Isolated left ventricular noncompaction is a rare form of primary cardiomyopathy. Although increasingly diagnosed, data on the outcomes are limited. To define the predictors of adverse outcomes, we performed a retrospective analysis of a prospectively defined cohort of consecutive patients (age >14 years) diagnosed with left ventricular noncompaction at a single center. The baseline characteristics included presentation with a cardiovascular complication (i.e., decompensated heart failure, systemic embolic event, or sustained ventricular arrhythmia). The primary end point was survival free from cardiovascular death or transplantation. The predictors of survival were evaluated using the Kaplan-Meier method and Cox proportional hazards analysis. A total of 115 patients were included, 77% of whom were symptomatic at diagnosis. Compared to the asymptomatic patients, the symptomatic patients were significantly older and had larger left ventricular cavities and worse left ventricular ejection fraction. Of the 115 patients, 49 (43%) presented with a cardiovascular complication. During a median follow-up of 2.7 years (range 0.1 to 19.4), none of the asymptomatic patients died or underwent transplantation compared to 31% (27 of 88) of the symptomatic patients (p = 0.001). The major determinants of cardiovascular death or transplantation were presentation with a cardiovascular complication (hazard ratio 20.6, 95% confidence interval 4.9 to 87.5, p <0.0001) or New York Heart Association class III or greater (hazard ratio 8.8, 95% confidence interval 3.2 to 24.0, p <0.0001). Left ventricular dilation and systolic dysfunction were less strong predictors. In conclusion, in patients with left ventricular noncompaction, New York Heart Association class III or greater and cardiovascular complications at presentation are strong predictors for adverse outcome.
Isolated left ventricular noncompaction (LVNC) is a rare cardiomyopathy with considerable genetic heterogeneity. Despite its increasing recognition and diagnosis, the clinical outcome of this rare entity is not well defined. The aim of the present study was to examine the clinical outcomes in a relatively large, prospectively defined, cohort of patients with LVNC and to identify the risk factors for adverse cardiovascular events.
Methods
The diagnostic criteria previously described by our group were used. In the absence of other congenital or acquired structural heart disease or neuromuscular disorders, these criteria included the presence of a typical 2-layered structure of a significantly thickened myocardium. The thickened 2-layered myocardium consisted of a thin, compacted outer (epicardial) layer and a much thicker, noncompacted inner (endocardial) layer with deep intertrabecular recesses filled with blood from the left ventricular cavity. A noncompacted/compacted layer ratio of >2, obtained in the parasternal short-axis view, had to be present at end-systole. All diagnoses were established by echocardiography and required independent agreement by 2 experienced echocardiographers (R.J. and E.O.). These criteria were previously validated against dilated cardiomyopathy, hypertensive heart disease, and valvar heart disease and showed good sensitivity and specificity. To define the extent of involvement, the left ventricle was divided into 9 segments, as previously described. The left ventricular dimensions and function at the diagnosis and during follow-up were assessed according to the established guidelines for 2-dimensional echocardiography. The left ventricular dimensions were normalized for the body surface area.
Left ventricular noncompaction was diagnosed in 152 consecutive patients >14 years old at a single tertiary referral center, University Hospital, Zurich (0.15% of all echocardiograms) from 1984 to 2006. Twenty patients were excluded because they had associated congenital heart disease. This left 132 patients with LVNC in the study cohort. The lower age limit of 14 years was chosen to allow enrollment of adolescents identified by family screening but to avoid enrollment of neonatal LVNC or LVNC with symptom onset in early childhood, a disease entity that is often accompanied by syndromic association and might have a different outcome than LVNC diagnosed in adulthood.
The clinical characteristics collected at initial presentation were the presence and nature of cardiac symptoms, functional class (New York Heart Association classification) and the occurrence of cardiovascular complications at the initial assessment or before presentation. The latter included decompensated heart failure requiring hospital admission, systemic embolic events, sustained ventricular arrhythmias, and/or presentation with survived sudden cardiac death.
