Coronary computed tomographic angiography allows direct evaluation of the vessel wall and thus positive remodeling, which is a marker of vulnerability. The purpose of this study was to assess the association between positive remodeling on computed tomography angiogram (CTA) and vulnerable plaque characteristics on virtual histologic intravascular ultrasound (VH IVUS) images. Forty-five patients (78% men, 58 ± 11 years old) underwent computed tomographic angiography followed by VH IVUS. On CTA, the remodeling index was determined for each lesion by a blinded observer using quantitative analysis. Positive remodeling was defined based on a remodeling index ≥1.0. Percent necrotic core and presence of thin-capped fibroatheroma (TCFA) were used as markers for plaque vulnerability on VH IVUS images. Ninety-nine atherosclerotic plaques were evaluated, of which 37 lesions (37.4%) were identified as having positive remodeling on CTA. Higher levels of plaque vulnerability were identified in lesions with positive remodeling compared to lesions without positive remodeling. Percent necrotic core was significantly higher in lesions with positive remodeling (15.7 ± 7.8%) compared to lesions without this characteristic (10.2 ± 7.2%, p <0.001). Furthermore, significantly more TCFA lesions were identified in positively remodeled lesions (n = 16, 43.2%) than in lesions without positive remodeling (n = 3, 4.8%, p <0.001). In conclusion, lesions with positive remodeling on CTA are associated with increased levels of plaque vulnerability on VH IVUS images including a higher percent necrotic core and a higher prevalence of TCFA. Thus evaluation of remodeling on CTA may provide a valuable marker for plaque vulnerability.
Noninvasive coronary computed tomographic angiography has emerged as a promising procedure to detect coronary atherosclerosis. The technique allows for direct evaluation of the coronary artery vessel wall, thus enabling to some extent noninvasive evaluation of plaque structure and composition. Because of technical restrictions, computed tomographic angiography cannot provide detailed visualization of fibrous cap thickness or necrotic core size. However, presence of positive remodeling, which is an important surrogate marker of vulnerability, can be reliably assessed. Moreover, previous studies have demonstrated a relation between positive remodeling assessed on computed tomographic angiogram (CTA) and presentation with acute coronary syndrome (ACS). However, direct comparison of plaque remodeling on CTA and plaque characteristics on virtual histologic intravascular ultrasound (VH IVUS) image has not yet been performed. The purpose of this study was to assess the association between positive remodeling on CTA and vulnerable plaque characteristics on VH IVUS image.
Methods
The patient population consisted of 45 patients who underwent computed tomographic angiography and invasive coronary angiography in combination with VH IVUS. Patients were clinically referred for computed tomographic angiography because of known or suspected coronary artery disease, which was followed by invasive coronary angiography and VH IVUS. Referral for invasive coronary angiography was based on clinical presentation and/or imaging results. VH IVUS was performed to further evaluate the extent and severity of disease to determine further management more precisely and elucidate possible discrepancies between noninvasive and invasive angiographic findings. Contraindications for computed tomographic angiography were (1) (supra)ventricular arrhythmias, (2) renal insufficiency (glomerular filtration rate <30 ml/min), (3) known allergy to iodinated contrast agents, (4) severe claustrophobia, and (5) pregnancy. Exclusion criteria for IVUS were severe vessel tortuosity, severe stenosis, or vessel occlusion. Risk factors for coronary artery disease were derived from existing patient medical record data. For this retrospective evaluation, patients with good to moderate image quality on CTA and available quantitative analyses were selected from an ongoing registry.
Computed tomographic angiography was performed using a 64-detector row (n = 34) helical scanner or a 320-detector row (n = 11) volumetric scanner (Aquilion 64 or Aquilion ONE, Toshiba Medical Systems, Otawara, Japan) as previously described. Patients with an increased heart rate (≥65 beats/min) were administered β blockers (oral metoprolol 50 or 100 mg, single dose, 1 hour before examination) if not contraindicated. Unless contraindicated, nitroglycerin 0.4 mg sublingually was administered immediately before contrast injection. During computed tomographic angiographic examination mean heart rate was 57 ± 8 beats/min. An initial dataset was reconstructed at 75% of the RR interval, with a slice thickness of 0.50 mm and a reconstruction interval of 0.25 mm. For motion artifacts, additional reconstructions were explored to obtain images with most optimal image quality for evaluation. For processing and evaluation, computed tomographic angiographic data were transferred to an off-line workstation.
