Despite advances in cardiopulmonary resuscitation (CPR), survival remains low after out-of-hospital cardiac arrest (OOHCA). Acute coronary ischemia is the predominating precipitant, and prompt delivery of patients to dedicated facilities may improve outcomes. Since 2011, all patients experiencing OOHCA in London, where a cardiac etiology is suspected, are systematically brought to heart attack centers (HACs). We determined the predictors for survival and favorable functional outcomes in this setting. We analyzed 174 consecutive patients experiencing OOHCA from 2011 to 2013 brought to Harefield Hospital—a designated HAC in London. We analyzed (1) all-cause mortality and (2) functional status using a modified Rankin scale (mRS 0 to 6, where mRS0-3 + = favorable functional status). The overall survival rates were 66.7% (30 days) and 62.1% (1 year); and 54.5% had mRS0-3 + at discharge. Patients with mRS0-3 + had reduced mortality compared to mRS0-3 − : 30 days (1.2% vs 72.2%, p <0.001) and 1 year (5.3% vs 77.2%, p <0.001). Multivariate analyses identified lower patient comorbidity, absence of cardiogenic shock, bystander CPR, ventricular tachycardia/ventricullar fibrillation as initial rhythm, shorter duration of resuscitation, prehospital advanced airway, absence of adrenaline and inotrope use, and intra-aortic balloon pump use as predictors of mRS0-3 + . Consistent predictors of increased mortality were the presence of cardiogenic shock, advanced airway use, increased duration of resuscitation, and absence of therapeutic hypothermia. A streamlined delivery of patients experiencing OOHCA to dedicated facilities is associated with improved functional status and survival. Our study supports the standardization of care for such patients with the widespread adoption of HACs.
The incidence of out-of-hospital cardiac arrests (OOHCAs) is approximately 60,000 in the United Kingdom and 420,000 in the United States each year. Coronary artery disease is responsible for >70% of OOHCA, and rapid access to cardiac catheterization may improve outcomes in these patients. Since 2011, the London Ambulance Service (LAS) embarked on a pathway enabling ambulance personnel to bypass the nearest hospital and transfer patients with OOHCA, if the cause was considered primarily cardiac, directly to 1 of 8 heart attack centers (HACs) for immediate cardiac catheterization and revascularization, if indicated. This has led to a significant increase in survival rate—discharge survival rates for those meeting the Utstein comparator criteria increased from 12% in 2007 to 32% in 2012. Randomized studies are often difficult in patients with OOHCA, and our understanding in this field is largely driven by observational data. Although many observational studies have documented predictors of outcomes in these patients, there are no studies specifically examining the outcomes where patients experiencing OOHCA undergo a prehospital triaging system and strategic delivery to dedicated HACs, particularly over a contemporary period. Thus, we analyzed the predictors of favorable functional status and survival in patients experiencing OOHCA in this setting.
Methods
This was an observational analysis to determine the predictors of favorable functional status at discharge and long-term survival in 182 consecutive patients experiencing an OOHCA from 2011 to 2013 who were brought directly by the emergency medical services (EMS) to Harefield Hospital, Middlesex—1 of 8 designated heart attack centers in London. Of these, return of spontaneous circulation was achieved in 174 patients (96%) and included in the final analysis. The LAS is the largest free emergency medical ambulance service in the world operating from 69 ambulance stations. It is a publicly funded National Health Service (NHS) organization, serving 8.2 million people and covering an area of 1,579 km 2 . Patients are usually conveyed to 1 of 35 emergency departments or 8 HACs in the Greater London area. All clinical data for this study were collected prospectively as part of the British Cardiovascular Intervention Society–National Institute for Cardiovascular Outcomes Research database that collects data from all hospitals in the United Kingdom that perform percutaneous coronary intervention, recording information about every procedure performed.
