Atrial fibrillation (AF) can be the first manifestation of latent Brugada syndrome (BS). The aim of our study was to assess the prevalence of AF as the first clinical diagnosis in patients with BS and their demographic and clinical characteristics and diagnosis management in a large cohort of patients. The patient group consisted of 611 patients with BS. The data from those with a diagnosis of AF previous to the identification of BS were analyzed (n = 35). Eleven cases were unmasked after the initiation of a class I antiarrhythmic drug and one during the establishment of general anesthesia. In the remaining population, BS was diagnosed using an ajmaline test performed mainly because of younger age in patients with lone AF (n = 13), previous syncope or sudden cardiac death (n = 3), or a clinical history of sudden cardiac death in the family (n = 5). The mean patient age was 49 ± 15 years, 21 were male patients, 14 had a family history of sudden death, 15 had had previous syncope, and 4 had survived cardiac arrest. Concomitant electrical disorder was found in 13 patients. Remarkably, 21 patients had normal findings on the baseline electrocardiogram. In conclusion, AF could be one of the first clinical manifestations of latent BS in a considerable number of patients. This identification is crucial because the treatment of these patients is subject to relevant changes. The ajmaline test plays an essential role, mainly in young patients with a family history of sudden death, despite having normal findings on a baseline electrocardiogram.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, occurring in 1% to 2% of the general population. The main risk factors for the development of AF are arterial hypertension and structural heart disease. Nevertheless, ≤30% of patients with AF can have “lone AF,” which can be, in certain cases, of hereditary origin. Accordingly, during previous years, numerous inherited cardiac syndromes associated with AF have been identified, including Brugada syndrome (BS). Moreover, AF can even be the first manifestation of latent BS. This has crucial importance in terms of medical management, in particular, because of the contraindication for a series of antiarrhythmic and other drugs. The aim of our study was to assess the prevalence of the diagnosis of AF previous to the identification of BS in a large cohort of patients. We also reviewed their demographic and clinical characteristics.
Methods
A total of 611 patients with the BS were included in our database from 1995 to 2011. Of these, we analyzed the data from those who had documented AF (defined as ≥1 documented episode of paroxysmal AF lasting >30 seconds) previous to the diagnosis of BS. Lone AF was defined as AF occurring in the absence of structural heart disease, a history of hypertension, and/or left ventricular hypertrophy, as determined by physical examination, electrocardiography, chest radiography, and echocardiography. The diagnosis of BS was determined using the recommendations of the Brugada consensus reports, with recent modifications. Accordingly, in the assessment of a potential conversion to a typical type 1 Brugada electrocardiographic pattern, patients with types 2 and 3 Brugada electrocardiographic patterns underwent pharmacologic testing with intravenous ajmaline at a dose of 1 mg/kg body weight as a continuous infusion within 5 minutes. The test was performed with continuous electrocardiographic recording, and, after administration of the last dose, the electrocardiographic recording was continued for another 10 minutes. The ajmaline test findings were considered positive if a normal or type 2 or 3 electrocardiographic pattern converted to a coved-type electrocardiographic pattern with an ST-segment elevation of >0.2 mV in ≥1 right precordial lead, including recordings from the third intercostal space. The PR, QRS, and QTc intervals were measured before and after the test in all patients.
The occurrence of sudden cardiac death (SCD) in the family was categorized as follows: <35, 35 to 55, and 56 to 65 years old. An electrophysiologic study was performed in asymptomatic patients to perform risk stratification and in the symptomatic patients (those with syncope, previous cardiac arrest, or documented ventricular tachycardia/ventricular fibrillation) for the assessment of eventually inducible supraventricular arrhythmias.
Descriptive data are reported as frequencies, mean ± SD, or medians, as appropriate. For between group comparisons, 2-sided t tests for independent samples for continuous variables and chi-square tests for binary variables were used. All statistics were computed using SPSS software (SPSS, Chicago, Illinois). All probability values were 2-sided, with p <0.05 considered significant.