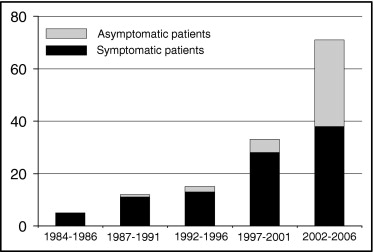
Figure 1 depicts the number of newly diagnosed patients with LVNC at our center during the study period. The increased number of asymptomatic patients after 2000 reflects our policy of routine family screening.
Of the 132 patients within the study cohort, 115 (87%) had ≥1 year of follow-up or died or underwent heart transplantation within the first 12 months after diagnosis. These 115 patients were included in the survival analysis. Follow-up information was collected by retrospective chart review. The initial presentation and outcome of the first 34 patients of the cohort have been previously reported.
The primary end point included cardiovascular death or heart transplantation. Other major adverse events were recorded and included systemic embolism, sustained ventricular arrhythmias, and admission for heart failure. Cardiovascular death was defined as death directly related to progressive heart failure, sudden death (death within 1 hour of the onset of symptoms, or acute deterioration of a symptomatic patient with previously stable symptoms), death related to cardioembolic stroke, death caused by pulmonary embolism, or death ensuing in the immediate sequence of a cardiovascular intervention or operation.
Statistical analysis was performed using the Statistical Package for Social Sciences, version 17.0 (SPSS, Chicago, Illinois). The descriptive data are presented as the median (range), mean ± SD, and proportions, as appropriate. A comparison between survivors and nonsurvivors and the groups of patients presenting with and without symptoms was performed using Student’s t test, the Mann-Whitney test, or the chi-square test. Kaplan-Meier curves were used to depict differences between patients with and without symptoms at presentation, cardiovascular complications at presentation, New York Heart Association class III or greater, left ventricular end-diastolic diameter indexed to the body surface area >3.7 cm/m 2 and a left ventricular ejection fraction <35%. The predictors of survival free from cardiovascular death or heart transplantation were determined using a Cox proportional hazards model. A p value <0.05 (2-sided) was considered significant.
Results
The clinical, echocardiographic, and electrocardiographic baseline characteristics of the entire study cohort, survivors, and patients with cardiovascular death/transplantation are summarized in Table 1 . At the diagnosis, 66 symptomatic patients (50%) were receiving medical treatment. The most common medications were angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists (36%), β blockers (38%), and diuretics (26%); 48 patients (36%) were taking oral anticoagulation drugs and 9 (7%) low-dose aspirin.
| Variable | All Patients ⁎ (n = 132) | Nonsurvivors ⁎ (n = 27) | Survivors ⁎ (n = 88) | p Value † |
|---|---|---|---|---|
| Age (years) | 41 ± 17 | 48 ± 17 | 40 ± 17 | 0.02 |
| Female gender | 86 (65%) | 18 (67%) | 57 (65%) | 1.0 |
| Presentation with any symptoms ‡ | 95 (72%) | 27 (100%) | 61 (69%) | <0.0001 |
| New York Heart Association class III or greater at presentation | 46 (35%) | 20 (74%) | 23 (26%) | <0.0001 |
| Presentation with any complication § | 51 (39%) | 24 (89%) | 26 (30%) | <0.0001 |
| Decompensated heart failure | 44 (33%) | 19 (70%) | 24 (27%) | <0.0001 |
| Systemic embolization | 3 (2%) | 1 (4%) | 2 (2%) | 0.56 |
| Transient ischemic attack | 1 (1%) | — | 1 (1%) | — |
| Peripheral emboli | 2 (2%) | 1 (4%) | 1 (1%) | — |
| Sustained ventricular arrhythmia | 9 (7%) | 6 (22%) | 3 (3%) | 0.005 |
| Echocardiographic variables | ||||
| Left ventricular ejection fraction | 41 ± 18% | 31 ± 11% | 43 ± 19% | 0.001 |
| Left ventricular end-diastolic diameter indexed to body surface area (cm/m 2 ) | 3.4 ± 0.7 | 3.9 ± 0.7 | 3.3 ± 0.6 | <0.0001 |
| Electrocardiographic abnormalities | ||||
| Atrial fibrillation | 18 (14%) | 10 (37%) | 8 (9%) | 0.001 |
| Bundle branch block ∥ | 32 (24%) | 15 (56%) | 16 (18%) | <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


