22
Police, firefighters and the military
Police, firefighters and military personnel may be exposed to pulmonary toxins and irritants, placing them at risk for the development of acute and chronic respiratory disease. While each profession is distinct, potential exposures overlap significantly. The first section of this chapter addresses potential exposures for all three professions in their capacity as first responders. The remainder of the chapter considers exposures more unique to each of the three professions.
Sources for each exposure are discussed along with relevant historical aspects. Pathophysiological mechanisms are addressed in conjunction with clinical presentation. Primary prevention is discussed in varying detail, although due to the uncontrolled nature of the environments in which police, firefighters and military personnel work, administrative and engineering controls are often not possible and personal protective equipment (PPE) may be the sole preventative measure. Secondary prevention, in the form of medical surveillance, is touched upon where relevant. Treatment and prognosis are also described.
22.2 First responders: potential exposures common to police, firefighters and the military
Police, firefighters and military personnel act as first responders to threats involving public safety and security. Potential exposures include acute chemical emergencies (chemical weapons and hazardous materials), biological hazards and fire smoke. The World Trade Center (WTC) disaster on 11 September 2001 exposed emergency response personnel to a novel and complex mixture of smoke and hazardous dusts. A large proportion of first responders to the WTC disaster developed a variety of respiratory problems, some of which are unique to this population. As such, respiratory disease in WTC responders is considered as a distinct topic in this chapter.
22.2.1 Chemical weapons and hazardous materials
Exposure to chemical weapons may occur during terrorist attacks or warfare. Chemical warfare agents include crowd control agents, chlorine, sulfur mustard (SM), phosgene and nerve agents. Hazardous material exposure can result from industrial disasters, recreational mishaps and natural catastrophes. Hazardous materials incidents involve a wide variety of chemical hazards, with clandestine drug laboratories posing unique risks.
Most chemical weapons and hazardous material incidents involve exposure to strong irritants. The clinical effects of exposure are dependant on concentration, duration of exposure, the water content of exposed tissues and individual characteristics of the exposed victim. Agents with high water solubility (crowd control agents, chlorine, ammonia) predominantly affect exposed mucous membranes and upper airways, while those with lower water solubility (SM, phosgene) penetrate to the small airways and alveoli. Table 22.1 delineates these exposures by source, water solubility and mechanism of toxicity.
Table 22.1 Respiratory irritants and toxicants; sources, solubility and mechanisms of injurya
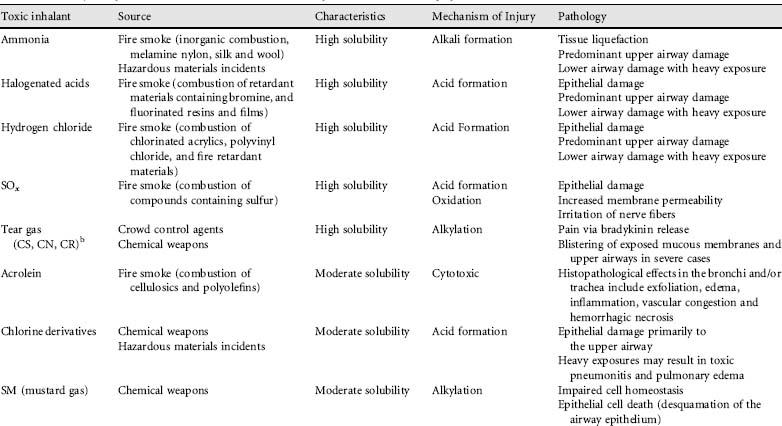
aInternational Programme on Chemical Safety (IPCS). INCHEM. Concise International Chemical Assessment Documents (CICADs).
bCS, o-chlorobenzylidene malononitrile; CN, chloroacetophenone (CN); CR, dibenzoxazepine.
The basic management of acute chemical exposures involves cessation of exposure and aggressive supportive measures as needed. The former is accomplished by early decontamination (ideally prior to hospital transport). Clothing removal eliminates 85-90% of trapped chemical substances, and should be followed by soap and water decontamination. Clinical signs of severe chemical injury include altered mental status, cardio-respiratory manifestations, unconsciousness and convulsions. Initial supportive care should focus on airway patency, ventilation and circulation, while surveying the patient for burns, trauma and other injuries.
Chemical weapons
Crowd control agents are a unique form of chemical weapon to which first responders, and police in particular, are exposed. The most commonly used crowd control agents are o-chlorobenzylidene malononitrile (CS), chloroacetophenone (CN) and dibenzoxazepine (CR). While colloquially referred to as ‘tear gas’, these agents are actually aerosolized powders. Eye and upper airway symptoms typically occur within 30 seconds of exposure and persist for up to 30 minutes post-exposure. Severe exposure may cause laryngospasm and bronchospasm, especially in persons with pre-existing respiratory disease such as asthma or bronchitis. Effects are usually self-limited, although they may persist longer in cases of high exposure (such as in enclosed spaces) or in individuals with underlying lung disease. In general, long-term prognosis is excellent; however, reactive airways dysfunction syndrome (RADS) and other sequelae have been reported in select cases.
