Several epidemiologic studies have demonstrated that plasma low-density lipoprotein cholesterol (LDL-C) profile is a key risk indicator for coronary heart disease (CHD). However, almost half of all patients with CHD have normal LDL-C levels. A total of 7,931 male subjects aged ≥40 years from the general population with no cardiovascular history and no use of lipid-lowering agents were followed for incidence of acute myocardial infarction (AMI) and sudden death. Of the 4,827 participants with LDL-C levels <120 mg/dl, 55 subjects had a first AMI/sudden death during an average of 5.5 years of follow-up. After adjustment for confounding factors, multiadjusted hazard ratios (HRs) were increased by 1 SD for non-high-density lipoprotein cholesterol (non-HDL-C; HR = 1.36, 95% confidence interval [CI], 1.02 to 1.81), total cholesterol (TC)/HDL-C ratio (HR = 1.40, 95% CI: 1.11 to 1.78) and LDL-C/HDL-C ratio (HR = 1.32, 95% CI: 1.02 to 1.73) but not for LDL-C (HR = 1.09, 95% CI: 0.82 to 1.44) and HDL-C (HR = 0.84, 95% CI: 0.68 to 1.04). When stratified as categorical variables on the basis of points with highest accuracy on receiver operating characteristic analysis, non-HDL-C levels >126 mg/dl (HR = 1.25, 95% CI: 1.03 to 1.51), TC/HDL-C ratio above 3.5 (HR = 1.22, 95% CI: 1.01 to 1.48) and LDL-C/HDL-C ratio >1.9 (HR = 1.25, 95% CI: 1.04 to 1.51) had increased multiadjusted HRs for AMI/sudden death. In conclusion, in men with LDL-C levels <120 mg/dl, non HDL-C, TC/HDL-C, and LDL-C/HDL-C ratios have predictive value for residual risk of AMI/sudden death.
Low-density lipoprotein cholesterol (LDL-C) has been identified as a key risk factor for coronary heart disease (CHD) by several epidemiological and interventional studies. However, almost half of all patients with CHD have normal LDL-C levels. Therefore, the main question is whether there is any residual coronary risk associated with other lipid parameters even at normal LDL-C levels. High-density lipoprotein cholesterol (HDL-C) has been identified as one of the major risk factors that modify LDL-C target by the current National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) guidelines. Non-HDL-C and the ratios of total cholesterol (TC) or LDL-C to HDL-C have been revealed to have predictive power for atherosclerotic cardiovascular disease and provide incremental predictive value over TC or LDL-C levels. Thus, these indices may be the parameters for CHD-related risk even in individuals with normal LDL-C levels; however, this remains unclear because prospective epidemiologic data are limited. The objective of the present study was to investigate whether lipid parameters including LDL-C, HDL-C, non-HDL-C, TC/HDL-C ratio, or LDL-C/HDL-C ratio are correlated with the development of CHD at LDL-C levels <120 mg/dl in the Japanese general population.
Methods
The Iwate-KENCO study cohort is a population-based prospective study of residents in the northern part of Iwate prefecture, northeast of Honsyu, Japan. Details of this cohort are provided elsewhere. Participants were recruited from a government-regulated multiphasic health checkup. Of the 31,318 (11,003 men) residents aged ≥18 years who took part in the health checkup program between April 2002 and January 2005, 26,469 (9,161 men) consented to participate in this cohort study (85%). After exclusion of those with previous myocardial infarction or angina pectoris (185 men), previous stroke (328 men), use of lipid-lowering agents (249 men), or missing data (222 men) at baseline, 7,931 male subjects aged ≥40 years were recruited into the study.
Diagnosis of acute myocardial infarction (AMI) was based on the criteria of the World Health Organization-MONICA (Monitoring Trends and Determinants of Cardiovascular Disease) project, which requires evidence from suspected symptoms, an electrocardiogram, cardiac enzymes, and/or autopsy. Sudden death was defined as any death after exclusion of known causes in a person who had sudden loss of ability to carry out normal activity due to serious physical impairment with death following in <24 hours.
