Although bicuspid aortic valve occurs in an estimated 1% of adults and mitral valve prolapse in an estimated 5% of adults, occurrence of the 2 in the same patient is infrequent. During examination of operatively excised aortic and mitral valves because of dysfunction (stenosis and/or regurgitation), we encountered 16 patients who had congenitally bicuspid aortic valves associated with various types of dysfunctioning mitral valves. Eleven of the 16 patients had aortic stenosis (AS): 5 of them also had mitral stenosis, of rheumatic origin in 4 and secondary to mitral annular calcium in 1; the other 6 with aortic stenosis had pure mitral regurgitation (MR) secondary to mitral valve prolapse in 3, to ischemia in 2, and to unclear origin in 1. Of the 5 patients with pure aortic regurgitation, each also had pure mitral regurgitation: in 1 secondary to mitral valve prolapse and in 4 secondary to infective endocarditis. In conclusion, various types of mitral dysfunction severe enough to warrant mitral valve replacement occur in patients with bicuspid aortic valves. A proper search for mitral valve dysfunction in patients with bicuspid aortic valves appears warranted.
In 1994 Fernicola and Roberts described morphologic features of operatively excised aortic and mitral valves in 12 patients who had undergone combined aortic and mitral valve replacement for dysfunctioning congenitally bicuspid aortic valves (aortic stenosis [AS] in 8 and pure aortic regurgitation [AR] in 4) and dysfunctioning mitral valves (mitral regurgitation [MR] in 11 and congenital mitral stenosis [MS] in 1). The 12 patients (10%) were from 115 having combined mitral and aortic valve replacement. The present report examines at another institution 16 patients who had undergone combined aortic and mitral valve replacement for dysfunctioning congenitally bicuspid aortic valves and dysfunctioning mitral valves to demonstrate again the relative frequency of structural mitral disease in patients with dysfunctioning congenitally bicuspid aortic valves.
Methods
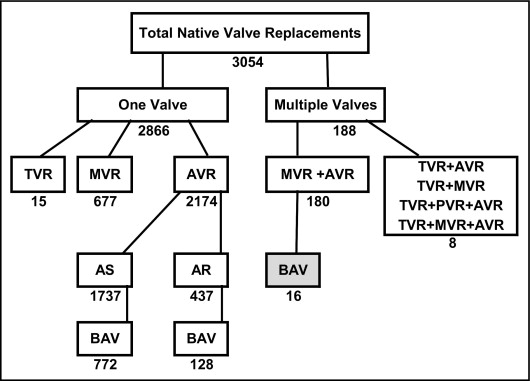
At Baylor University Medical Center (BUMC) at Dallas from March 3, 1993 to July 8, 2011, 3,054 native valve replacement operations were performed ( Figure 1 ). Of that number, 2866 (94%) involved a single valve (aortic in 2,174, mitral in 677, and tricuspid in 15) and 169 (6%) the replacement of >1 cardiac valve (mitral and aortic valves in 180 and tricuspid plus ≥1 other valve in 8). Of the 180 who had left-sided double valve replacements, 16 (9%) were in patients having a stenotic or purely regurgitant congenitally bicuspid aortic valve and a stenotic or purely regurgitant mitral valve. These 16 patients are the subject of this report. All 32 valves from these 16 patients were examined in the cardiovascular pathology laboratory of BUMC at Dallas, a part of the surgical pathology department, by 1 of us (W.C.R.). Photographs of the operatively excised valves were taken by 1 of us (J.M.K.). Histologic sections after the gross photographs were prepared from the valves that were the sites of infective endocarditis and from the mitral valves considered on gross examination to be characteristic of mitral valve prolapse. Stenotic valves were not studied histologically.
Medical records and available echocardiographic, hemodynamic, and angiographic reports were acquired on all 16 patients. Records of death were obtained from the Social Security Death Index. Intervals from the time of combined mitral and aortic valve replacement to June 30, 2011, were calculated.
Results
Pertinent findings in the 16 patients are presented in Tables 1 and 2 and illustrated in 13 patients in Figures 2 through 14 . Of the 16 patients, 12 were men age 24 to 77 (mean 57) and 4 were women age 53 to 84 (mean 67). Fifteen were white (94%) and 1 was Hispanic (6%, case 2).