Chlorine gas, an irritant with intermediate solubility, was first used as a weapon in World War I in the Second Battle of Ypres, on 22 April 1915. Its use in World War I as a chemical weapon declined with the advent of phosgene and SM. Today, chlorine is ubiquitous as both an industrial chemical and disinfectant. Among hazardous materials incidents, accidental releases of chlorine compounds are second only to those involving ammonia. Chlorine gas causes upper and lower airway damage via its conversion to hydrochloric and hypochlorous acids. Low concentrations are scrubbed out in the upper airways, while higher exposures (>50 ppm) penetrate more deeply, causing acute lung injury and potential long-term respiratory complications. Even with severe exposures, mortality is low and long-term prognosis is good. Pulmonary symptoms usually resolve within 1-2 months, although there have been case reports of persistent obstructive disease, restrictive disease and RADS. Smokers and those with chronic chlorine exposure are most susceptible to persistent respiratory sequelae. Treatment is supportive (bronchodilators and steroids in severe cases). Nebulized sodium bicarbonate may be of benefit in select cases.
SM, the most widely used chemical weapon in the past century, is a vesicant or ‘blistering’ agent known as mustard. SM predominantly causes skin and eye injuries, but can also affect the conducting airways and adjacent alveoli. The mechanism of action of SM involves DNA and protein alkylation, causing cell death. The result is desquamation of the airway epithelium and a generalized inflammatory response. Mortality rates are low, although subsequent morbidity (eye, skin and respiratory) is common and often significant. Long-term respiratory complications from SM exposure include interstitial fibrosis, chronic obstructive pulmonary disease (COPD), bronchiectasis and bronchiolitis obliterans. Bronchiectasis and pulmonary fibrosis are usually confined to the lower lobes. Victims can also develop an SM-induced asthma. Treatment is supportive, including antibiotics for superinfection and selective use of steroids to prevent progression of fibrosis.
Phosgene (carbonyl chloride) was the most lethal chemical weapon used in World War I, causing an estimated 80% of poison gas deaths. Today, phosgene is a widely used industrial chemical. Its low water solubility allows it to penetrate to the distal respiratory units of the lung parenchyma. Phosgene causes diffuse injury by directly damaging cellular elements of the respiratory tract and triggering a cytokine-induced inflammatory cascade. Moderate to high exposures (>3 ppm) cause a triphasic response. The initial ‘reflex’ phase occurs when sensory receptors initiate a vagal reflex which leads to rapid shallow breathing. An asymptomatic second ‘latent’ phase characterized by increased pulmonary capillary permeability may then ensue after a period of up to 30 hours. In severe cases, victims progress to a third phase: adult respiratory distress syndrome. Radiographic evidence of early pulmonary edema may begin as early as 7-8 hours post-exposure, showing blurred enlargement of the hila and ill-defined patches or strip shadows in the central portions of the lung. Treatment is supportive, often requiring positive airway pressure ventilation. Diuretics should be avoided as pulmonary edema is due to capillary leak, which can lead to a relative vascular hypovolemia. While no specific antidote for phosgene exposure exists, steroids and ibuprofen have been used with some success. The long-term prognosis is generally good for victims surviving the initial stages of disease, although an obstructive pattern compatible with chronic bronchitis, emphysema or RADS on pulmonary function testing may persist for months to years.
The chemical weapons sarin, soman, tabun and VX are organophosphorous compounds often referred to as ‘nerve agents’ because they inhibit acetylcholinesterase, resulting in cholinergic overstimulation. Cholinergic overstimulation presents with muscarinic and nicotinic effects. Muscarinic symptoms include profuse exocrine secretions, miosis, headache and eye pain. Nicotinic symptoms include skeletal muscle weakness, fasciculations and paralysis. While primarily systemic toxins, mortality from nerve agent exposure usually results from respiratory compromise due to hypersecretions, bronchoconstriction, thoracic weakness and decreased respiratory drive. Treatment is predicated upon diagnosing the clinical cholinergic toxidrome. Measuring erythrocyte and serum cholinesterase levels is confirmatory, although results are not available rapidly enough to be useful, and treatment should not be delayed for purposes of laboratory confirmation. Supportive treatment consists of supplemental oxygen, suctioning of secretions and, in severe cases, mechanical ventilation. Benzodiazepines are used as anticonvulsants, and are the only effective anticonvulsant drugs in the context of nerve agent poisoning. Two specific antidotes exist: (1) atropine competitively blocks the action of acetylcholine at muscarinic receptors; (2) pralidoxime and other ‘oximes’ reactivate acetylcholinesterase and work at nicotinic, muscarinic and central nervous system receptors.
Hazardous materials
Hazardous materials comprise a wide range of physical, chemical and biological hazards in a variety of settings. Most hazardous material incidents do not result in chemical exposure victims. Incidents that do result in casualties usually involve irritants such as chlorine derivatives, ammonia, phosgene and other corrosive substances. The mechanisms of injury, clinical presentation, treatment and prognosis are the same as described for irritant chemical weapons. In events involving fires and explosions, thermal injury and exposure to fire smoke can also cause significant injury. Fire smoke is discussed below.
Organophosphorous and carbamate pesticides may also be released during chemical accidents. These substances are cholinesterase inhibitors with effects analogous to those of the nerve agent chemical weapons. The resulting cholinergic toxidrome and its treatment are similar to those described for nerve agents. The major difference between cholinesterase-inhibiting pesticides and weaponized nerve agents is the time course of symptoms. Pesticides tend to have a slower onset but longer duration of action. As such, supportive care for cholinesterase-inhibiting pesticide exposure is usually longer, and the cumulative dosage of atropine required greater, than is required for exposure to the weaponized nerve agents.
A unique set of toxins encountered by first responders and law enforcement personnel are those produced in clandestine drug laboratories. Potential exposures include lead oxide, aluminum hydroxide, mercury vapor, iodine, phosphine, yellow phosphorus, hydrogen chloride and anhydrous ammonia. While some of these agents have the potential to cause serious systemic toxicity, respiratory irritation is the most common acute symptom and long-term sequelae may include persistent cough, wheeze, breathlessness, bronchitis, chest colds, pneumonia, chronic bronchitis and emphysema.