Results
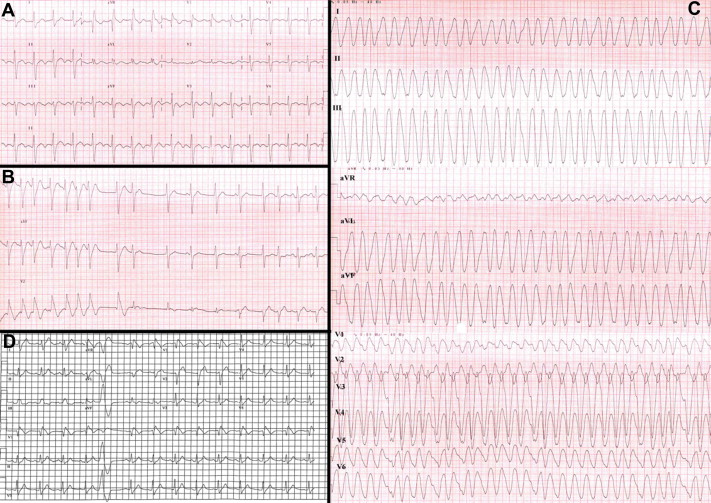
Of the 611 patients with the BS, 35 had AF documented before the diagnosis of BS. The mean age was 49 ± 15 years, and 21 were male and 14 were female patients ( Table 1 ). In 12 patients, the diagnostic workup started after observation of suggestive pharmacologically induced electrocardiographic changes (11 patients after class IC antiarrhythmic drug [AAD] administration and 1 during establishment of general anesthesia; Table 2 ). The first patient presented with aborted SCD 1 month after the initiation of propafenone, which had been prescribed for rhythm control of paroxysmal AF (patient 29). The second patient, a previously reported 22-year-old woman, was admitted to the emergency department with typical atrial flutter and developed Brugada-like electrocardiographic changes after conversion to sinus rhythm with flecainide infusion and, subsequently, a degeneration in ventricular fibrillation ( Figure 1 ). Of these 12 patients, 5 had a family history of sudden death and 4 had reported previous syncope. All these patients were later diagnosed with BS using the ajmaline test.
| Previous AF | p Value | ||
|---|---|---|---|
| Yes (n = 35) | No (n = 576) | ||
| Age (yrs) | 49 (15) | 44 (17) | NS |
| Gender | NS | ||
| Male | 63% | 68% | |
| Female | 37% | 32% | |
| Syncope | 38% | 19% | 0.01 |
| Sudden cardiac death | 8% | 3% | NS |
| Baseline electrocardiographic pattern | |||
| Type 1 | 20% | 22% | NS |
| Type 2 | 11% | 13% | NS |
| Type 3 | 9% | 6% | NS |
| Family history of sudden cardiac death | 40% | 46% | NS |
| First-degree | 26% | 27% | NS |
| Second-degree | 21% | 30% | NS |
| Third-degree | 0% | 17% | NS |
| PR interval (ms) | 183 ± 37 | 179 ± 34 | NS |
| QRS interval (ms) | 108 ± 24 | 95 ± 20 | 0.01 |
| QTc interval (ms) | 414.48 ± 32 | 405 ± 35 | NS |
| HV interval (ms) | 48 ± 10 | 45.96 ± 10 | NS |
| Implantable cardioverter-defibrillator implantation | 43.24% | 23.61% | NS |
| Pt. No. | Age | Gender | Family History of SCD | Syncope | SCD | ED | HV Interval | ECG Pattern |
|---|---|---|---|---|---|---|---|---|
| 1 | 22 | Male | 1, First-degree | Yes | Yes | SSS | — | Type 1 |
| 2 | 25 | Male | No | Yes | No | No | 50 | Type 1 |
| 3 | 32 | Male | No | No | No | No | 40 | Type 1 |
| 4 | 33 | Male | 1, Second-degree (<35 yrs) | No | No | No | 50 | Type 3 |
| 5 | 39 | Male | 1 Second-degree (35–55 yrs) | Yes | Yes | No | — | Type 1 |
| 6 | 49 | Male | No | No | No | No | 45 | Type 3 |
| 7 | 51 | Female | 1, Second-degree (55–65 yrs) | No | No | SSS (PCM) | 65 | Type 1 |
| 8 | 51 | Male | No | No | No | No | 35 | Type 2 |
| 9 | 56 | Female | 1, First-degree (56–65 y); 2, second-degree (56–65 yrs) | Yes | No | AVNRT | — | Type 2 |
| 10 | 57 | Female | 1, First-degree (55–65 yrs) | No | No | No | 35 | Type 2 |
| 11 | 58 | Female | 2, First-degree (56–65 yrs) | Yes | No | No | 40 | Type 1 |
| 12 | 58 | Male | No | No | No | No | — | Type 2 |
| 13 | 58 | Female | 2, First-degree (<35 yrs) | Yes | No | No | 40 | Type 1 |
| 14 | 71 | Female | No | Yes | No | SSS | 50 | Type 2 |
| 15 | 89 | Female | No | No | No | No | — | Type 1 |
In the remaining patients, the diagnosis of BS was also by ajmaline challenge. The reasons for testing for BS were as follows: 13 were young patients with lone AF (4 of whom had a family history of sudden death and 1 young male patient who had presented with previous syncope). One of these patients was an 11-year-old girl with short episodes of AF and syncope and one was a 56-year-old woman with polymorphic ventricular tachycardia on the Holter electrocardiogram (patient 16 and 28, respectively). Five patients with a previous diagnosis of AF were seen in our hospital because of a family history of BS. Three of them reported a history of previous syncope and the two had experienced aborted SCD. Finally, 2 patients were seen in consultation because of syncope, 1 patient underwent an ajmaline challenge test because of 1 episode of SCD (baseline type 2 electrocardiographic Brugada pattern), and 2 patients were referred to our institution because of a type 1 pattern on the baseline electrocardiogram.
