The present study examined the association between patient-reported anxiety and postcardiac surgery mortality and major morbidity. Frailty Assessment Before Cardiac Surgery was a prospective multicenter cohort study of elderly patients undergoing cardiac surgery (coronary artery bypass surgery and/or valve repair or replacement) at 4 tertiary care hospitals from 2008 to 2009. The patients were evaluated a mean of 2 days preoperatively with the Hospital Anxiety and Depression Scale, a validated questionnaire assessing depression and anxiety in hospitalized patients. The primary predictor variable was a high level of anxiety, defined by a Hospital Anxiety and Depression Scale score of ≥11. The main outcome measure was all-cause mortality or major morbidity (e.g., stroke, renal failure, prolonged ventilation, deep sternal wound infection, or reoperation) occurring during the index hospitalization. Multivariable logistic regression analysis examined the association between high preoperative anxiety and all-cause mortality/major morbidity, adjusting for the Society of Thoracic Surgeons predicted risk, age, gender, and depression symptoms. A total of 148 patients (mean age 75.8 ± 4.4 years; 34% women) completed the Hospital Anxiety and Depression Scale. High levels of preoperative anxiety were present in 7% of patients. No differences were found in the type of surgery and Society of Thoracic Surgeons predicted risk across the preoperative levels of anxiety. After adjusting for potential confounders, high preoperative anxiety was remained independently predictive of postoperative mortality or major morbidity (odds ratio 5.1, 95% confidence interval 1.3 to 20.2; p = 0.02). In conclusion, although high levels of anxiety were present in few patients anticipating cardiac surgery, this conferred a strong and independent heightened risk of mortality or major morbidity.
The importance of altered mood states in cardiovascular disease has been highlighted by several reports. With regard to surgical outcomes, depressive symptoms were evaluated in a cohort of patients undergoing coronary artery bypass graft surgery from 1989 to 1991, with Blumenthal et al discovering a significantly greater mortality among patients with preoperative depression. Despite the interrelation between the affective states of anxiety and depression, preoperative anxiety was not assessed. Prospective and simultaneous assessment of both anxiety and depression using a measure such as the Hospital Anxiety and Depression Scale (HADS) is necessary to understand and distinguish the role of these 2 affective states in postoperative outcomes. As such, we administered the HADS to measure anxiety and depression prospectively in hospitalized elderly patients awaiting coronary artery bypass grafting and/or valve repair or replacement.
Methods
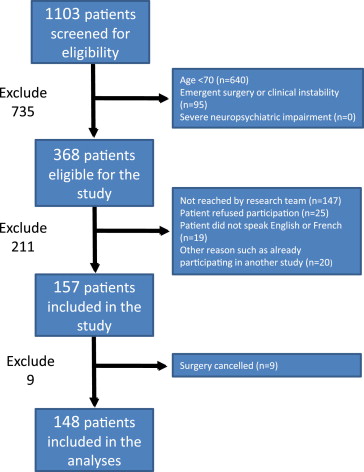
Consecutive patients were screened for study inclusion from 2008 to 2009 at 4 university-affiliated tertiary care centers in the United States and Canada as a part of the Frailty Assessment Before Cardiac Surgery (Frailty ABC’S) study. Eligible patients were asked by the study personnel to complete a structured questionnaire that included the HADS and a brief battery of physical performance tests. Mini-mental state examinations were also administered, and patients were asked to grade their overall health status. Frailty criteria were determined according to the Cardiovascular Health Study (CHS) scale.
The inclusion criteria were age ≥70 years and scheduled to undergo coronary artery bypass grafting and/or valve replacement or repair through a traditional midline sternotomy. The exclusion criteria included any of the following: emergent surgery, defined as surgery for ongoing refractory cardiac compromise for which there should be no delay; clinical instability, defined as active coronary ischemia, decompensated heart failure, or any acute process causing significant symptoms or abnormal vital signs; a severe neuropsychiatric condition causing inability to cooperate with the study procedures; or cancellation of the patient’s planned surgery. The treating physicians were unaware of the results of the HADS to not influence perioperative care.
The present report was prepared in keeping with the standards set forth by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement. The institutional review board at each enrolling center approved the study before proceeding with patient enrollment or any data acquisition. All patients provided written informed consent to participate in the present study.