Primary prevention for personnel responding to chemical weapons or hazardous materials releases requires provision and instruction in the use of appropriate PPE. Administrative controls include written protocols addressing the order in which responders enter buildings and the PPE they should wear. Secondary prevention should include periodic medical assessments, including spirometry. In the event of phosgene, SM or chlorine gas exposure, patients should have ongoing medical surveillance to ensure optimization of therapy in cases of residual airway hyperreactivity, and to rule out the development of pulmonary fibrosis.
Existing evidence indicates that hazardous material (HAZMAT) procedures and personal protective equipment are effective, with the literature reporting that HAZMAT responders do not lose pulmonary function at an accelerated rate compared with their non-HAZMAT firefighting counterparts.
Bacterial pathogens can be disseminated as aerosols for use in biological warfare or acts of terrorism. Biological agents with the potential to be weaponized include bacteria, viruses and biologically derived toxins. Although the pathological endpoints for most biological weapons are systemic, victims may present with isolated respiratory symptoms.
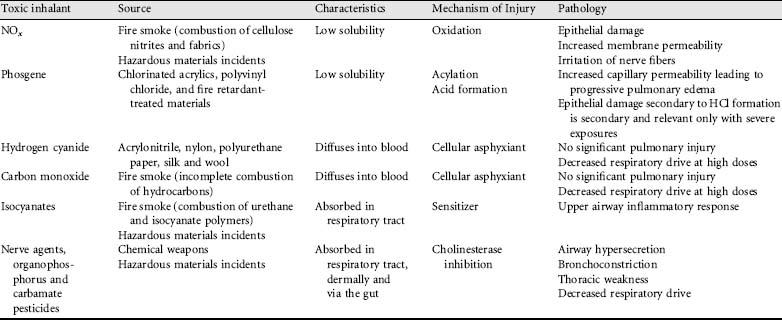
The United States Centers for Disease Control and Prevention (CDC) has identified, and placed in priority order according to likelihood of weaponization, those biological agents thought to pose a risk for use as biological weapons. Category A represents agents considered to be of highest priority (agents already weaponized or with high likelihood to be weaponized in the future), while Category C represents agents of low priority (emerging diseases or agents that may be weaponized in the future). The essentials for diagnosis and management of the primary potential biological weapons of interest (respiratory anthrax, plague, tularemia, brucellosis, glanders and Q fever) are summarized in Table 22.2. Suspected infection with any of these agents requires immediate work-up because rapid diagnosis is vital to enable identification of index cases, manage potential outbreaks and prevent further exposures. An in-depth discussion of these specific biological agents is beyond the scope of this chapter, although some general aspects of presentation regarding each is worth mention.
Table 22.2 Bioterrorism agents
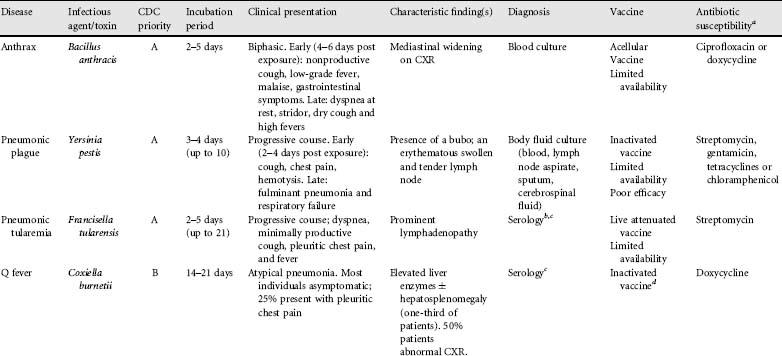
aResistance may occur; consult current recommendations prior to use.
bTularaemia serologic tests may cross-react with Salmonella, Brucella, Yersinia and Legionella species.
cBlood culture difficult/unreliable means of diagnosis.
dDo not give to previously infected individuals. Pre-vaccination screening.
Anthrax has been of greatest concern to date, with documented attacks having already occurred. Anthrax presents with a biphasic course, and distinguishes itself from influenza and other viral illnesses because of early dyspnea, gastrointestinal upset, lack of rhinorrhea and sore throat. Mediastinal widening on chest imaging is characteristic.
Pneumonic plague is the least common form of plague, after bubonic and primary septicemic plague. Pneumonic plague initially presents as a flu-like illness. The presence of a bubo, an erythematous swollen and tender lymph node, is characteristic of infection. Recognized and appropriately treated, the prognosis for pneumonic plague is good, although multidrug resistant strains exist so susceptibility testing is recommended.
Pneumonic tularemia is characterized by marked respiratory symptoms, with most victims developing prominent lymphadenopathy and a nonspecific secondary rash in select cases. Pleuritic chest pain and fever may also be noted upon presentation.
Acute Q fever may present as an atypical pneumonia. Most individuals with Q fever are asymptomatic; only 50% show radiographic evidence of pneumonia and only 25% develop pleuritic chest pain. Elevated liver enzymes with or without evidence of hepatosplenomegaly are seen in up to one-third of cases. Diagnosis is based on serology.
Brucellosis in humans is caused by four different species of Brucella. Brucella suis was the first biological agent weaponized by the USA in 1954. Brucella has a long incubation period of 2-4 weeks. Most symptoms are systemic (general malaise and gastrointestinal); only 20% of patients present with cough and pleuritic chest pain, and acute pneumonia is unusual.