A concomitant other electrical disorder was found in 13 patients: 6 with sinus node dysfunction, 4 with right atrial flutter, 2 with first-degree atrioventricular block, 1 with atrioventricular reentrant tachycardia, and 1 with atrioventricular nodal reentrant tachycardia. The mean HV interval was 48 ± 10 ms; however, 5 patients showed a baseline HV interval of ≥60 ms. The baseline electrocardiogram showed a type 1 electrocardiographic Brugada pattern in 7 patients, type 2 in 4, and type 3 in 3; 21 patients had normal findings on the baseline electrocardiogram ( Table 3 ). In addition, 1 of the patients presented with AF on the baseline electrocardiogram (patient 11); 1 patient exhibited a J-wave in ≥2 inferior leads (patient 16) and 3 in the lateral leads (I and aVL; patients 7, 10, and 34). After the test, an increase occurred in the PR interval (from 179 to 216.25 ms; p = 0.07), QRS (from 106 to 140.35 ms; p = 0.05), and QT interval (from 396 to 465.27 ms; p = 0.001). In addition, where meaningful, our study population was compared to patients from our in-hospital database with the diagnosis of BS without any documented AF as the first clinical manifestation with regard to the studied parameters ( Table 1 ). Patients with AF as a first clinical manifestation had a greater frequency of previous syncope (37.8% vs 19.4%, p <0.01) and, although not significant, showed a trend a greater number of implantable cardioverter-defibrillator implantations compared to patients without AF before the BS diagnosis (43.2% vs 23.6%, p = 0.07).
| Pt. No. | Age | Gender | Family History of SCD | Syncope | Aborted SCD | ED | HV | ECG |
|---|---|---|---|---|---|---|---|---|
| 16 | 11 | Male | No | Yes | No | SSS | 70 | Normal |
| 17 | 22 | Female | No | Yes | Yes | No | 40 | Normal |
| 18 | 38 | Male | No | No | No | Normal | Normal | |
| 19 | 39 | Male | No | No | No | AVRT | 45 | Normal |
| 20 | 42 | Female | No | No | No | No | Normal | |
| 21 | 42 | Male | 2, First-degree (1 aged <35 yrs; 1 aged 35–55 yrs); 2, second-degree (1 aged <35 and 1 aged 56–65 yrs) | No | No | No | 60 | Normal |
| 22 | 43 | Male | No | No | No | No | 55 | Normal |
| 23 | 52 | Female | No | No | No | No | 35 | Normal |
| 24 | 53 | Male | No | No | No | First-degree AVB | 55 | Normal |
| 25 | 54 | Female | No | Yes | No | SSS; atrial flutter | 49 | Normal |
| 26 | 55 | Male | 1, First-degree (35– 55 yrs) | Yes | No | Atrial flutter | 60 | Normal |
| 27 | 56 | Male | 1, First-degree (56–65 yrs); 2, second-degree (55–65 yrs) | Yes | No | No | Normal | |
| 28 | 56 | Male | No | No | No | No | 50 | Normal |
| 29 | 58 | Female | No | No | No | No | 45 | Normal |
| 30 | 59 | Male | 2, First-degree (1 aged <35 yrs; 1 aged 56–65 yrs) | No | Yes | No | 40 | Normal |
| 31 | 60 | Male | No | No | No | First-degree AVB; atrial flutter | 40 | Normal |
| 32 | 61 | Female | No | Yes | No | Atrial flutter | 40 | Normal |
| 33 | 62 | Male | No | No | No | RBBB | 40 | Normal |
| 34 | 62 | Female | 1, Second-degree (33–55 yrs) | Yes | No | SSS | 63 | Normal |
| 35 | 74 | Male | 1, First-degree (35–55 yrs) | Yes | No | No | 50 | Normal |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