Patients with newly diagnosed AMI and sudden death were registered from April 2002 to August 2007. Incidents of AMI were identified by accessing data from the Northern Iwate Heart Disease Registry Consortium, which has been collecting data since 2002. Registration was initially performed by attending physicians at each hospital. To ensure complete capture of all registrations, physicians or trained research nurses reviewed medical charts and/or discharge summaries at referral hospitals within the study area. Furthermore, to capture registrations of sudden death irrespective of hospital visit, we reviewed death certificates at government offices within the target district and identified sudden death (I46.1, R96) according to the International Classification of Diseases, 10th Revision . The study was approved by our institutional ethics committee. Women were excluded from the analysis because of the low incidence of AMI/sudden death (41 events among 14,636 women; 0.3%).
Body mass index was calculated by dividing weight (in kilograms) by the square of height (in meters). Participants completed a self-report questionnaire to document their medical history including current medications and lifestyle factors such as smoking habits. Blood pressure was measured twice using an automatic digital sphygmomanometer after 5 minutes of rest in a sitting position, and the average of these two values was used for analysis. Both fasting (n = 1,287) and nonfasting (n = 6,644) blood samples were drawn from an antecubital vein and collected into vacuum tubes containing a serum separator gel. Tubes were stored immediately after sampling in an icebox and transported to the laboratory <8 hours after collection. Glycosylated hemoglobin was measured quantitatively using high-performance liquid chromatography. Serum TC and HDL-C concentrations were measured by an enzymatic method. Serum LDL-C concentrations were measured by an enzymatic homogeneous assay Cholestest-LDL (Daiichi Chemicals Co. Ltd, Tokyo, Japan). Measurements for TC, HDL-C, and LDL-C (homogeneous assays) have been standardized by the Osaka Medical Center for Health Science and Promotion, a member of the Cholesterol Reference Method Laboratory Network (CRMLN) controlled by the CDC (Centers for Disease Control and Prevention, Atlanta, Georgia) and have met all criteria for both precision and accuracy of lipid measurements.
Non-HDL-C was calculated as follows: non-HDL-C = TC to HDL-C. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or current use of antihypertensive agents. Diabetes mellitus (DM) was defined as a random blood glucose level ≥200 mg/dl, a glycosylated hemoglobin value ≥6.5%, and/or current antidiabetic therapy. Estimated glomerular filtration rate (eGFR) was calculated using an equation (eGFR [ml/min/1.73m 2 ] = 194 × serum creatinine −1.094 × age −0.278 ) from the Modification of Diet in Renal Disease (MDRD) study. Smoking habit was defined as current smoking.
Data are presented as mean ± SD or percentage. All data were analyzed using SPSS statistical software, version 11.0. We defined normal levels of LDL-C as <120 mg/dl in line with the Japan Atherosclerosis Society’s suggested LDL-C levels of 120 to 139 mg/dl as borderline hyper LDL-cholesterolemia and LDL-C levels of ≥140 mg/dl as hyper LDL-cholesterolemia. Baseline characteristics were shown in total participants and those with LDL-C levels <120 mg/dl.
