Patients with heart disease and depression have an increased mortality rate. Both behavioral and biologic factors have been proposed as potential etiologic mechanisms. Given that the pathophysiology of depression is considered to involve disruption in brain serotonergic signaling, we investigated platelet response to serotonin stimulation in patients with stable coronary artery disease (CAD). We enrolled 92 patients with stable CAD. Platelet response to increasing concentrations of serotonin (5-HT), epinephrine-augmented 5-HT, and adenosine diphosphate (ADP) was measured by optical aggregation and flow cytometry. As concentrations of 5-HT and ADP increased, so did the activation and aggregation of the platelets. However, on addition of the highest concentration of 5-HT (30 μM), a significant decrease in platelet activation (p = 0.005) was detected by flow cytometry. This contrasts the increase in platelet activation seen with the addition of the highest concentration of ADP. In conclusion, we found increased platelet activation and aggregation with increased concentrations of ADP; however, when platelets are stimulated with a high concentration of 5-HT (30 μM), there is decreased platelet activation. The data demonstrate unique patterns of platelet activation by 5-HT in patients with stable CAD. The cause of this phenomenon is unclear. Our study sheds light on the in vitro response of platelet function to serotonin in patients with stable CAD, which may further the mechanistic understanding of heart disease and depression.
Platelet reactivity is a key component of the pathophysiology of coronary atherosclerosis. Potent vasoconstrictors such as adenosine diphosphate (ADP), epinephrine, and thromboxane have been well studied in patients with stable coronary artery disease (CAD). Mental stress has been shown to induce platelet activation in patients with CAD. Serotonin (5-HT) has recently gained increasing interest as greater evidence collects on depression as an independent risk factor for cardiovascular disease. 5-HT has been considered to be the link between the 2 diseases of CAD and depression. 5-HT has been shown to also mediate an exaggerated platelet response in patients with acute coronary syndrome (ACS). There has been a recent cross-sectional study showing increased platelet reactivity to serotonin in depressed patients 3 months after an ACS. However, to our knowledge, no study has examined 5-HT–mediated platelet activity in truly stable CAD without an event within 1 year. To further delineate the role of serotonin in heart disease, we conducted a study to observe the physiological response of platelets to direct serotonin challenge and augmented serotonin challenge in patients with stable CAD.
Methods
We enrolled 92 patients with stable CAD from a single urban academic medical center from February 2011 to July 2013. Patients were designated as patients with stable CAD if they had CAD diagnosed by cardiac catheterization (≥50% coronary stenosis), electrocardiographic criteria of myocardial infarction, or stress testing revealing ischemia or infarction. Patients were recruited from outpatient cardiology clinics when they presented for scheduled follow-up and who by report had been taking daily aspirin therapy for at least 6 months. Exclusion criteria included an ACS within the past year before enrollment, current or previous (14 days) use of glycoprotein IIb/IIIa inhibitor, active narcotic use by personal report or laboratory testing, inability to give informed consent, baseline platelet count <100 K/μl, current use of antidepressants, and chronic disease with a <1-year expected mortality.
The study was approved by the Johns Hopkins Institutional Review Board, and all patients provided written informed consent. All patients had platelet functional testing.
Study participants had blood drawn and immediately centrifuged to obtain platelet rich plasma (PRP). Once PRP was obtained, the remainder of the blood was centrifuged to form platelet poor plasma as a control. Flow cytometry was performed to measure platelet activation brought on by varying concentrations of serotonin and ADP. The PRP was diluted to the same concentrations for each patient sample (250 ± 20 × 10 3 platelets/μl) and incubated with various concentrations of serotonin hydrochloride (0.3, 3, 5, 15, and 30 μM) and ADP (0.5, 5, 10, and 20 μM). Epinephrine (1 mM) was not used to boost platelet activation levels in this analysis because of the sensitivity of flow cytometry on detecting even minimal expressions of platelet activation. Arg-Gly-Asp-Ser (RGDS) (Sigma-Aldrich, St. Louis, Missouri) was used as a negative control. For flow cytometry, PAC-1-FITC (Sigma-Aldrich, St. Louis, Missouri) was used to determine the conformational change of activated platelets, while anti-CD61-PerCP (Sigma-Aldrich, St. Louis, Missouri) was used to label platelets for analysis. These samples were incubated at room temperature and quenched with 1% paraformaldehyde (Polysciences, Warrington, Pennsylvania). These samples were analyzed using a FACSCalibur flow cytometer (Becton, Dickinson and Company, Franklin Lakes, New Jersey). The results were represented as histograms and dot plots using Cell Quest 3.1 software (Becton, Dickinson and Company).
