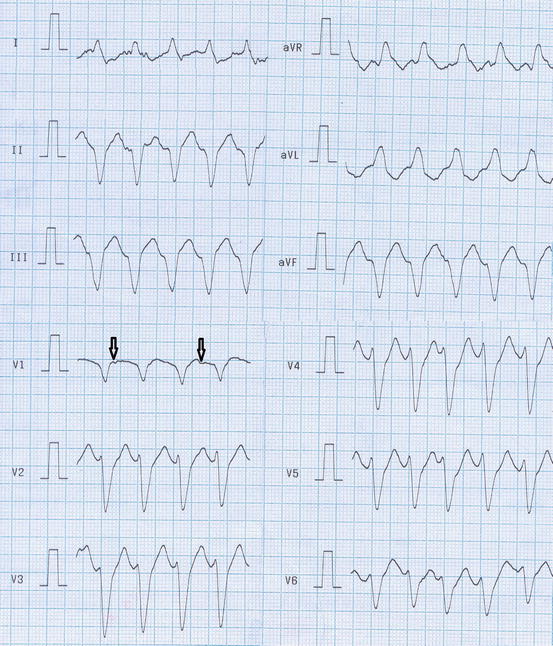
Fig. 9.1
This figure shows atrial fibrillation with undulating atrial activity and irregular ventricular response
9.1.2 Pathogenesis
The mechanism of postoperative AF is not well described and is probably multifactorial. It is suggested that endogenous adenosine, inflammation, and oxidative injury may play a mechanistic role in this arrhythmia (Yavuz et al. 2004; Chung et al. 2001; Korantzopoulos et al. 2006). The perioperative period is also characterized by acute ischemic reperfusion injury and delayed inflammatory response that together result in a net depletion at plasma antioxidants (De Vecchi et al. 1998). Furthermore, patients undergoing cardiac surgery often have underlying atrial enlargement or increased atrial pressures that may predispose to AF. Age-related structural or electrophysiological changes also appear to lower the threshold for postoperative AF in elderly patients (Leitch et al. 1990). Other reported predisposing conditions for development of the postoperative AF included left main or proximal right coronary artery stenoses, chronic obstructive pulmonary disease, beta-blocker withdrawal, history of AF or heart failure, and preoperative electrocardiographic findings of PR interval of 185 ms or longer, P wave duration of 110 ms or longer in lead V1, and left atrial abnormality (Passman et al. 2001; Amar et al. 2004).
Considering the peak incidence of AF in the first 2–3 days after surgery, inflammatory mechanisms have been suggested. The idea has also been supported by the efficacy of anti-inflammatory agents in decreasing the incidence of postoperative AF (Ho and Tan 2009). However, there are other electrophysiological explanations for the higher incidence of AF in this period. Nonuniform atrial conduction is greatest on postoperative days 2 and 3, and longest atrial conduction is on day 3 (Ishii et al. 2005). Perioperative hypokalemia has been shown to be associated with postoperative AF partly via changes in atrial conduction and refractoriness (Wahr et al. 1999).
There are recent evidences indicating that minimally invasive cardiac surgery or surgery without cardiopulmonary bypass has been associated with lower incidence of postoperative AF. In a prospective randomized study, 200 patients were randomly assigned into on-pump CABG and off-pump CABG. The results of this study clearly indicated postoperative AF occurs with lower frequency in patients who underwent off-pump beating heart surgery compared to those with on-pump CABG (Ascione et al. 2000).
9.1.3 Prophylaxis
Several pharmacological and non-pharmacological strategies have been employed to prevent postoperative AF after cardiac surgery. Efficacy of beta-blockers, amiodarone, sotalol, magnesium, and atrial pacing has been assessed in several randomized and nonrandomized clinical trials.