The HADS is a brief, user-friendly, self-report questionnaire developed by Zigmond and Snaith in 1983 to assess the levels of anxiety and depression among patients in nonpsychiatric hospitals. This self-report scale can be administered to patients in approximately ≤5 minutes and can be scored in approximately 1 minute. The HADS has been repeatedly validated and shown to perform well as a screening tool in assessing the presence and symptom severity of both anxiety disorders and depression. The HADS has been translated into many languages, with validation studies confirming the international applicability of the questionnaire. In the present study, the HADS questionnaires were administered in English or French.
The HADS questionnaire consists of 14 items, 7 for each of 2 subscales: anxiety (HADS-A) and depression (HADS-D). Each item is rated from 0 to 3 on a 4-point Likert scale, resulting in a potential range of scores from 0 to 21 for each subscale. A score of ≥11 on either subscale is considered to indicate cases of “significant psychological morbidity.” Scores of 8 to 10 represent “possible anxiety” and 0 to 7 represent “no anxiety.” Designed for use in the inpatient setting, the individual HADS items are formulated as symptoms referring to the previous 7 days and do not include physical indexes of psychological distress, which might be expected to result in false-positive results among hospitalized patients. The key phrases from the questions including the HADS-A subscale are listed in Table 1 .
| Question | How often in the past week did you… ? |
|---|---|
| A1 | “feel tense or ‘wound up’” |
| A2 | “get a sort of frightened feeling as if something awful is about to happen” |
| A3 | “have worrying thoughts go through your mind” |
| A4 | “sit at ease and feel relaxed” |
| A5 | “get a sort of frightened feeling like ‘butterflies’ in the stomach” |
| A6 | “feel restless as if I have to be on the move” |
| A7 | “get sudden feelings of panic” |
∗ The complete HADS is available in the original 1983 report by Zigmond and Snaith.
The primary outcome measure was the incidence of mortality or major morbidity occurring after cardiac surgery during the index hospitalization. The Society of Thoracic Surgeons (STS) database definitions were used for all outcomes. The outcomes were death (defined as mortality from any cause), stroke (central neurologic deficit persisting >72 hours), renal failure (a new dialysis requirement or increase in serum creatinine >2 mg/dl and more than twofold greater than the preoperative level), prolonged ventilation (need for mechanical ventilation >24 hours), deep sternal wound infection, and reoperation for any reason. The secondary outcome measures were discharge to a healthcare facility for ongoing medical care or rehabilitation, and prolonged postoperative length of stay, defined by the STS standard of >14 days after surgery. The physicians ascertaining outcomes from the medical records were unaware of the results of the HADS questionnaire.
The demographic and operative characteristics were compared across the categories of HADS-A scores: 0 to 7 (no anxiety), 8 to 10 (possible anxiety), and ≥11 (anxiety). The categorical variables are presented as the percentages, and continuous variables are presented as the median and 25th and 75th percentiles. The comparisons of baseline variables were conducted using the nonparametric Wilcoxon rank sum test.
Multivariable analyses were performed with logistic regression modeling and reported as odds ratios (ORs), with 95% confidence intervals (CIs). Because the number of risk factors in patients undergoing cardiac surgery is large, entering all possible covariates in the model would have resulted in model instability and overfitting. Therefore, we used the STS predicted risk of mortality or major morbidity (STS-PROMM) as a risk score to adjust for the surgical risk associated with traditional medical factors. The STS-PROMM was selected among all available adult cardiac surgery risk scores, because this score was specifically designed to predict in-hospital mortality or major morbidity, the precise primary end point of the present study.
A sensitivity analysis using a nonparsimonious model adjusted for additional covariates was performed to ensure that significant confounding had not been overlooked. The performance of the model was assessed before and after addition of the HADS-A score to determine its incremental value. Model discrimination, reflecting the ability to assign a greater predicted risk to those who will have the observed outcome, was measured with the area under the receiver operating characteristic curve c-statistic. Sensitivity analyses, with the HADS-A score represented as a continuous variable, were also performed. All analyses were performed with STATA, version 11 (StataCorp, College Station, Texas).