Cox regression analysis was used to calculate hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) for lipid indices in relation to risk of future AMI/sudden death. A multivariate Cox proportional hazards model was constructed including lipid indices and adjusting for age, body mass index, systolic blood pressure, eGFR, presence of DM, and smoking habits. We calculated multivariable HRs for a 1 standard deviation (SD) increase in levels of LDL-C, HDL-C and non-HDL-C, and for TC/HDL-C ratio or LDL-C/HDL-C ratio in total participants and those with LDL-C levels <120 mg/dl. The SD units correspond to 29.1 mg/dl for LDL-C, 15.4 mg/dl for HDL-C, 32.7 mg/dl for non-HDL-C, 1.06 for TC/HDL-C ratio, and 0.85 for LDL-C/HDL-C ratio in total participants, and 17.5 mg/dl for LDL-C, 16.5 mg/dl for HDL-C, 21.6 mg/dl for non-HDL-C, 0.86 for TC/HDL-C ratio, and 0.62 for LDL-C/HDL-C ratio in participants with LDL-C levels <120 mg/dl. The lipid indices showing a linear correlation with risk were used to construct a receiver operating characteristic (ROC) curve with AMI/sudden death events as the outcome. The crude and multivariable adjusted HRs with corresponding 95% CIs for risk of future AMI/sudden death in the categorical variables of lipid indices on the basis of points with highest accuracy on ROC analysis were calculated for total participants and for those with LDL-C levels <120 mg/dl. To determine the HR for future AMI/sudden death, p <0.05 was considered statistically significant.
Results
Of the 7,931 participants, 4,827 (60.9 %) had LDL-C levels <120 mg/dl at the baseline survey. Table 1 shows the baseline characteristics of total participants and those with LDL-C levels <120 mg/dl. During the average 5.5 years of follow-up, 113 subjects (1.4 %) had a first AMI/sudden death.
| Variable | Total | LDL-C <120 mg/dL |
|---|---|---|
| (n = 7,931) | (n = 4,827) | |
| Age (yrs) | 64 ± 10 | 65 ± 10 |
| Body mass index (kg/m 2 ) | 23.9 ± 3.0 | 23.5 ± 3.0 |
| Total cholesterol (mg/dl) | 191 ± 32 | 173 ± 23 |
| LDL-C (mg/dl) | 113 ± 29 | 95 ± 17 |
| HDL-C (mg/dl) | 56 ± 15 | 58 ± 17 |
| Total/HDL-C | 3.62 ± 1.06 | 3.20 ± 0.86 |
| LDL-C/HDL-C | 2.18 ± 0.85 | 1.78 ± 0.62 |
| Non-HDL-C (mg/dl) | 135 ± 33 | 116 ± 22 |
| Systolic blood pressure (mm Hg) | 131 ± 20 | 131 ± 20 |
| Diastolic blood pressure (mm Hg) | 79 ± 11 | 78 ± 11 |
| Hypertension | 46.6% | 46.4% |
| eGFR (ml/min/1.73 m 2 ) | 73 ± 15 | 74 ± 15 |
| Diabetes mellitus | 7.8% | 7.6% |
| Current smoker | 31.1% | 31.9% |
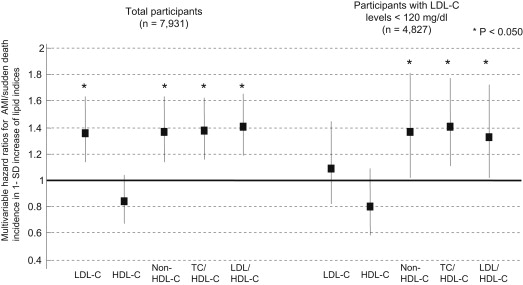
Figure 1 shows HRs for future AMI/sudden death associated with a 1-SD increase of LDL-C, HDL-C, non-HDL-C, and TC/HDL-C or LDL-C/HDL-C ratio after adjustment for age, body mass index, systolic blood pressure, eGFR, presence of DM, and smoking habits. Among all participants, adjusted HRs were increased with a 1 SD increase in LDL-C (HR = 1.36, 95% CI: 1.14 to 1.63), non-HDL-C (HR = 1.36, 95% CI: 1.13 to 1.64), TC/HDL-C ratio (HR = 1.37, 95% CI: 1.16 to 1.62), and LDL-C/HDL-C ratio (HR = 1.40, 95% CI: 1.19 to 1.65) but not HDL-C (HR = 0.84, 95% CI: 0.68 to 1.04). However, in participants with LDL-C levels <120 mg/dl, the increased HR associated with a 1 SD increase of LDL-C was not significant (HR = 1.09, 95% CI: 0.82 to 1.44). In contrast, HRs remained increased significantly with a 1 SD increase in non-HDL-C (HR = 1.36, 95% CI: 1.02 to 1.81), TC/HDL-C ratio (HR = 1.40, 95% CI: 1.11 to 1.78) and LDL-C/HDL-C ratio (HR = 1.32, 95% CI: 1.02 to 1.73).