| Case Number (figure number) | Age (years)/Sex | AVR to Discharge (days) | AVR to Death (days) | CABG | AS | AR | MS | MR | IE | RHD | IMR | MVP | MAC | Preoperative AF | BMI (kg/m 2 ) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (2) | 53/F | 5 | alive (5,264) | 0 | + | 0 | + | 0 | 0 | + | 0 | 0 | 0 | 0 | 34 |
| 2 | 50/M | 9 | 3,704 | + | + | 0 | + | 0 | 0 | + | 0 | 0 | 0 | 0 † | 27 |
| 3 (3) | 46/M | 4 | 2,534 | 0 ⁎ | + | 0 | + | 0 | 0 | + | 0 | 0 | 0 | + | 26 |
| 4 (4) | 74/F | 13 | 4,856 | 0 | + | 0 | + | 0 | 0 | + | 0 | 0 | 0 | + | 21 |
| 5 (5) | 71/M | 12 | alive (1,162) | + | + | 0 | + | 0 | 0 | 0 | 0 | 0 | + | 0 | 35 |
| 6 (6) | 84/F | 18 | 3,858 | + | + | 0 | 0 | + | 0 | 0 | + | 0 | 0 | 0 | 29 |
| 7 (7) | 77/M | 7 | 867 | + | + | 0 | 0 | + | 0 | 0 | + | 0 | 0 | 0 † | 22 |
| 8 (8) | 58/F | 6 | alive (1,301) | 0 | + | 0 | 0 | + | 0 | 0 | 0 | 0 | 0 | 0 | 42 |
| 9 (9) | 68/M | 6 | 1,540 | 0 | + | 0 | 0 | + | 0 | 0 | 0 | + | 0 | 0 | 23 |
| 10 (10) | 67/M | 6 | alive (1,267) | 0 | + | 0 | 0 | + | 0 | 0 | 0 | + | 0 | 0 † | 24 |
| 11 (11) | 66/M | 7 | 472 | 0 | + | 0 | 0 | + | 0 | 0 | 0 | + | 0 | 0 | 27 |
| 12 | 48/M | 56 | alive (6,096) | + | 0 | + | 0 | + | 0 | 0 | 0 | + | 0 | + | — |
| 13 (12) | 66/M | 6 | alive (1,252) | 0 | 0 | + | 0 | + | + | 0 | 0 | 0 | 0 | 0 | 23 |
| 14 (13) | 47/M | 5 | 674 | 0 | 0 | + | 0 | + | + | 0 | 0 | 0 | 0 | 0 | 36 |
| 15 | 24/M | 14 | alive (2,017) | 0 | 0 | + | 0 | + | + | 0 | 0 | 0 | 0 | 0 | 20 |
| 16 (14) | 50/M | 11 | alive (1,127) | 0 | 0 | + | 0 | + | + | 0 | 0 | 0 | 0 | 0 | 23 |
⁎ Previous resection of aortic isthmic coarctation.
† Developed atrial fibrillation postoperatively after double-valve replacement.
| Case Number (figure number) | Pressures (mm Hg) | AV Area (cm 2 ) | MV Area (cm 2 ) | MR (0–4+) | AR (0–4+) | EF (%) | AV Weight (g) | MV Weight (g) | Type (size [mm]) Substitute Valve | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LV (s/d) | Ao (s/d) | LV-Ao (psg) | LV-Ao (msg) | LV-MV (mdg) | RV (s/d) | RA (Mean) | PW (Mean) | AV | MV | ||||||||
| 1 (2) | — | — | — | — | — | — | — | — | 0.9 | 1.8 | — | — | — | — | — | P (20) | P (27) |
| 2 | 173/40 | 146/88 | 27 | 30 | 25 | 56/18 | 13 | 39 | 1.0 | 1.28 | 2+ | 1+ | 50 | — | — | P (21) | P (27) |
| 3 (3) | 139/17 | 133/88 | 6 | 54 | 15 | 48/18 | 13 | 26 | 0.46 | 0.95 | — | 2+ | 55 | 1.37 | 3.44 | P (23) | P (31) |
| 4 (4) | 226/19 | 195/85 | 31 | 129 | 14 | 79/17 | 54 | 33 | 0.53 | 0.95 | 0 | 2+ | 60 | — | — | P (21) | P (29) |
| 5 (5) | 159/27 | 140/65 | 19 | — | 6 | 57/21 | 20 | 22 | 1.1 | 2.33 | — | — | 20 | 2.54 | 3.70 | B (27) | B (29) |
| 6 (6) | 163/17 | 124/56 | 39 | 46 | 14 | 99/28 | 18 | 36 | 0.39 | — | — | 1+ | 70 | 0.90 | 1.00 | P (19) | P (25) |
| 7 (7) | 180/8 | 148/63 | 32 | 40 | — | — | — | — | 0.77 | — | 4+ | 2+ | 70 | 2.40 | 0.90 | P (25) | P (29) |
| 8 (8) | 234/ | 110/ | 124 | — | — | 44/17 | 12 | 18 | 0.5 | 1.0 | — | — | 60 | 2.39 | 0.40 | P (23) | P (27) |
| 9 (9) | 149/38 | 118/64 | 31 | 21 | — | 34/13 | 5 | 16 | — | — | 4+ | — | 60 | 2.81 | 4.66 | P (25) | P (33) |
| 10 (10) | 154/24 | 94/63 | 60 | 41 | — | 73/24 | 9 | 29 | 0.52 | — | 4+ | — | 20 | 5.86 | 0.52 | B (27) | B (29) |
| 11 (11) | — | 125/79 | — | — | — | 49/12 | 7 | 21 | — | — | 1+ | 4+ | — | 5.20 | 5.09 | P (24) | P (33) |
| 12 | 142/8 | 134/78 | 8 | — | — | 58/14 | — | — | — | — | 4+ | 2+ | 40 | — | — | P (—) | P (—) |
| 13 (12) | — | 130/60 ⁎ | — | — | — | — | — | — | — | — | 4+ | 4+ | — | 1.55 | 0.67 | P (25) | P (29) |
| 14 (13) | — | 116/61 | — | — | — | 28/11 | 6 | 8 | — | — | — | 3+ | 60 | 1.30 | 1.28 | P (25) | P (31) |
| 15 | — | 100/60 ⁎ | — | — | — | — | — | — | — | — | — | — | 60 | — | — | B (25) | B (29) |
| 16 (14) | — | 120/60 ⁎ | — | — | — | — | — | — | — | — | — | — | — | 1.02 | 2.01 | B (23) | B (31) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