We analyzed functional status at discharge and all-cause mortality at 30 days and 1 year. The functional status at discharge was established by reviewing case notes and graded using a modified Rankin Scale (mRS). This scale grades functional status as 0, no symptoms; 1, no significant disability, able to carry out all usual activities despite some symptoms; 2, slight disability, able to look after own affairs without assistance but unable to carry out all previous activities; 3, moderate disability, requires some help but able to walk unassisted; 4, moderately severe disability, unable to attend to own bodily needs without assistance and unable to walk unassisted; 5, severe disability, requires constant nursing care and attention, bedridden, incontinent; and 6, dead. This grading system is widely reported in studies with patients experiencing OOHCA where mRS0-3 + is indicative of favorable functional status. Patients’ survival data were obtained by linkage of patients’ NHS numbers to the Office of National Statistics, which records the date of death for all patients. All patient identifiable information was removed before analysis. Because this analysis was performed on anonymized data from mandatory audit, the local ethics committee advised us that ethical approval was not required.
Patients were divided into mRS0-3 + and mRS0-3 − groups, indicating favorable and poor functional status at discharge, respectively. All continuous variables had skewed distributions and thus summarized as medians (lower and upper quartiles) and compared using the Mann–Whitney U test (2 tailed). Categorical variables were expressed as percentages and compared using the Z test (2 tailed). All statistical analyses were performed using MedCalc v12.1 (MedCalc Software, Ostend, Belgium) and R (Foundation for Statistical Computing, Vienna, Austria). Statistical significance was established at p <0.05 (2 tailed) for all tests. All data are reported according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines.
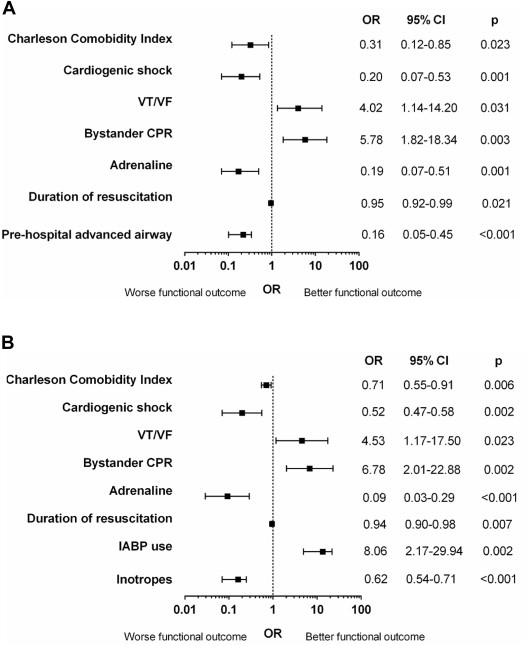
To determine independent predictors for favorable functional status, logistic regression models were used to provide adjusted odds ratios with 95% confidence intervals (CIs). The goodness of fit was determined using both the Hosmer–Lemeshow test and the discriminatory power using receiver operating characteristic (ROC) curve analysis (c statistic). To determine the variables for each final multivariate model, we first examined all variables using a stepwise variable selection process, in which the entry criteria was set at the p <0.05 level and exit criteria set at p >0.1. The significant variables from this were included in the final multivariate model. We used 2 multivariate models (1) a prehospital model which adjusted for witnessed arrest, call to EMS arrival time, bystander CPR, ventricular tachycardia/ventricullar fibrillation (VT/VF) as initial rhythm, delivery of shocks, adrenaline administration, duration of resuscitation, Charleson comorbidity index (CMI), male gender, cardiogenic shock, ST elevation on electrocardiogram (ECG), and prehospital advanced airway and (2) an inhospital model which adjusted for the covariates in the prehospital model but also included advanced airway use, cardiac catheterization, inpatient revascularization, intra-aortic balloon pump (IABP) use, inotrope use, hypothermia, hemoglobin, creatinine, and hemodialysis requirement. The variables included in the final prehospital multivariable model were CMI, cardiogenic shock, VT/VF as initial rhythm, bystander CPR, adrenaline administration, duration of resuscitation and prehospital advanced airway, and those included in the final inhospital multivariable model were CMI, cardiogenic shock, VT/VF as initial rhythm, bystander CPR, adrenaline administration, duration of resuscitation, IABP use, and inotrope use. In this way, the number of variables was limited to 1 per ≥10 events to prevent overfitting of the model. No significant colinearity was demonstrated for the variables in each of the final logistic regression models.
To determine independent predictors for mortality, Cox proportional hazards regression models were used to provide adjusted hazard ratios (HRs) with 95% CIs. The proportional hazards assumption was tested and verified with Schoenfeld residuals. To determine the variables for the final multivariate model, we first examined all variables using a stepwise variable selection process (as mentioned previously), adjusting for witnessed arrest, call to EMS arrival time, bystander CPR, VT/VF as initial rhythm, delivery of shocks, adrenaline administration, duration of resuscitation, CMI, male gender, cardiogenic shock, ST elevation on ECG, advanced airway, cardiac catheterization, inpatient revascularization, IABP use, inotrope use, hypothermia, hemoglobin, creatinine, hemodialysis requirement, and predischarge implantable cardioverter defibrillator insertion. The variables included in the final multivariable model for 30-day mortality were cardiogenic shock, duration of resuscitation, advanced airway use, hypothermia, and cardiac catheterization and for 1-year mortality were CMI, cardiogenic shock, duration of resuscitation, advanced airway use, hypothermia, and predischarge implantable cardioverter defibrillator therapy. In this way, the number of variables were limited to 1 per ≥10 events to prevent overfitting of the model. No significant colinearity was demonstrated for the variables in each of the final Cox regression models. Cumulative mortality rates were also presented as Kaplan–Meier curves and compared with the log-rank test.
The proportion of patients surviving with favorable functional status was plotted as a function of duration of CPR and was modeled using decay kinetics (TableCurve 2D v.50, Systat, California). The goodness of fit was assessed using the F statistics. The kinetic equation was used to determine proportion of patients surviving with favorable functional status at different time points.
Results
The patient characteristics are summarized in Table 1 . For the 174 patients who were successfully resuscitated, (1) the mortality rate was 33.3% at 30 days and 37.9% at 1 year and (2) 63.5% survived to hospital discharge with 54.6% having a favorable functional status (mRS0-3 + ).
| Total n=174 | Functional status at discharge | |||
|---|---|---|---|---|
| mRS0-3 + n=95 | mRS0-3 – n=79 | p-value | ||
| Baseline characteristics | ||||
| Age (years) | 65(56,65) | 63(55,72) | 70(56,69) | 0.015 |
| Male | 79.9% | 82.1% | 77.2% | 0.423 |
| Hypertension | 35.1% | 32.6% | 38.0% | 0.462 |
| Hypercholesterolaemia | 32.2% | 35.8% | 27.8% | 0.264 |
| Diabetes | 18.4% | 13.7% | 24.1% | 0.079 |
| Peripheral vascular disease | 4.0% | 6.3% | 1.3% | 0.091 |
| Previous myocardial infarction | 20.7% | 21.1% | 20.3% | 0.897 |
| Previous percutaneous coronary intervention | 9.2% | 7.4% | 11.4% | 0.360 |
| Previous coronary artery bypass surgery | 6.3% | 4.2% | 8.9% | 0.209 |
| Previous cerebrovascular accident | 5.2% | 5.3% | 5.1% | 0.953 |
| Renal disease | 4.6% | 3.2% | 6.3% | 0.320 |
| Smoking | 21.8% | 28.4% | 13.9% | 0.021 |
| Asthma/Obstructive airways disease | 6.9% | 2.1% | 12.7% | 0.006 |
| Dementia | 4.6% | 2.1% | 7.6% | 0.085 |
| Malignancy | 6.3% | 9.5% | 2.5% | 0.061 |
| Charleson Comorbidity Index | 4(2,5) | 3(2,5) | 4(3,5) | 0.064 |
| Event characteristics | ||||
| Witnessed | 92.0% | 93.7% | 89.9% | 0.358 |
| Witnessed by emergency medical services | 34.5% | 48.4% | 17.7% | <0.001 |
| Bystander cardiopulmonary resuscitation | 79.3% | 87.4% | 69.6% | 0.004 |
| Initial rhythm | ||||
| Ventricular tachycardia/ventricular fibrillation | 82.8% | 92.6% | 70.9% | <0.001 |
| Electromechanical dissociation | 10.9% | 5.3% | 17.7% | 0.009 |
| Asystole | 6.3% | 2.1% | 11.4% | 0.012 |
| EMS interventions | ||||
| Call to emergency medical services (min) | 10(6,15) | 11(6,16) | 9(6,14) | 0.100 |
| Duration of resuscitation (min) | 8(4,17) | 4(2,12) | 16(8,30) | <0.001 |
| Any shocks delivered | 85.6% | 90.5% | 79.7% | 0.044 |
| Number of shocks delivered | 1(1,3) | 1(1,3) | 1(1,5) | 0.502 |
| Adrenaline administered | 45.4% | 18.9% | 77.2% | <0.001 |
| Pre-hospital advanced airway | 25.3% | 13.7% | 39.2% | <0.001 |
| ECG characteristics | ||||
| ST elevation | 73.6% | 74.7% | 72.2% | 0.700 |
| Anterior ST elevation | 34.5% | 38.9% | 29.1% | 0.174 |
| Inferior ST elevation | 19.0% | 15.8% | 22.8% | 0.241 |
| Lateral ST elevation | 5.2% | 8.4% | 1.3% | 0.034 |
| Other | 15.5% | 13.7% | 17.7% | 0.464 |
| Left bundle branch block | 5.2% | 2.1% | 8.9% | 0.045 |
| Other | 21.3% | 23.2% | 19.0% | 0.503 |
| Inpatient intervention | ||||
| First recorded systolic BP (mmHg) | 123(100,140) | 126(110,140) | 117(90,138) | 0.038 |
| Cardiogenic shock | 31.6% | 14.7% | 51.9% | <0.001 |
| Advanced airway | 55.2% | 29.5% | 86.1% | <0.001 |
| Cardiac catheterisation | 92.0% | 97.9% | 84.8% | 0.002 |
| Inotropes administered | 35.1% | 17.9% | 55.7% | <0.001 |
| Intra-aortic balloon pump use | 31.6% | 28.4% | 35.4% | 0.321 |
| Hypothermia | 39.7% | 24.2% | 58.2% | <0.001 |
| Coronary revascularisation | 66.1% | 76.8% | 53.2% | 0.001 |
| Percutaneous coronary intervention | 63.8% | 72.6% | 53.2% | 0.008 |
| Coronary artery bypass surgery | 2.9% | 5.3% | 0.0% | 0.039 |
| Implantable cardioverter defibrillator | 12.6% | 23.2% | 0.0% | <0.001 |
| Investigations | ||||
| Haemoglobin (g/dL) | 13.4(12.4,14.7) | 13.9(12.6,15.0) | 13.0(11.5,14.3) | 0.002 |
| Creatinine (μmol/L) | 97(81,126) | 92(76,109) | 115(90,146) | <0.001 |
| Left ventricular ejection fraction (%) | 47(40,56) | 49(40,57) | 43(37,53) | 0.088 |
Multivariate logistic regression analyses were used to identify independent predictors of mRS0-3 + ( Figure 1 ). Consistent predictors of mRS0-3 + in both models included a lower CMI, absence of cardiogenic shock, bystander CPR, VT/VF as initial rhythm, shorter duration of resuscitation, and absence of adrenaline administration. In the inhospital adjusted model, the IABP use and absence of inotropic support were identified as other predictors of mRS0-3 + .