification. 12L-Holter recording might avoid 20% of the pharmacological challenges with sodium channel blockers, which are not without risks, and should thus be considered as the first screening test, particularly in children or in presence of borderline diagnostic basal ECG.
Brugada (Br) syndrome is an inherited arrhythmogenic disorder characterized by ST-segment elevation in the right precordial leads and an increased risk of sudden death due to ventricular fibrillation, mostly in young and otherwise healthy adults. There are 2 electrocardiographic patterns: type 1, that is, coved ST-segment elevation ≥2 mm, followed by a negative T wave in at least 1 right precordial lead and type 2, saddle-back ST elevation. Type 1 is diagnostic, whereas in type 2, drug test with sodium channel blockers is needed to confirm the diagnosis. The authors agree in considering spontaneous type 1 electrocardiographic pattern (Br electrocardiogram [BrECG]) as a risk factor. It is, however, likely that type 1 BrECG is underestimated by recording only sporadic 12-lead ECGs, due to the well-known Br electrocardiographic fluctuations. For this reason, aim of this study was to analyze, in a large population of patients with Br, the prevalence of type-1 BrECG using 12-lead 24-hour Holter monitoring (12L-Holter) and the correlation of type 1 BrECG with the time of the day.
Methods
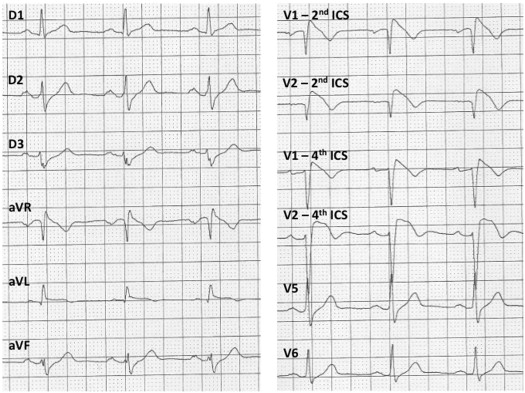
Of 684 patients included in the Brugada Registry of the Piedmont region of Italy from 2001 to 2013, we considered in this study 251 patients who underwent 12L-Holter at least once during the follow-up, starting from 2008. All the patients gave their informed consent to the inclusion in the registry. Type 1 Br pattern at baseline ECG was defined as coved-type ST-segment elevation ≥0.2 mV, followed by a negative T wave in at least 1 right precordial lead, including recordings from the second or third intercostal space (ICS). This typical electrocardiographic pattern could be recorded either spontaneously or after Class 1 antiarrhythmic drug challenge (intravenous ajmaline 1 mg/kg in 5 minutes or flecainide 2 mg/kg in 10 minutes). The pharmacological test was performed in patients presenting with a saddle-back ST elevation in V1-V2 recorded in the standard position or in the second ICS or in the presence of a rounded, wide r’ wave in V1 andV2 and a QRS duration longer in the right precordial leads than in V6. All the patients signed an informed consent before undergoing the test. Two groups were considered. Group 1 consisted in patients with spontaneous type 1 BrECG before the 12L-Holter. Group 2 included patients with only drug-induced type 1 BrECG before the 12L-Holter. Patients were classified as symptomatic if they had a history of aborted sudden death or syncope, otherwise they were considered asymptomatic.
In all patients, 12L-Holter was recorded in the right precordial leads both at the fourth and the second ICS during 24-hour periods of ordinary daily life (recording systems: Mortara H12+ High Fidelity [Mortara Instrument Europe S.r.l., Casalecchio di Reno, Bologna, Italy] and Esaote Lifecard CF 12 [Esaote S.p.A., Firenze, Italy] Holter recorders). V1 and V2 electrodes were attached in the second ICS, V3 and V4 electrodes in the fourth ICS (on the right and left parasternal line), and V5 and V6 in the fifth ICS in their standard position. Before the examination, we recorded a fourth and a second ICS strip during standing and supine positions to evaluate changes in ST-segment morphology related to the position. All 12L-Holter were analyzed independently by 2 cardiologists. The type 1 pattern was searched scrolling the 12L-Holter traces from the beginning to the end.
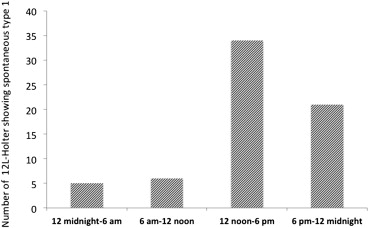
Type 1 Br pattern on 12L-Holter was defined as for 12-lead ECG ( Figure 1 ). The Br electrocardiographic burden was arbitrarily defined as follows: “persistent,” when the type 1 BrECG was present for >85% of the 24-hour Holter recording, “intermittent,” corresponding to a type 1 burden <85% of the recording, “absent,” when type 1 was never recorded. To evaluate the circadian fluctuations of the Br electrocardiographic pattern, we divided the day into 4 periods: 12 midnight to 6 a.m. , 6 a.m. to 12 noon, 12 noon to 6 p.m. , and 6 p.m. to 12 midnight. The presence of spontaneous type 1 BrECG on 12L-Holter was compared between symptomatic and asymptomatic patients. Moreover, the correlation with arrhythmic events at follow-up was searched. Arrhythmic events during follow-up were defined as documented sustained (>30 seconds) ventricular arrhythmias or appropriate implantable cardioverter defibrillator shock.
