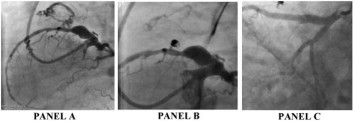
Coronary artery fistula is a rare anomaly, either with congenital or acquired origin, which is characterized by blood flow from myocardial capillary network to any of the heart chambers, great vessels or other structures. A 54-year-old male complaining about chest pain was admitted to our hospital. The patient had history of hypertension and cigarette smoking. Initial blood pressure and heart rate were 144/89 mmHg, 75/min respectively. Physical examination and laboratory findings were unremarkable. Electrocardiography revealed a normal sinus rhythm with left anterior hemiblock. Transthorasic echocardiography showed left ventricular ejection fraction of 62% and left atrial enlargement. The patient underwent to diagnostic coronary angiogram as well as pulmonary angiogram with detection of a fistula originating from aneurysmatic part of proksimal left anterior descending artery to main pulmonary artery and stenotic lesions on LAD. (Panel A) The fistula was occluded with different size of coils (Panel B). 90 % stenotic lesion in distal part and aneurysmatic proximal part of LAD were stented in another session. (Panel C). The patient was discharged from the hospital without complications. Coronary artery fistula is a rare anomaly, and is mainly asymptomatic but may present with fatigue, dyspnea, angina, orthopnea, endocarditis, myocardial ischemia and arrythmias. Main indications of fistula closure are heart failure and symptoms of myocardial ischemia. Surgical or cathater based interventions are recommended for fistula closure. In our case, the fistula was successfully coiled and aneurysmatic part of proximal LAD was stented with cathater based intervention. The patient’s symptoms were completely relieved after interventions.