VH IVUS examinations were performed during invasive coronary angiography. Invasive coronary angiography was performed according to standard protocols. Patients were administered intracoronary nitroglycerin before induction of the IVUS catheter (Eagle Eye, Volcano Corporation, Rancho Cordova, California). The ultrasound catheter was positioned in the coronary artery, and motorized pullback at a speed of 0.5 mm/s was used until the catheter reached the guiding catheter. VH IVUS data were stored digitally and assessed offline.
Computed tomographic angiographic examinations were evaluated by an independent and experienced observer who was blinded to VH IVUS results, using a dedicated and extended version of QAngio CT 1.1 (Medis Medical Imaging Systems, Leiden, the Netherlands). On computed tomographic angiographic datasets, dedicated software was used to detect lumen and vessel wall contours. According to the modified American Heart Association classification, coronary arteries were divided into 17 segments. Only segments that were available on VH IVUS image and CTA were analyzed. Coronary plaques were defined as structures >1 mm 2 within and/or adjacent to the coronary artery lumen, which could be clearly distinguished from the vessel lumen. Per-segment coronary plaque was selected at the site of most severe luminal narrowing. Detected lumen and vessel wall contours were used for automated quantitative measurements of coronary plaques. At the level of the minimal lumen area, the remodeling index (RI) was calculated by dividing the cross-sectional vessel wall area by the corresponding reference area. The cross-sectional reference area was determined in the normal-appearing reference area as close as possible to the respective coronary lesion. Presence of positive remodeling was defined as an RI ≥1.0.
VH IVUS analysis was performed by 2 experienced observers who were blinded to baseline patient characteristics and computed tomographic angiographic results, using dedicated software (pcVH2.1, Volcano Corporation). The previously described 17-segment model was used to ensure that similar plaques were analyzed with computed tomographic angiography and VH IVUS. Side branches and coronary ostia were used as anatomic markers.
For each lesion identified on CTA and VH IVUS image, minimal lumen area and corresponding vessel area were determined. In addition, percent plaque burden was calculated as plaque cross-sectional area divided by vessel cross-sectional area multiplied by 100. Four different plaque components, namely fibrotic tissue, fibrofatty, necrotic core, and dense calcium, were differentiated into different color codes. Different plaque components were calculated as percent plaque burden. Plaque type was determined on VH IVUS image using a classification based on differentiation of the 4 plaque components as described previously. Four different plaque types were identified, namely pathologic intimal thickening, fibroatheroma, fibrocalcific plaque, and thin-capped fibroatheroma (TCFA). TCFA lesions were defined as lesions with a plaque burden ≥40%, presence of confluent necrotic core >10%, and no evidence of an overlying fibrous cap. Percent necrotic core and presence of TCFA were used to determine plaque vulnerability on VH IVUS image.
Statistical analysis was performed using SPSS 18.0 (SPSS, Inc., Chicago, Illinois). Continuous data are presented as mean ± SD. Categorical data are expressed as absolute numbers or percentages. Segments available on CTA and VH IVUS image were included in the lesion-based analysis. Plaque vulnerability on VH IVUS image (defined by percent necrotic core and presence of TCFA) was assessed in lesions with positive remodeling (RI ≥1.0) on CTA and compared to the remaining lesions that did not show positive remodeling (RI <1.0) on CTA. Comparisons were performed by chi-square analysis. A p value <0.05 was considered statistically significant.
Results
Forty-five patients (78% men, 57.8 ± 11 years old) who underwent computed tomographic angiography followed by VH IVUS were enrolled retrospectively. Characteristics of the patient population are presented in Table 1 .
| Age (years) | 58 ± 11 |
| Men/women | 35/10 |
| Heart rate during coronary computed tomographic angiography (beats/min) | 57 ± 8 |
| Stable angina/suspected acute coronary syndrome | 27/18 |
| ≥1 coronary stenosis with >50% diameter narrowing on invasive coronary angiogram | 32 (71%) |
| Number of diseased vessels | |
| 1 | 17 (53%) |
| 2 | 6 (19%) |
| 3 | 9 (28%) |
| Cardiovascular risk factors | |
| Diabetes mellitus | 10 (22%) |
| Hypertension ⁎ | 29 (64%) |
| Hypercholesterolemia † | 26 (58%) |
| Current smoker | 20 (44%) |
| Obesity ‡ | 8 (18%) |
⁎ Systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg or use of antihypertensive medication.