Glanders is caused by Burkholderia mallei bacteria, which exists primarily in horses. Inhalational exposure may cause pneumonia, pulmonary abscesses and pleural effusions. Progression to septicemia can be fatal in 7-10 days. Human infection with B. mallei is extremely rare and the diagnosis should prompt suspicion of a malicious source of the infection.
Staphylococcal enterotoxin B, Clostridium perfringens-toxin and ricin are biotoxins with the potential to be weaponized. Staphylococcal enterotoxin B causes a syndrome of fever, nausea and diarrhea. Clostridium perfringens-toxin, if aerosolized, can result in acute lung injury. Ricin intoxication, although usually manifesting with gastrointestinal hemorrhage after ingestion or muscle necrosis after intramuscular injection, can also cause acute pulmonary disease after inhalation.
In summary, while most potential biological warfare agents produce systemic infections, pulmonary manifestations may be significant. Respirator selection is complicated and differs depending on the agent’s physical characteristics, concentration, infectious dose and mode of dispersion. Use of a self-contained breathing apparatus (SCBA) is recommended for responders to a suspected bioaerosol attack, while a high efficiency particulate (HEPA) filter equipped respirator is usually adequate for bioaerosols disseminated by letter or package. Many biological and chemical warfare agents can be absorbed dermally, so full contact precautions and facilities and training for rapid and effective decontamination are necessary.
22.2.3 Other respiratory infections
First responders come into direct contact with the general public in uncontrolled environments, which predisposes them to respiratory infections. Police frequently interact with people living in shelters or on the street and incarcerated criminals, and transport persons who are in custody. Firefighters may be exposed during provision of emergency medical services. Military personnel live in close quarters and, while deployed overseas for humanitarian or combat duties, are exposed to populations affected by social disruption, poor hygiene and crowded conditions. Common viral infections are the most prevalent respiratory infections to which police, firefighters and military personnel are exposed placing them increased risk of upper respiratory tract infections (URTIs). Tuberculosis (TB) and emerging respiratory infections, such as severe acute respiratory syndrome (SARS) and avian influenza, are also significant concerns.
URTIs, although rarely serious health threats, can significantly impact operational capabilities, accounting for a large proportion of absenteeism and adversely affecting emergency preparedness. Emergency personnel may also spread infections to susceptible persons in the communities they serve. An additional concern is that infection may debilitate first responders in general, making them more susceptible to other, more severe, forms of disease. For example, it has been postulated that increased rates of influenza may explain the higher rates of on-duty coronary heart disease deaths in firefighters during the winter months. Preventative immunizations should be aggressively promoted, in particular for influenza and pertussis. Self-reporting of symptoms, frequent hand washing and general hygiene measures must also be encouraged.
Tuberculosis remains a common disease with inner city, incarcerated and developing world populations having the highest risk. Increased conversion rates have been demonstrated in military personnel involved in humanitarian and refugee operations, and it is expected that police and firefighters are also at increased risk due to their contact with institutionalized and marginalized populations. Primary prevention in cases of known or suspected contact with infected persons requires National Institute for Occupational Safety and Health (NIOSH) approved HEPA respirators with filters classified as N95 being the minimum acceptable level. A complete respirator protection program requiring periodic fit testing should be in place. Secondary prevention should include screening first responders for TB, timely reporting of cases, initiation of isoniazid or other approved chemoprophylaxis for converters in accordance with existing guidelines and ensuring compliance with therapy.
First responders are also called upon to deal with outbreaks of novel infectious disease. The most prominent recent example was the SARS outbreak of 2003. During an outbreak, first responders may transport infected individuals or help to enforce quarantine requirements. Provision and training in the use of respiratory protection is vital. While there is now compelling evidence that SARS is transmitted by contact or droplet transmission, cases were documented of healthcare workers who contracted the disease despite droplet precautions. Thus, properly fit tested N95 respirators in conjunction with universal precautions are recommended in the event of the reemergence of SARS or an avian influenza outbreak.
22.2.4 World trade center disaster and occupational lung disease
On 11 September 2001, the collapse of the WTC intensely exposed an unprecedented number of emergency response personnel to a complex mixture of smoke and hazardous dusts. RADS, ‘WTC cough’, new-onset asthma, gastroesophageal reflux disease and sarcoidosis have all been linked to exposures occurring in workers involved in the immediate response and clean-up of the disaster.
A detailed exposure assessment for first responders to the WTC disaster is difficult, although studies on the subject report an aggregate consisting of polycyclic aromatic hydrocarbons, polychlorinated biphenyls, organochlorine pesticides, vermiculite, plaster, synthetic foam, asbestos, glass fibers and fragments, calcium sulfate (gypsum) and calcium carbonate (calcite). The exact mechanisms of WTC dust toxicity remain unresolved, but the alkaline and corrosive nature of the dust seems to have caused acute upper respiratory tract irritative symptoms and persistent hyper-reactivity with airway dysfunction. It has also been postulated that inflammation was triggered by high exposure to fine and ultrafine particulate matter.
‘WTC cough’ refers to complaints of a severe, persistent, nonasthmatic cough and dyspnea in exposed individuals in the months following the WTC disaster. The case definition specifies symptoms that are debilitating enough to require affected individuals to have taken at least 4 weeks of medical leave and onset of symptoms to have occurred within 6 months of exposure. A dose-response relationship has been observed in affected individuals.
New-onset asthma has also been observed in first responders to the WTC disaster, with a dose-response relationship suggested by the finding that responders exposed to the initial cloud of dust and debris were more than twice as likely to report newly diagnosed asthma compared with unexposed individuals.