Platelet aggregation was assessed using standard light transmission in PRP. Serotonin hydrochloride and ADP were added to PRP to obtain 0.3, 3, 5, 15, and 30 μM serotonin and 0.5, 5, 10, and 20 μM ADP concentrations, respectively. The range of concentrations used is the same as a recent study conducted showing association of depression score and platelet aggregation in patients with ACS. Unlike ADP, 5-HT, in vitro, is a very weak platelet agonist that causes reversible platelet aggregation and is considered a “helper agonist,” hence it is generally used in conjunction with a second agonist when measuring platelet aggregation. A fixed dose of epinephrine was chosen because it induces an increase in the maximal response to 5-HT without changing the half maximal effective concentration EC 50 value of 5-HT or the affinity of 5-HT to the platelet 5-HT 2A receptor. Arachidonic acid (1 mM) was used to assess aspirin response.
Distributions of demographic and clinical characteristics of the study sample are described as mean and SD for continuous variables and as frequency (%) for categorical variables. The association of epinephrine-augmented serotonin platelet aggregation or serotonin-stimulated platelet activation as measured by flow cytometry, as well as ADP-induced platelet aggregation and activation as dependent variables with agonist dose, adjusted for gender or race was assessed using mixed model regression, with random effect for within-individual repeat measurements. To assess whether there may be confounding by gender or race on either epinephrine-augmented serotonin platelet aggregation or serotonin-stimulated platelet activation as measured by flow cytometry, as well as ADP-induced platelet aggregation and activation, we initially controlled for both gender and race and found no differences in either serotonin- or ADP-induced platelet aggregation and activation; therefore, we report data unadjusted for gender or race.
Results
Demographic and clinical characteristics of the 92 patients with stable CAD are presented in Table 1 . The mean age of the participants was 66 years. Men constituted 67% of the population. The mean body mass index was 32 kg/m 2 . The predominant race was white (87%) with 12% African-Americans. Two-thirds had myocardial infarction in the past with 29% requiring previous coronary artery bypass surgery and 95% having a previous percutaneous intervention. Fifteen percent had a history of depression. Half of the population had a family history of early CAD and most had hypertension and dyslipidemia. Thirteen percent of the enrolled population were current smokers. Thirty-eight percent were diabetic. As a prerequisite, all participants were receiving aspirin therapy. One-third of the participants were receiving clopidogrel therapy in addition to their aspirin therapy.
| Variable | Total (n = 92) |
|---|---|
| Age (years) | 66 ± 9 |
| Men | 62 (67%) |
| Body mass index (kg/m 2 ) | 32 (19–61) |
| European American | 80 (87%) |
| African American | 11 (12%) |
| Asian | 1 (1%) |
| Prior myocardial infarction | 61 (66%) |
| Prior coronary artery disease | 92 (100%) |
| Prior coronary artery bypass | 27 (29%) |
| Prior percutaneous intervention | 87 (95%) |
| Diabetes mellitus | 35 (38%) |
| Hypertension ∗ | 78 (85%) |
| Dyslipidemia ∗ | 82 (89%) |
| History of depression | 14 (15%) |
| Current smoker | 12 (13%) |
| Family history † | 47 (51%) |
| Antiplatelet medications | |
| Aspirin | 92 (100%) |
| Clopidogrel | 27 (29%) |
∗ Documented medical history of hypertension and dyslipidemia.
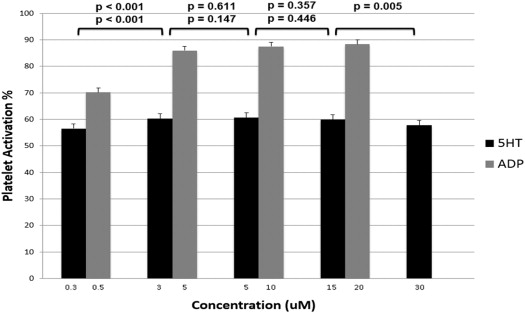
When platelets were activated with nonaugmented direct serotonin, there was an initial increase from serotonin concentration 0.3 to 3 μM (56.5% ± 1.9 vs 60.2% ± 1.9, mean percent activation ± standard error, p <0.001) with a plateau of platelet activation level from concentrations 3 to 15 μM (60.2% ± 1.9 vs 60.6% ± 1.9 vs 59.9% ± 1.9). However, on addition of the highest concentration of 5-HT (30 μM), platelet activation was significantly lower compared with the second to highest concentration of serotonin (15 μM) detected by flow cytometry (57.8% ± 1.8 vs 59.9% ± 1.8, p = 0.005). The peak platelet activation was seen at the 5-HT concentration of 5 μM. This is in contrast to the platelet activation that was seen with ADP. Platelet activation in response to ADP showed an initial increase from the lowest to next concentration, then a subsequent plateau at the higher ADP concentrations from 5 to 20 μM without evidence of lower platelet activation at the maximum concentration of ADP (20 μM) as seen with 5-HT. Platelet activation at the highest concentration of ADP (20 μM) was not significantly different compared with the second to highest concentration of ADP (10 μM; 88.4% ± 1.5 vs 87.7% ± 1.5, p = 0.45; Figure 1 ). A mixed regression model showed no significant difference for gender (p = 0.63 for 5-HT, p = 0.63 for ADP) or race (p = 0.82 for 5-HT, p = 0.49 for ADP). After adjustment for clopidogrel use, we found that direct serotonin-stimulated platelet activation was not decreased in those patients receiving clopidogrel therapy compared with those not receiving clopidogrel (p = 0.43). For ADP-induced platelet activation, there was an overall significant decrease in those patients receiving clopidogrel therapy compared with those not receiving clopidogrel (p <0.001). Although, when directly comparing the clopidogrel groups at each of the ADP levels, only the lowest concentration of 5 μM was statistically significant. The other’s mean activations were lower for those patients on clopidogrel therapy compared with those not on clopidogrel, but were not statistically significant ( Table 2 ).