† Serum total cholesterol ≥230 mg/dl or serum triglycerides ≥200 mg/dl or treatment with lipid-lowering drugs.
In all patients computed tomographic angiographic and VH IVUS studies were of sufficient imaging quality for analysis.
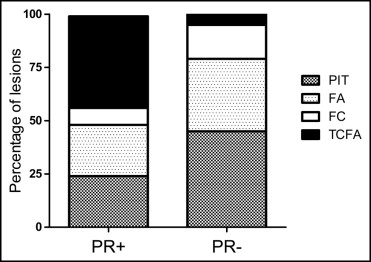
Ninety-nine plaques were identified on CTA and corresponding available VH IVUS analyses. Of theses 99 atherosclerotic plaques, 37 lesions (37.4%) were classified as positively remodeled (RI ≥1.0) on CTA. In the remaining 62 lesions (62.6%) no positive remodeling (RI <1.0) was observed. On VH IVUS image the most prevalent plaque component was fibrotic tissue (52% ± 16%), followed by fibrofatty tissue (19% ± 12%), necrotic core (13% ± 8%), and dense calcium (8% ± 9%). Qualitative evaluation of coronary lesions on VH IVUS image revealed the presence of pathologic intimal thickening, fibroatheroma, and fibrocalcific lesions in 37 (37.4%), 30 (30.3%), and 13 (13.1%) of lesions, respectively. TCFAs were identified in 19 lesions (19.2%).
Lesions identified as positively remodeled (RI ≥1.0) on CTA had a significantly higher plaque burden on VH IVUS image compared to lesions without positive remodeling (RI <1.0) as presented in Table 2 . Percent necrotic core was also significantly higher in positively remodeled lesions (RI ≥1.0) compared to lesions without positive remodeling (RI <1.0). No differences in presence or absence of positive remodeling on CTA were observed in percent fibrotic tissue, fibrofatty tissue, and dense calcium.
| Plaque Characteristics on VH IVUS Image | Presence of Positive Remodeling on CTA | Absence of Positive Remodeling on CTA | p Value |
|---|---|---|---|
| Minimal lumen area (mm 2 ) | 8 ± 4 | 9 ± 5 | 0.38 |
| Vessel area (mm 2 ) ⁎ | 16 ± 6 | 15 ± 6 | 0.24 |
| Plaque burden (%) | 51 ± 10 | 41 ± 16 | <0.001 |
| Fibrotic (%) | 55 ± 9 | 51 ± 19 | 0.18 |
| Fibrofatty (%) | 20 ± 11 | 18 ± 13 | 0.58 |
| Necrotic core (%) | 16 ± 8 | 10 ± 7 | 0.001 |
| Dense calcium (%) | 9 ± 6 | 7 ± 11 | 0.25 |
Qualitative evaluation of plaque types, as shown in Figure 1 , revealed an equal distribution of the presence of fibroatheroma (9, 24%, vs 21, 34%, p = 0.32) between lesions with positive remodeling (RI ≥1.0) and lesions without positive remodeling (RI <1.0). Furthermore, no significant difference in presence of fibrocalcific plaques (3, 8%, vs 10, 16%, p = 0.36) were observed between the 2 groups. Pathologic intimal thickening was significantly more often observed in lesions without positive remodeling (RI ≥1.0) on CTA; 28 lesions (45%) without positive remodeling (RI <1.0) on CTA were classified as showing pathologic intimal thickening compared to 9 lesions (24%) with positive remodeling (RI ≥1.0) on CTA (p = 0.04). Importantly, as shown in Figure 1 , 16 lesions (43.2%) with positive remodeling (RI ≥1.0) on CTA were identified as TCFAs. In contrast, only 3 lesions (4.8%) without positive remodeling (RI <1.0) on CTA were classified as TCFAs (p <0.001). An example of a lesion with positive remodeling (RI ≥1.0) on CTA and corresponding findings on VH IVUS image is provided in Figure 2 .