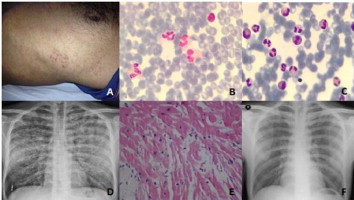
A 38-year-old-man was admitted to emergency department with left inguinal pain and fever. He was hospitalized with the diagnosis of nephrolithiasis and urinary tract infection. Antibiotic theraphy (meropenem 3 grams per day) and analgesic (pethidine 50 mg per day) were given intravenously. About 24 hours after treatment, typical angina pectoris and dyspnea developed. Rash on the chest (Panel A) and reduced bilateral lung sounds and rales were detected. There were nonspecific changes on ECG. Laboratory analysis showed progressively increasing levels of cardiac biomarkers (Peak CKMB: 10.3 ng/ml, peak Troponin I: 1.62 ng/ml) and eosinophilia (white blood cell count was 51.000 and percentage of eosinophils was 57%). Peripheral blood smear (Panel B) and bone marrow aspiration and biopsy (Panel C) demonstrated eosinophilia. Chest X-ray revealed diffuse, bilateral interstitial and reticulonodular infiltrates (Panel D). Transthoracic echocardiography showed thickened left verticle. Coronary angiography showed normal coronary arteries. Endomyocardial biopsy was performed with the suspicion of eosinophilic myocarditis. Pathologic specimen confirmed the diagnosis of eosinophilic myocarditis (Panel E). After the definitive diagnosis corticosteroid treatment started. One day after the treatment, his angina pectoris and dyspnea were dramatically reduced, also cardiac biomarkers and WBC (eosinophils) count were decreased. Chest X-ray was normalized after 72 hours (Panel F). The patient was discharged from the hospital with steroid treatment.