Gastroesophageal reflux disease (GERD) has been closely associated with WTC cough with the majority of firefighters with ‘WTC cough’ also reporting new onset GERD. Interesting, a dose-response relationship has also been demonstrated with earlier arrival to the scene being predictive of more severe disease. The etiology and significance of this is not completely understood, although GERD is known to both cause and aggravate respiratory symptoms such as laryngitis, asthma and chronic cough.
Sarcoid-like granulomatous pulmonary disease has been recognized in New York City firefighters. This association is discussed further below.
Police are not routinely exposed to respiratory hazards, although significant exposures may occur while responding to vehicular accidents, natural disasters and crime scenes. Crowd control agents also pose respiratory risks, as can chemicals used in forensic investigation.
22.3.1 Epidemiology of respiratory disease in police workers
Epidemiologic studies reveal the prevalence of lung disease in police to be lower than that of the general population. Notable exceptions are an increased prevalence of occupational asthma in police working in forensic identification, and the potential for increased risk of respiratory infections resulting from frequent contact with the general public and high-risk populations. Concern has also been expressed over the potential health effects of exposure to vehicular exhaust in police working in traffic-related positions.
22.3.2 Respiratory exposures in police workers
Occupational asthma has been reported in police forensics workers. Forensic identification involves a wide variety of chemicals, primarily irritants, and certain known sensitizers. Police involved in forensic identification have been found to have a significantly higher prevalence of respiratory symptoms compared with matched controls working in other fields. Cyanoacrylate, a known sensitizer, is used to uncover fingerprints and has been postulated as the most likely cause of occupational asthma in this population. Primary prevention for forensics workers should include respiratory protection and periodic health assessments with spirometry. In cases where sensitization has occurred, removal from the exposure and continued medical surveillance should be conducted to prevent the development of persistent bronchial hyperreactivity.
Police officers may be exposed to TB as a result of their frequent dealings with atrisk populations such as current and former prisoners, the homeless and intravenous drug users. Although it is widely recognized as a potential occupational hazard, the literature does not offer much insight regarding the incidence and prevalence of TB in police. Similar to healthcare workers, secondary prevention using annual TB skin testing is recommended for police officers who have frequent contact with at risk populations.
Several studies have examined whether police workers who frequently perform traffic-related duties are at increased risk for respiratory disease. The literature does not suggest increased respiratory symptoms in most police workers exposed to vehicular exhaust, except perhaps in exceptional circumstances. The only study of note that demonstrated significant effects involved heavily exposed officers in Bangkok. These officers reported significantly more cough and had lower FEV1 measurements than their occupationally nontraffic-exposed controls.
22.3.3 Respiratory cancer in police workers
Slightly elevated rates of lung cancer have been reported in police, although these results have been attributed to greater cigarette smoking in this population. Forensic work involves the use of some known chemical carcinogens, but evidence of increased cancer among police working in forensics doing fingerprint work is lacking. Vehicular exhaust has not been linked to an increased risk of respiratory cancer among police workers (Table 22.3).
Table 22.3 Respiratory diseases associated with police work
| Disease | Associated exposures |
| Infection | Community acquired infections Tuberculosis |
| Asthma | Cyanoacrylate (used in forensics) |
| Lung cancer | Elevated rates of tobacco smoking Chemicals used in forensics (e.g. Gentian Violet) |
The act of firefighting consists of four stages: break-in/breach of the burning structure; rescue operations; fire suppression; and overhaul and salvage. Overhaul and salvage involve firefighters checking the structure to ensure the fire is entirely extinguished and assessment of structural integrity. During fires, firefighters are exposed to a variety of pulmonary toxicants. The highest exposures occur during the initial stages of firefighting, although it is standard practice for firefighters to wear a self-contained breathing apparatus during these initial stages. During overhaul and salvage activities, respiratory protection is often not worn due to the perception that the toxicants have dissipated. In actual fact, the risks of airborne toxicant exposure remain elevated throughout these stages of firefighting.
22.4.1 Epidemiology of respiratory disease in firefighters
Historically, firefighters have shown increased rates of airway hyper-reactivity/asthma and, to a lesser extent, decreased ventilatory function (FVC, FEV1). Improved sophistication and compliance with SCBAs has lowered the risk for decreased ventilatory capacity in firefighters to a level similar to the general public, and significant impairment now appears to be limited to those with a long service history. In contrast to persistent ventilatory dysfunction, epidemiological surveys continue to show firefighters to have high rates of occupational asthma. The SENSOR program in California, a surveillance initiative recording prevalence of work-related asthma, found firefighters to have the second highest rate among considered occupations (the highest rates were observed in correctional officers). Airway hyper-responsiveness in firefighters may be acute or chronic. Acutely, firefighters may show airway hyper-responsiveness for up to 24 hours post-exposure to fire smoke. Particularly severe exposures can result in cases of chronic airway hyper-reactivity.
Sarcoidosis is more prevalent among firefighters then in the general population. Prior to 11 September 2001, the point prevalence for sarcoidosis in New York City firefighters (FDNY) was 7-13 times greater than their healthcare worker counterparts. The WTC disaster led to a further increase in the incidence of sarcoidosis among FDNY rescue workers. The etiology of these sarcoidosis cases has not been resolved, but is suspected to involve a complex gene-environment interaction. Plausible environmental factors include infections, allergens and aerosolized toxins.
Using police officers as controls, firefighters have historically had increased rates of nonmalignant respiratory disease mortality with an estimated relative risk ratio of 1.4-2.0. Improved respiratory protection and a lower incidence of structure fires appear to be lowering these standardized mortality ratios.