Because patients recovering from cardiac surgery often have enhanced sympathetic tone, the risk of postoperative AF is increased. Beta-blockers antagonize the effects of catecholamines on the myocardium and are, thus, expected to prevent AF after cardiac surgery. Multiple clinical trials and three landmark meta-analyses have shown a significant reduction in postoperative AF by beta-blocker prophylaxis in cardiac surgery patients (Crystal et al. 2002). Following these remarkable results, updated American Heart Association/American College of Cardiology Foundation (AHA/ACCF) 2006/2011 and recent European Society of Cardiology (ESC) 2010 guidelines recommended beta-blocker prophylaxis to prevent AF in cardiac surgery patients in the absence of contraindications (Fuster et al. 2011; Camm et al. 2010). Oral carvedilol, with its unique antioxidant and antiapoptotic properties, appears to be the most effective beta-blocker in the prevention of postoperative AF (Haghjoo et al. 2007). It has been demonstrated that both prophylactic oral and intravenous amiodarone are effective and safe agents in reducing the incidence of AF and its related cerebrovascular accident and postoperative ventricular tachyarrhythmia (Bagshaw et al. 2006). Currently, preoperative administration of amiodarone is deemed class IIa indication for prophylactic therapy in patients at high risk for postoperative AF in the latest AHA/ACCF and ESC guidelines for AF management (Fuster et al. 2011; Camm et al. 2010). Sotalol is a class III antiarrhythmic agent with potent beta-blocking activity. As a result, it would be a suitable drug for AF prevention after cardiac surgeries. Sotalol has been proven to be an effective agent across all the clinical trials using this drug (Pfisterer et al. 1997; Weber et al. 1998). The only issue is related to its safety profile.
Hypomagnesemia has been suggested as a cause of both supraventricular and ventricular tachycardias, and it is an independent risk factor for the development of AF in cardiac surgery patients. Therefore, it has been hypothesized that magnesium supplementation may reduce the incidence of AF after heart surgery. Several clinical trials have examined the use of intravenous magnesium sulfate for the prevention of AF after CABG (Fanning et al. 1991; Kaplan et al. 2003). A meta-analysis of eight identified randomized controlled trials revealed that the use of intravenous magnesium supplementation was associated with a significant reduction in the AF incidence after CABG (Alghamdi et al. 2005).
Overdrive atrial pacing may exert its preventive effect on postoperative AF by suppressing bradycardia-induced irregular heart rate, overdrive suppression of atrial premature beats, suppressing compensatory pauses after atrial premature beats, and resynchronizing atrial activation (Fan et al. 2003). Efficacy of right atrial, left atrial, and biatrial (BiA) pacing has been studied in several randomized studies (Archbold and Schilling 2004). It appears that BiA pacing is more effective than single-site pacing; be that as it may, available data do not permit a firm recommendation on the application of this intervention in a postoperative setting. Recently, the ESC 2010 guidelines on AF management considered BiA pacing as a class IIB recommendation for AF prevention after cardiac surgery (Camm et al. 2010). Latest AHA/ACCF and ESC recommendations for AF prevention in cardiac surgery are summarized in Table 9.1.
Table 9.1
Recommendations for prevention of atrial fibrillation after cardiac surgery
Recommendation | Class | Level |
|---|---|---|
Unless contraindicated, treatment with an oral beta-blocker to prevent postoperative AF is recommended for patients undergoing cardiac surgery | I | A |
Preoperative administration of amiodarone reduces the incidence of AF in patients undergoing cardiac surgery and represents appropriate prophylactic therapy for patients at high risk for postoperative AF | IIa | A |
Prophylactic administration of sotalol may be considered for patients at risk of developing AF following cardiac surgery | IIb | A |
Biatrial pacing may be considered for prevention of AF after cardiac surgery | IIb | A |
Corticosteroids may be considered in order to reduce the incidence of AF after cardiac surgery but are associated with risk | IIb | B |
9.1.4 Management
Considering the self-limited course of the postoperative AF or AFL, treatment begins with pharmacological control of the heart rate (Table 9.2). Beta-blockers should be first-line agents for the rate control because of rapid onset of action and 50 % likelihood of conversion to sinus rhythm. Both metoprolol and esmolol are available in intravenous (IV) formulation. Calcium-channel antagonists are less effective than beta-blockers and considered as second-line agents. Calcium-channel antagonists result in rate control of AF more rapidly than does digoxin. These latter agents may be useful when beta-blockers are contraindicated (i.e., bronchospasm).