Continuous variables are presented as mean ± SD. Comparisons between groups were performed using the chi-square test (maximum-likelihood chi-square test) for qualitative variables. Comparisons of quantitative variables were carried out with Student t test and nonparametric Mann-Whitney test for 2 distributions. All probability values were 2-sided, with p <0.05 considered significant. Analyses were performed using SPSS 20 (IBM, Armonk, New York).
Results
Three hundred and three 12L-Holter were recorded in 251 patients with Br. Mean age was 46 ± 15 years, 72% of the patients were men. Seventy-five patients (30%) exhibited spontaneous type 1 BrECG at basal ECG (group 1); of these, 11 (15%) had previous syncope and 1 aborted sudden death, and the remaining were asymptomatic. One hundred seventy-six subjects (70%) had drug-induced type 1 (group 2); 21 (12%) were symptomatic for syncope, and the remaining 154 (88%) were asymptomatic.
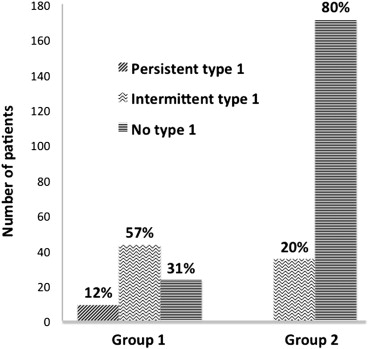
In group 1, 52 (69%) of 75 patients showed type 1 at 12L-Holter, 43 (57%) had intermittent type 1, 9 (12%) had persistent type 1, and 23 (31%) never had type 1 at 12L-Holter ( Figure 2 ). In this latter group, there were 6 patients in whom the type 1 Br pattern at basal ECG had been documented only during fever. In group 2, 35 (20%) of 176 patients developed intermittent type 1 BrECG at 12L-Holter, and in the remaining 80%, type 1 BrECG was never recorded ( Figure 2 ). One patient showed type 1 BrECG both at basal ECG and at 12L-Holter during antidepressant therapy with mirtazapine; he did not show anymore the diagnostic pattern after discontinuation of the therapy. Forty-five (18%) 12L-Holter were recorded in subjects with family history of BrECG. Thirty-seven (82%) belonged to group 2 and 6 (16%) of them exhibited type 1 at 12L-Holter. Type 1 BrECG on 12L-Holter was present in 12 of 33 symptomatic patients (33%) and in 75 of 218 asymptomatic patients (34%; p = NS).
Type 1 BrECG was most frequently recorded from 12 noon to 6 p.m. (52%), followed by 6 p.m. to 12 midnight (32%), 6 a.m. to 12 noon (9%), and 12 midnight to 6 a.m. (7%, p <0.001; Figure 3 ). Mean heart rate was respectively 90 ± 8 beats/min, 82 ± 11 beats/min, 63 ± 13 beats/min, and 69 ± 7 beats/min. Mean heart rate was significantly lower from 12 midnight to 6 a.m. than in the other periods (p <0.001). Thirty-eight subjects had 2 or more 12L-Holter (mean 1.2 Holter per patient); between one 12L-Holter and the other, about 12 months elapsed. The repeated recording allowed identifying the type 1 pattern in other 3 out of 20 subjects (15%) with drug-induced type 1 BrECG, who were negative at the first monitoring.
At a mean follow-up of 38 ± 26 months, no patient had arrhythmic events.
Results
Three hundred and three 12L-Holter were recorded in 251 patients with Br. Mean age was 46 ± 15 years, 72% of the patients were men. Seventy-five patients (30%) exhibited spontaneous type 1 BrECG at basal ECG (group 1); of these, 11 (15%) had previous syncope and 1 aborted sudden death, and the remaining were asymptomatic. One hundred seventy-six subjects (70%) had drug-induced type 1 (group 2); 21 (12%) were symptomatic for syncope, and the remaining 154 (88%) were asymptomatic.
In group 1, 52 (69%) of 75 patients showed type 1 at 12L-Holter, 43 (57%) had intermittent type 1, 9 (12%) had persistent type 1, and 23 (31%) never had type 1 at 12L-Holter ( Figure 2 ). In this latter group, there were 6 patients in whom the type 1 Br pattern at basal ECG had been documented only during fever. In group 2, 35 (20%) of 176 patients developed intermittent type 1 BrECG at 12L-Holter, and in the remaining 80%, type 1 BrECG was never recorded ( Figure 2 ). One patient showed type 1 BrECG both at basal ECG and at 12L-Holter during antidepressant therapy with mirtazapine; he did not show anymore the diagnostic pattern after discontinuation of the therapy. Forty-five (18%) 12L-Holter were recorded in subjects with family history of BrECG. Thirty-seven (82%) belonged to group 2 and 6 (16%) of them exhibited type 1 at 12L-Holter. Type 1 BrECG on 12L-Holter was present in 12 of 33 symptomatic patients (33%) and in 75 of 218 asymptomatic patients (34%; p = NS).