Wildland firefighters are a distinct group of firefighters, and tend to have an increased risk of pulmonary sequelae compared with their structural firefighting counterparts. This discrepancy is probably the result of decreased use/level of respiratory protection in these workers.
22.4.2 Respiratory exposures in firefighters
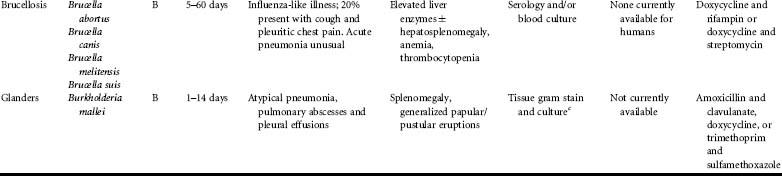
Firefighters are exposed to toxicants in fire smoke and pulverized structural elements of buildings including metals (lead, antimony, cadmium, uranium), mineral dusts, and other chemical substances (Table 22.4).
Table 22.4 Respiratory diseases associated with firefighters
| Disease | Associated exposures |
| Airway hyper-reactivity/asthma | Irritants in fire smoke: ammonia, halogenated acids, hydrogen chloride, sulfur dioxide, acrolein, oxides of nitrogen and phosgene |
| Chronic obstructive and/or restrictive impairment | Irritants in fire smoke: ammonia, halogenated acids, hydrogen chloride, sulfur dioxide, acrolein, oxides of nitrogen and phosgene |
| Sarcoidosis | Unknown: hypothesized to result from complex interaction of genetic predisposition and exposures (including mineral/metal dusts) WTC dust mixtures |
Fire smoke
Approximately 1-5% of North American firefighters’ professional time is spent fighting fires. The majority of US firefighters’ work involves the provision of emergency medical services or is nonemergency-related. Despite this, fire smoke remains one of the most significant occupational hazards facing firefighters.
Fire smoke is a complex mixture of particulate matter and toxic gases whose exact composition depends on the materials being burned, the rate and temperature of burning, and ambient oxygen levels. Smoke inhalation causes bronchopulmonary injury via four primary mechanisms: (1) hypoxic gas inhalation/oxygen deficiency; (2) thermal injury; (3) inhalation of systemic toxins/asphyxiants; and (4) inhalation of bronchopulmonary irritants.
Hypoxic gas inhalation, while acutely debilitating, does not usually directly damage the airways or pulmonary parenchyma. Thermal injury can acutely cause tracheobronchitis/ bronchiolitis and, in severe cases, asphyxiation due to laryngeal edema. Injury is usually confined to the supraglottic airways because heat exchange is rapid in the naso- and oropharynx. The exception to this is exposure to hot gases or steam which, having a greater thermal capacity than dry air, penetrate to the intrathoracic airways at temperatures high enough to cause injury. In most cases, inhalational thermal injuries occur in the hours to days following exposure with good recovery thereafter. Stricture formation in the larynx and/or trachea may occur in severe cases.
Carbon monoxide, cyanide gas and methemoglobin-forming materials may also be components of fire smoke. These agents cause tissue hypoxia with little or no direct respiratory irritation. Sequelae from chemical asphyxiant poisoning are primarily neurological and cardiac. Carbon monoxide, produced from incomplete combustion of carbonaceous materials, binds hemoglobin and cardiac myoglobin, and disrupts cytochrome oxidase. Cyanide, produced from the combustion of plastics, polyurethane, wool, silk, nylon, nitrites and rubber, binds cytochrome oxidase, blocking aerobic metabolism. Methemoglobin-forming materials enter the blood stream and oxidize ferrohemoglobin to methemoglobin. The list of potential methemoglobinforming compounds is extensive; nitrites are the most frequently encountered.
The most common irritants in smoke are ammonia, halogenated acids, hydrogen chloride and sulfur dioxide (high water solubility); acrolein (moderate water solubility); and oxides of nitrogen and phosgene (low water solubility). The mechanism of injury for each irritant may differ (Table 22.1), although with sufficient exposure all can lead to inflammation and necrosis of the lung parenchyma. Acute complications include bronchopneumonia, atelectasis, pleural effusion, pulmonary embolism and pneumothorax. Chronically, airway hyper-reactivity/RADS may occur.
In summary, most episodes of smoke inhalation do not result in lung injury, although subclinical transient declines in pulmonary function may occur. Severe exposures can result in respiratory compromise due to the combined effects of thermal injury and bronchopulmonary irritants. In patients surviving the initial complications of inhalational injury, there is usually no chronic respiratory impairment, although cases of increased airway hyper-reactivity/RADS have been documented. Chronic exposure to smoke may predispose to the development of airway hyper-reactivity. Prospective studies involving younger cohorts of firefighters have not demonstrated any decline in ventilatory function due to chronic smoke inhalation. Decreased pulmonary function tends to be marginal, with smoking history playing the predomi-nant role in most cases.
Metals
Exposure to aerosolized metals may result from the burning of painted surfaces, such as materials coated with leaded paint, and firefighters have been shown to have blood lead levels slightly above that of the general population, although frank heavy metal toxicity is rarely an issue.
Mineral dusts
Firefighters may be exposed to minerals including asbestos and silica from the pulverization of structural materials after a building collapses, and fire smoke may act as a vehicle for these exposures. The malignant and nonmalignant pulmonary diseases associated with exposure to mineral fibers, including asbestos and silica, are well described. While a theoretical risk of asbestos and silica related disease exists, the literature does not document increased rates of such diseases in firefighters. Nonetheless, firefighters are potentially exposed to these minerals and respiratory protection, even during overhaul, is strongly recommended.