For categorical analysis of lipid indices showing a linear correlation with risk of future AMI/sudden death, we set the threshold of non-HDL-C, TC/HDL-C ratio, and LDL-C/HDL-C ratio as the optimal cut-off levels for prediction of AMI/sudden death from points with highest accuracy on a ROC curve. As a result, the threshold was 131 mg/dl for non-HDL-C, 3.82 for TC/HDL-C ratio, and 2.51 for LDL-C/HDL-C ratio in total participants, and 126 mg/dl for non-HDL-C, 3.47 for TC/HDL-C ratio, and 1.88 for LDL-C/HDL-C ratio in participants with LDL-C levels <120 mg/dl.
Table 2 shows the crude and multivariable adjusted HRs for risk of future AMI/sudden death with non-HDL-C, TC/HDL-C ratio or LDL-C/HDL-C ratio as the categorical variable on the basis of points with highest accuracy on ROC analysis. Among total participants, the multi-adjusted HRs for AMI/sudden death were increased in individuals with non-HDL-C levels above 131 mg/dl, TC/HDL-C ratio above 3.82, and LDL-C/HDL-C ratio above 2.51. Moreover, in participants with LDL-C levels <120 mg/dl, an increased HR remained significant in individuals with non-HDL-C levels >126 mg/dl, TC/HDL-C ratio >3.47 and LDL-C/HDL-C ratio >1.88.
| Lipid Indices | Total (n = 7,931) | Lipid Indices | LDL-C <120 mg/dl (n = 4,827) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Subjects | No. of Events | No./1,000 person-yrs | Crude HR (95% CI) | Multivariable Adjusted HR (95% CI) ∗ | No. of Subjects | No. of Events | No./1,000 person-yrs | Crude HR (95% CI) | Multivariable Adjusted HR (95% CI) ∗ | ||
| Non HDL-C, 131 mg/dl | Non HDL-C, 126 mg/dl | ||||||||||
| Below | 3,853 | 36 | 1.7 | 1 | 1 | Below | 3,345 | 30 | 1.6 | 1 | 1 |
| Above | 4,078 | 77 | 3.4 | 1.97 (1.33–2.93) | 2.09 (1.40–3.14) | Above | 1,482 | 25 | 3.1 | 1.86 (1.09–3.16) | 2.02 (1.17–3.50) |
| TC/HDL-C, 3.82 | TC/HDL-C, 3.47 | ||||||||||
| Below | 5,024 | 50 | 1.8 | 1 | 1 | Below | 3,325 | 27 | 1.5 | 1 | 1 |
| Above | 2,907 | 63 | 3.9 | 2.17 (1.50–3.15) | 2.19 (1.48–3.24) | Above | 1,502 | 28 | 3.4 | 2.33 (1.37–3.95) | 2.43 (1.39–4.26) |
| LDL-C/HDL-C, 2.51 | LDL-C/HDL-C, 1.88 | ||||||||||
| Below | 5,418 | 54 | 1.8 | 1 | 1 | Below | 2,904 | 23 | 1.4 | 1 | 1 |
| Above | 2,513 | 59 | 4.3 | 2.34 (1.62–3.39) | 2.33 (1.59–3.42) | Above | 1,923 | 32 | 3.1 | 2.14 (1.25–3.65) | 2.06 (1.17–3.61) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