Results
The cohort for these analyses consisted of 148 patients who completed the HADS questionnaire and underwent cardiac surgery within the Frailty ABC’S study. The median interval from questionnaire completion to surgery was 2 days (interquartile range 1 to 3). No patients were lost to follow-up. Figure 1 displays the flow of patients through the present study. The baseline variables stratified by HADS-A score are listed in Table 2 : 71% scored 0 to 7 (“no anxiety”); 22% scored 8 to 10 (“possible anxiety”); and 7% scored 11 to 21 (“anxiety” group). Age and gender were included individually, along with the STS risk score in the multivariable model. Patients with anxiety were less likely to have a university level education. The 3 HADS groups were not markedly different in procedure type. The median STS-PROMM was 17%, 16%, and 15% for the no anxiety, possible anxiety, and anxiety groups, respectively ( Table 2 ).
| Variable | No Anxiety (HADS-A 0–7; n = 105) | Possible Anxiety (HADS-A 8–10; n = 32) | Anxiety HADS-A (11–21; n = 11) |
|---|---|---|---|
| Age (yrs) | 75 (72, 79) | 76 (73, 80) | 76 (71, 79) |
| Women | 29 (28%) | 17 (53%) | 4 (36%) |
| Living alone | 30 (29%) | 9 (28%) | 4 (36%) |
| University-level education | 34 (32%) | 8 (25%) | 1 (9%) |
| General perception of health | |||
| Very good | 29 (28%) | 4 (13%) | 0 (0%) |
| Good | 47 (45%) | 12 (38%) | 5 (45%) |
| Fair | 27 (26%) | 10 (31%) | 4 (36%) |
| Poor | 2 (2%) | 6 (19%) | 1 (18%) |
| Body mass index (kg/m 2 ) | 26 (24, 29) | 27 (23, 30) | 27 (26, 30) |
| Diabetes mellitus | 39 (37%) | 13 (41%) | 4 (36%) |
| Hypertension | 75 (71%) | 26 (81%) | 8 (73%) |
| Dyslipidemia | 67 (64%) | 22 (69%) | 9 (82%) |
| Current or past smoker | 59 (56%) | 20 (62%) | 5 (45%) |
| Chronic heart failure | 30 (29%) | 9 (28%) | 2 (18%) |
| Left ventricular ejection fraction (%) | 55 (45, 60) | 60 (54, 65) | 55 (35, 65) |
| Atrial fibrillation | 17 (16%) | 4 (13%) | 3 (27%) |
| Chronic renal failure | 19 (18%) | 6 (19%) | 2 (18%) |
| Stroke | 12 (11%) | 3 (9%) | 1 (9%) |
| History of anxiety | 6 (6%) | 2 (6%) | 0 (0%) |
| History of depression | 5 (5%) | 2 (6%) | 1 (9%) |
| Hospital Anxiety and Depression Scale depression score (/11) | 2 (1, 4) | 4 (2, 7) | 8 (6, 10) |
| Mini-mental state examination score (/30) | 27 (23, 29) | 28 (26, 29) | 27 (25, 29) |
| Frailty (Cardiovascular Health Study scale) | 16 (15) | 9 (28) | 5 (45) |
| Surgery type | |||
| Isolated coronary artery bypass grafting | 64 (61%) | 18 (56%) | 8 (73%) |
| Valve procedure with or without coronary artery bypass grafting | 41 (39%) | 14 (44%) | 3 (27%) |
| Urgent surgery | 56 (53%) | 20 (63%) | 5 (45%) |
| Society of Thoracic Surgeons predicted risk of mortality or major morbidity (%) | 17 (11, 26) | 16 (13, 21) | 15 (10, 23) |
| Society of Thoracic Surgeons predicted risk of mortality (%) | 3 (1, 4) | 2 (2, 3) | 2 (1, 4) |
| Logistic EuroSCORE | 7 (4, 12) | 8 (5, 14) | 6 (4, 9) |
The median mini-mental state examination score was 27 of 30 (normal range), without differences across the 3 HADS-A groups. An existing diagnosis of depression was more often present in patients with anxiety, and the median HADS-D score was 2, 4, and 8 for the no anxiety, possible anxiety, and anxiety groups, respectively ( Table 2 ).
The clinical outcomes according to the HADS-A score are listed in Table 3 . The composite end point of mortality or major morbidity occurred in 22% of the no anxiety group, 25% of the possible anxiety group, and 55% of the anxiety group. In-hospital mortality across the 3 HADS-A score groups (no anxiety, possible anxiety, and anxiety group) was 4%, 6%, and 9%, respectively. Discharge to a healthcare facility (nursing home or convalescence or rehabilitation facility) was also increased with increasing anxiety.



