Introduction
The novel oral anticoagulant agents (NOACs) provide compelling evidence-based advances over warfarin therapy in non-valvular atrial fibrillation (AF) and have received endorsement from contemporary guidelines. Rivaroxaban, one of these NOACs, is an oral factor Xa inhibitor that has been studied for prevention of systemic embolism in patients with AF. Previous studies have shown that rivaroxaban, specifically a 2.5 mg twice-daily dose, appears to improve outcomes in patients with recent acute coronary syndrome (ACS) when added to dual antiplatelet therapy. Despite the protective effect of rivaroxaban in ACS, we present here a case of acute inferior myocardial infarction (MI) in a patient undergoing rivaroxaban 15 mg/day therapy. To the best of our knowledge, this is the first such reported case.
Case Presentation
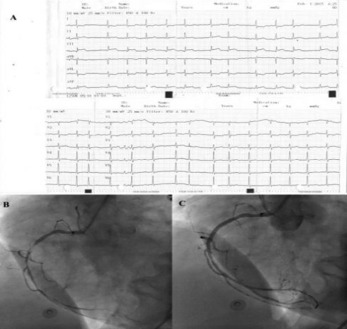
A 73-year-old female patient presented with retrosternal chest pain in the emergency department. The chest pain had been ongoing for the past two hours. Surface electrocardiography (ECG) was consistent with acute inferior ST segment elevation MI (Figure 1A). Her medical history was notable for diabetes mellitus, asthma, hyperthyroidism, and AF. She was taking metformin (1000 mg twice daily), bisoprolol (5 mg/day), free thyroxine (75 mg/day), rivaroxaban (15 mg/day), and propafenone (150 mg twice daily). Rivaroxaban was last taken 12 hours before the patient’s admission to the hospital. The patient was treated with clopidogrel (600 mg), acetylsalicylic acid (300 mg), and unfractional heparin (5000 units) and was taken to the catheter laboratory for primary percutaneous coronary intervention (PCI). Coronary angiography showed subtotal occlusion of the mid-portion of the right coronary artery (RCA) (Figure 1B). The acute lesion in the RCA was treated with a 2.5 x 28 mm Promus drug (everolimus) eluting stent (Figure 1C). The rivaroxaban therapy was discontinued and enoxaparin (0.6 ml twice daily) was given to the patient. After 72 hours, the patient was discharged on evidence-based medicine for ACS (clopidogrel 75 mg, acetylsalicylic acid 100 mg, atorvastatin 40 mg, metoprolol 50 mg, and pantoprazole 40 mg). After three months, rivaroxaban therapy (15 mg/day) was resumed and acetylsalicylic acid therapy was discontinued.