22.4.3 Respiratory cancer in firefighters
Asbestos exposure represents a potential carcinogenic risk for firefighters, as do some heavy metals (cadmium, hexavalent chromium) and chemicals (polyaromatic hydrocarbons, benzene, diesel exhaust). Meta-analyses suggest statistically increased risks of some site specific cancers among firefighters including bladder, central nervous system, colorectal, non-Hodgkin lymphoma, prostate and testicular cancer. Notably, studies to date have not shown an increased risk of respiratory cancers among firefighters.
Military personnel work in both combat and noncombat situations. Noncombat situations include humanitarian missions and emergency disaster assistance. Military duties vary depending on post and may involve rigorous training, maintenance work and repair, administrative duties and weapons/equipment testing. Terrorism, chemical warfare and emergency disaster assistance may expose military personnel to the hazards discussed in the section on first responders. This section will focus on respiratory hazards unique to military personnel, including zinc chloride (smoke bomb) inhalational injury, blast injury to the lung (BLI), asthma/vocal cord dysfunction (VCD) and respiratory infections to which military personnel are at risk.
22.5.1 Epidemiology of respiratory disease in military personnel
Military personnel have increased rates of respiratory infections. The observed increase is largely representative of overseas deployments in general, although further increases are observed during combat operations. Higher rates of other select pulmonary diseases have also been reported in military personnel, including asthma, VCD, acute eosinophilic pneumonia and lung cancer. Military personal may also be presumed to be at increased risk of inhalational injury from exposure to smoke bombs (zinc chloride) and BLI.
22.5.2 Respiratory exposures in military personnel
Smoke bombs are used by the military as an obscurant during training and in combat conditions. The primary pulmonary toxin in smoke bombs is a corrosive zinc chloride aerosol. Documented complications from exposure include upper airway obstruction, bronchospasm, consolidation and acute lung injury. Pathological examination reveals pulmonary edema, pneumonitis, diffuse alveolar damage with alveolar obliteration and, in severe cases, pulmonary fibrosis. Treatment is supportive using ventilatory support and judicious use of steroids. Smoke bomb inhalation may also induce methemoglobinemia, resulting in a functional anemia. Prognosis is generally good, with initial spirometric dysfunction tending to resolve gradually over time in most cases.
Blast injuries affect gas-containing organs and include BLI, ruptured tympanic membranes and intestinal blast injury. In BLI, the blast wave acutely elevates intrathoracic pressure, tearing the alveolar septae, resulting in alveolar hemorrhage, pulmonary edema and the formation of alveolovenous fistulae. Air embolism is a wellrecognized complication and one of the primary causes of immediate death in BLI. Clinically, the triad of respiratory distress, hypoxia and progressive ‘butterfly’ or ‘batwing’ pulmonary infiltrates is characteristic of BLI. Treatment is supportive. Mechanical ventilation should be used with caution due to the risk of pneumothroax and air emboli via alveolovenous fistulae. High-frequency ventilation and nitric oxide may reduce ventilation pressures and improve oxygenation. Survivors of the initial pulmonary sequelae tend to have a good prognosis. During recovery, a restrictive pattern may be seen on pulmonary function testing, which usually returns to baseline over time.
Asthma is a significant disease for military personnel because of its impact on the ability of affected individuals to perform duties. For this reason, in many countries the diagnosis is grounds for exclusion from service. There is some evidence of increased rates of asthma among military personnel, which may reflect occupational exposures or, more likely, case finding of previously undiagnosed exercise-induced asthma during detailed medical pre-placement and surveillance exams.
VCD should be included in the differential diagnosis of asthma, as military personnel may be at increased risk for VCD due to stressors associated with training and combat. VCD should be considered in cases of suspected asthma that present atypically or fail to respond to standard therapy. Further evidence for VCD is provided by spirometry, which may show attenuation of the inspiratory flow volume loop. The gold standard for diagnosis is laryngoscopic demonstration of paradoxical vocal cord movements during an acute attack. Treatment options include patient education, speech therapy and psychological counselling/cognitive behavioral therapy.
Military personnel are at risk of both domestically acquired respiratory infections, as well as infections somewhat unique to military deployments and working conditions. Military camps are prone to epidemics of influenza, Mycoplasma species, pneumococcus, meningococci and adenovirus. Group A streptococci (GAS) pneumonia, uncommon in the general population, has also been found to have a higher incidence among military personnel, and personnel serving overseas have higher than expected rates of Q fever. Crowded living conditions and exposure to populations with increased prevalence of infection are likely to be the most important predisposing factors. New research suggests depressed immune function associated with overexertion during training exercises may also be a contributing factor.
A higher than expected incidence of acute eosinophilic pneumonia (AEP) among military personnel deployed to Iraq and surrounding areas has also been observed. Acute eosinophilic pneumonia is a rare disorder, distinguished from chronic eosinophilic pneumonia by a lack of previous asthma, no protracted history of symptoms prior to presentation and rapid progression to respiratory failure. AEP is characterized by diffuse infiltrates on chest radiograph and pulmonary eosinophilia. The causative agent in cases of AEP in military personnel in Iraq has not been identified. Postulated causes include parasitic infections, certain medications and new-onset smoking.