| Agonist Concentration (μM) | Clopidogrel (+) | Clopidogrel (−) | p-Value |
|---|---|---|---|
| 5HT aggregation | |||
| 0.3 | 31.5 | 32.6 | 0.79 |
| 3.0 | 51.1 | 53.1 | 0.39 |
| 5.0 | 51.3 | 55.4 | 0.08 |
| 15 | 53.0 | 57.6 | 0.05 |
| 30 | 52.5 | 56.4 | 0.10 |
| 5HT activation | |||
| 0.3 | 53.0 | 59.2 | 0.13 |
| 3.0 | 62.4 | 63.0 | 0.72 |
| 5.0 | 62.3 | 63.6 | 0.44 |
| 15 | 61.5 | 63.0 | 0.39 |
| 30 | 60.7 | 60.3 | 0.81 |
| ADP aggregation | |||
| 0.5 | 5.0 | 13.5 | <0.01 |
| 5.0 | 41.9 | 66.2 | <0.01 |
| 10 | 46.1 | 70.3 | <0.01 |
| 20 | 52.6 | 74.1 | <0.01 |
| ADP activation | |||
| 0.5 | 59.4 | 74.3 | <0.01 |
| 5.0 | 75.9 | 90.5 | 0.81 |
| 10 | 78.7 | 91.4 | 0.28 |
| 20 | 80.7 | 91.7 | 0.06 |
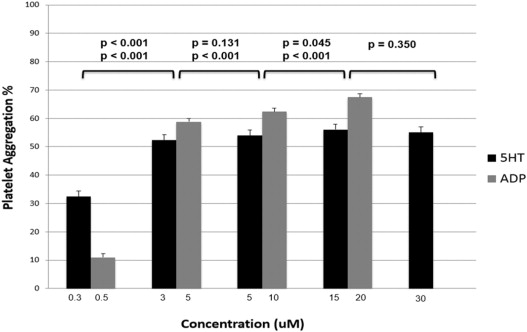
Platelet aggregation when stimulated with epinephrine-augmented 5-HT increased from lowest concentration of 0.3 μM to the next concentration of 3 μM (32.5% ± 1.9 vs 52.3% ± 1.9, p <0.001) and again from 5-HT concentrations of 5 μM to 15 μM (53.9% ± 1.9 vs 56.1% ± 1.9, p = 0.045). No difference in aggregation level was seen from concentrations 3 μM to 5 μM (52.3% ± 1.9 vs 53.9% ± 1.9, p = 0.131) and from 15 μM to 30 μM (56% ± 1.9 vs 55% ± 1.9, p = 0.35). Of note, the mean aggregation level was lower at the highest 5-HT concentration of 30 μM compared with the peak level at the 5-HT concentration of 15 μM. When platelets were stimulated with ADP there was a continued increase in aggregation level with each increasing concentration of ADP (11.0% ± 1.2 vs 58.8% ± 1.2 vs 62.4% ± 1.2 vs 67.5% ± 1.2, p <0.001 between each concentration; Figure 2 ). A mixed regression model showed no significant difference for gender (p = 0.13 for 5-HT, p = 0.90 for ADP) or race (p = 0.04 for 5-HT, p = 0.49 for ADP). After adjustment for clopidogrel use, we found that epinephrine-augmented serotonin platelet aggregation was not decreased in those patients receiving clopidogrel therapy compared with those patients not receiving clopidogrel at any of the 5-HT concentrations (p = 0.26 in linear regression model). However, for ADP-induced platelet aggregation, there was a significant decrease in those patients receiving clopidogrel therapy compared with those not receiving clopidogrel (p <0.001; Table 2 ).