Table 9.2
Antiarrhythmic medications used for rate and rhythm control in postoperative atrial fibrillation
Antiarrhythmic | Loading dose | Maintenance dose |
|---|---|---|
Beta-blockers | ||
Esmolol | 500 μg/kg IV over 1 min | 50–200 μg/kg/min IVa |
Metoprolol | 5 mg IV every 5 min | 25–100 mg PO bid or tid |
max 15 mg | ||
Propranolol | 1 mg IV every 2–5 min | 10–80 mg PO tid or qid |
max 0.1–0.2 mg/kg | ||
Calcium-channel antagonists | ||
Verapamil | 5–10 mg IV over 1–2 min | 5 μg/kg/min IV or 40–160 mg PO tid |
Diltiazem | 0.25 mg/kg IV over 2 min | 5–15 mg/h IV or 30–90 mg PO qid |
Digitalis | ||
Digoxin | 0.25–0.5 mg IV, then | 0.125–0.25 mg/day |
0.25 mg every 4–6 h | ||
max 1 mg/day | ||
Conversion of postoperative AF is not needed in the majority of patients after cardiac surgery because of high recurrence rate and self-limited nature. However, this approach may be useful in high-risk patients who are refractory to or intolerant of atrioventricular (AV) nodal blocking agents. Conversion of AF, AFL, and AT can be accomplished using electrical cardioversion, pharmacological cardioversion, and overdrive pacing (if AFL or AT present). Pharmacological cardioversion should be considered in the setting of unstable respiratory status or other contraindication for anesthesia. Drugs proven to be useful for cardioversion include procainamide, amiodarone, propafenone, ibutilide, and dofetilide. Latter two agents carry a risk of torsades de pointes about 2–4 % (VanderLugt et al. 1999). This risk is higher in the setting of bradycardia, female gender, hypokalemia, and hypomagnesemia. Rapid atrial pacing using epicardial wires implanted during surgery was proved to be safe and effective in conversion of postoperative AFL and AT. Rapid atrial pacing is highly desirable in the patients unsuitable for electrical cardioversion such as patients with chronic obstructive pulmonary disease. Electrical cardioversion is reserved for patients exhibiting acute hemodynamic instability. For elective cardioversion, anterior-posterior paddles are preferred with the posterior paddle placed at the lower tip of the scapula. It has been shown that there is a higher risk of stroke in cardiac surgery patients with AF. Accordingly, anticoagulation with heparin or oral anticoagulation is appropriate when AF persists longer than 48 h, as recommended for nonsurgical patients (Fuster et al. 2011). The duration of anticoagulation must be based on individual clinical situation.
9.2 Ventricular Arrhythmias
9.2.1 Incidence and Prognosis
New-onset ventricular arrhythmias (VA) are uncommon after cardiac surgery (El-Chami et al. 2012). The highest incidence was observed between 3 and 5 postoperative days (Brembilla-Perrot et al. 2003). The prognosis of postoperative VAs is highly dependent on the type of arrhythmia and the severity of structural heart disease. Patients with simple premature ventricular complex (PVC) usually exhibit a benign prognosis (Huikuri et al. 1990). Complex ventricular arrhythmias, including frequent PVC and nonsustained ventricular tachycardia (VT), have no effect on short-term prognosis but predict a poor long-term prognosis if ventricular function is impaired (Smith et al. 1992; Pinto et al. 1996). The occurrence of sustained VT (Fig. 9.2) always predicts a poor short- and long-term prognosis (Tam et al. 1991). Traditionally, early (<48 h) postoperative VA was considered to have little if any long-term prognostic value and should be ignored after treating the acute episode. Recently, this traditional notion has been challenged by recent data indicating that VAs occurring within 48 h of cardiac surgery resulted in similar long-term outcomes as those occurring >48 h after surgery (El-Chami et al. 2012).