Tobacco use in the military deserves special mention, because smoking rates in military personnel significantly exceed those of the general population. Proposed explanations for the high prevalence of smoking in military personnel (reported as being over 50% in active personnel) include stress, boredom, lower education level, lower economic status, group living conditions, the encouragement of conformity in an environment with high rates of smoking and the availability of cigarettes at discounted cost. The literature does not suggest military personnel to have an overall increased rate of nonmalignant smoking-related disease, but increased rates of smoking-related cancers have been observed.
22.5.3 Respiratory cancer in military personnel
Rates of malignant respiratory tumors in VA hospitals are double that of the general population, with the majority of these cancers being linked to smoking. It is hypothetically possible that some of these cancers might be related to other exposures including nuclear weapons testing, chemical weapons, propellants used for missiles or substances aerosolized from combustion sources such as oil-well fires, vehicular exhaust and tent heaters. Studies on the subject have considered military personnel in general, as well as specific cohorts such as those involved in nuclear weapons tests and nurses who served in Vietnam, but have not drawn any conclusive links to occupational exposure when smoking is controlled for in the analyses. The exception is mesothelioma. Increased rates of mesothelioma have been demonstrated in war veterans and navy personnel due to asbestos exposure from ship-building and insulation and the use of fire-retardant materials. Increased incidences of mesothelioma have also been documented in military personnel secondary to the assembly and/or use of gas masks in the 1940s, which contained 20% crocidolite in their filters (Table 22.5).
Table 22.5 Respiratory diseases associated with military personnel
| Disease | Associated exposures |
| Infections | Influenza Group A strep Tuberculosis Pneumococcus Meningococci Adenovirus Q fever |
| Acute eosinophilic pneumonia | Elevated rates new onset tobacco smoking Query dust exposure |
| Acute lung insults with potential chronic obstructive and/or restrictive impairment | Zinc chloride (smoke bomb) inhalation Blast lung injury (tends to resolve) |
| Lung cancer | Elevated rates of tobacco smoking |
| Mesothelioma | Asbestos exposure from ship-building, insulation and use of fire retardant materials |
Most US States and Canadian Provinces have presumptive disability provisions that apply to fire fighters and police officers. These laws tend to cover the development of heart and lung disease. Depending on the country, province or state in question, presumption laws may include lung diseases such as COPD, infectious diseases such as tuberculosis and respiratory cancers. In the case of firefighters, lung cancer is rarely included, although amendments in some locales have recently made this addition. Volunteer police and firefighters may also be covered by such legislation depending on the locality in which they work. The International Association of Fire Fighters maintains a database of the current presumptive disability provisions for fire fighters in the USA and Canada (Table 22.6).
Table 22.6 Websites/organizations and suggested reading
| Websites and organizations | |
| Websites/organizations |
|
| Further reading |
|
Compensation for military personnel usually functions within a separate system outside that of civilian workers’ compensation. In the USA, for example, military and Veterans Administration (VA) programs administer such services. In general, compensation provided via the military/VA payment schemes tends to be as good or better with respect to payments and provision of services when compared with civilian workers’ compensation programs.
Further reading
First responders
Banauch, G.I., Dhala, A., Prezant, D.J. (2005) Pulmonary disease in rescue workers at the World Trade Center site. Curr. Opin. Pulmon. Med. 11 (2): 160.
Greenfield, R.A., Brown, B.R., Hutchins, J.B., Iandolo, J.J., Jackson, R., Slater, L.N., Bronze, M.S. (2002) Microbiological, biological, and chemical weapons of warfare and terrorism. Am. J. Med. Sci. 323 (6): 326.
Kales, S.N., Christiani, D.C. (2004) Acute chemical emergencies. New Engl. J. Med. 350 (8): 800.
Urbanetti, J. (1997) Toxic inhalation injury. In Medical Aspects of Chemical and Biological Warfare, Zajtchuk, R., Bellamy, R.F. (eds). Office of the Surgeon General, US Department of the Army: Washington, DC; 1997; 247-270.
Police
Burgess, J.L., Kovalchick, D.F., Siegel, E.M., Hysong, T.A., McCurdy, S.A. (2002) Medical surveillance of clandestine drug laboratory investigators. J. Occup. Environ. Med. 44(2): 184.
Trottier, A., Brown, J. (1995) Occupational medicine for policing. J. Clin. Forens. Med. 2(2): 105-110.
Trottier, A., Brown, J., Wells, G. (1994) Respiratory symptoms among forensic identification workers. J. Clin. Forens. Med. 1(3): 129-132.
Firefighters
Alarie, Y. (2002) Toxicity of fire smoke. Crit. Rev. Toxicol. 32(4): 259.
Prezant, D.J., Dhala, A., Goldstein, A., Janus, D., Ortiz, F., Aldrich, T.K., Kelly, K.J. (1999) The incidence, prevalence, and severity of sarcoidosis in New York City firefighters. Chest 116(5): 1183-1193.
Scannell, C.H., Balmes, J.R. (1995) Pulmonary effects of firefighting. Occup. Med. 10(4): 789-801.
Military
Allen, M.B., Crisp, A., Snook, N., Page, R.L. (1992) ‘Smoke-bomb’ pneumonitis. Respir. Med. 86(2): 165-166.
Avidan, V., Hersch, M., Armon, Y., Spira, R., Aharoni, D., Reissman, P., Schecter, W.P. (2005) Blast lung injury: clinical manifestations, treatment, and outcome. Am. J. Surg. 190(6): 927-931.
Gray, G.C., Callahan, J.D., Hawksworth, A.W., Fisher, C.A., Gaydos, J.C. (1999) Respiratory diseases among U.S. military personnel: countering emerging threats. Emerging Infect. Dis. 5(3): 379.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


