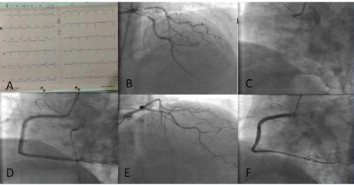
A 53 year old man with the history of hypertension and asthma was admitted to our emergency department with severe crushing chest pain of 2-hour duration. He was smoker and had family history of coronary artery disease. On admission; his blood pressure was hypotensive (85/52 mmHg) and heart rate was 60 bpm. Electrocardiogram (ECG) showed ST elevation in lead II, III, AVF and V4R and there was reciprocal ST depression in lead I, AVL. (Panel A). Aspirin 300 mg orally and ticagrelor 180 mg orally were given. He was immediately taken up coronary anjiography. Coronary anjiography showed 90% stenosis of proximal left anterior descending artery (LAD) and circumflex artery (CX) (Panel B) and showed a totally occlusion of proximal right coronary artery (RCA) (Panel C). The lesion in RCA was crossed with guide wire and predilated with 2.0x10mm balloon. After the predilatation the lesion was stented sequentially 3.0×18 mm stent and 3.0×26 mm stent at 18 atmospheres. During the procedure, atrioventricular block was occurred and transient pacemaker was implanted. Post deployment angiography showed good result with TIMI III flow and no residual stenosis in RCA. (Panel D). For the lesions of LAD and CX, it was decided to intervate in another coronary anjiogarphy session. After the procedure symptoms of patient was not regressed, therefore the patient was taken up to repeat coronary anjiography. Coronary anjiography showed totally normal left sided coronary arteries and RCA stents were totally open (Panel E, F). Lesions of LAD and CX was disappeared. Left sided coronary arteries was thought vasospastic. Patient was discharged on Aspirin 100 mg a day, ticagrelor 90 mg twice a day, diltiazem 90 mg a day, valsartan 80 mg a day, atorvastatin 40 mg a day, isosorbid-5-mononitrat 60 mg a day.