Plantar and Tarsal Artery Reconstructions
Enrico Ascher
Anil Hingorani
Natalie Marks
Frank J. Veith
In excess of five decades have passed since Jean Kunlin’s breakthrough publication depicted his clinical experience with a novel type of arterial reconstruction to avoid major amputations in patients with severe occlusive disease of the superficial femoral artery. Other investigators have confirmed the efficacy and durability of femoropopliteal bypasses using reversed saphenous vein making this become the procedure of choice over lumbar sympathectomy and endarterectomy.
Thereafter, it was discovered that other surgeons extended the bypass of occluded arterial segments in the lower extremity to the major branches of the popliteal artery. However, despite the fact that the bulk of patients with lower extremity atherosclerotic occlusive disease involving or threatening tissue loss have a disease pattern amenable to arterial reconstruction above or below the knee, a lesser but noteworthy number will need bypass to inframalleolar vessels.
These bypasses to branches of tibial arteries in the foot have shown to be an acceptable alternative and are preferable to major amputation. This is especially seen in the elderly diabetic population with limited rehabilitation potential in which this clinical presentation occurs most frequently. The following discussion will focus on the management of these patients, including a review of the anatomic relations important for vessel exposure, and the reported results.
The indications for surgery remain tissue loss or rest pain.
Preoperative Planning
Preoperative evaluation with noninvasive segmental blood pressure measurements and pulse-volume recordings are helpful to not only document and confirm clinical impressions, but as a comparison for postoperative surveillance. Angiography is necessary to demonstrate both inflow and outflow sites for the bypass. Typically, the most distally available inflow site is preferentially used to shorten the length of the vein graft.
Identification of a distal outflow vessel usually necessitates biplanar views to differentiate a “blind” dorsalis-pedis artery from a lateral tarsal or the medial from the
plantar arteries. Time-delayed imaging may be used to visualize the foot arteries because of the reduced flow. Lately, the use of magnetic resonance angiography has proved to be of benefit in identifying patent lower extremity arteries not demonstrated by conventional arteriographic techniques. Moreover, some centers have examined the use of duplex arteriography for the preoperative planning for these types of procedures.
plantar arteries. Time-delayed imaging may be used to visualize the foot arteries because of the reduced flow. Lately, the use of magnetic resonance angiography has proved to be of benefit in identifying patent lower extremity arteries not demonstrated by conventional arteriographic techniques. Moreover, some centers have examined the use of duplex arteriography for the preoperative planning for these types of procedures.
Anatomic Exposure and Techniques
Plantar Arteries
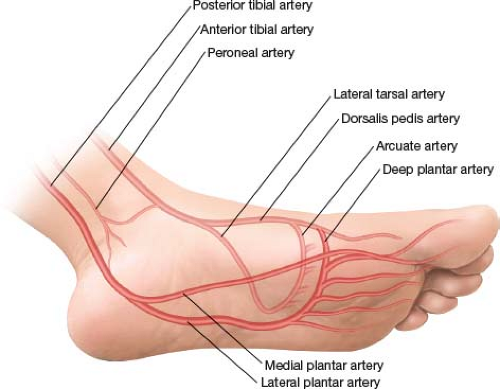
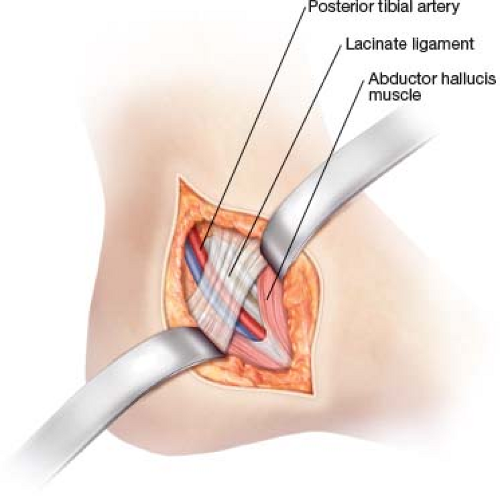
A complete knowledge of the topographic anatomy of the foot is requisite to facilitate the exposure of these vessels. The posterior tibial artery bifurcates a short distance inferior to the medial malleolus into two major branches: The lateral and medial plantar arteries (Fig. 27.1). Exposure of the medial or lateral plantar arteries is facilitated by initially dissecting the retromalleolar posterior tibial artery lying deep to the lacinate ligament (flexor retinaculum) (Fig. 27.2). Extension of the incision into the sole of the foot will eventually expose the two main branches of the posterior tibial artery (Fig. 27.3). Although anatomic variation is not rare, the lateral plantar artery most often forms the main plantar arch and is larger than its medial counterpart. The smaller medial plantar artery supplies via small collateral vessels, the intrinsic muscles of the first, second, and third toes (Fig. 27.1). If the lateral plantar branch is occluded, then the medial plantar artery may enlarge and supply the arch via collaterals.
A direct approach to these vessels for several reasons is not suggested. Firstly, due to the thick nature of the skin on the sole of the foot, it is not easily retractable and satisfactory exposure is difficult unless the incision exactly follows the course of the vessel. Secondly, the small diameter of these vessels, coupled with their relatively deep location within the foot, makes their localization difficult when approached directly. Finally, because the lateral plantar artery is usually larger and inferiorly located when the foot is externally rotated, its exposure and isolation is facilitated by observing the branch point from the posterior tibial artery. As soon as either of the vessels is identified and isolated, further exposure can be accomplished by incising the lacinate ligament along with transection of the abductor hallucis muscle. More distal exposure can be obtained by division of the medial border of the plantar aponeurosis and the flexor digitorum brevis muscle.
Deep Plantar Artery
The deep plantar arch branch of the dorsalis pedis artery is located by extending the initial incision used to identify the dorsalis pedis artery distally to the metatarsal bone level. The deep plantar branch originates at this point. It courses through a foramen bounded proximally by the dorsal metatarsal ligament, distally by the dorsal interosseous muscle ring, and medially and laterally by the base of the first and second metatarsal bones (Fig. 27.4). Deep to the foramen, the plantar arch joins with the lateral plantar artery to form the deep pedal arch. Exposure of the artery within the foramen is enhanced by retracting or transecting the extensor hallucis brevis muscle along with elevating the periosteum of the proximal




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree