Chapter 5 Physiotherapy techniques
ACUPUNCTURE
What can be treated with acupuncture?
Acupuncture is recognized by the World Health Organization (WHO) in the treatment of respiratory conditions (Hopwood 1993) and acupuncture techniques can also be used to treat associated symptoms: acute and chronic pain, panic attacks and stress, which are so often a contributing or causative factor. Acupuncture has been found to be safe and potentially effective for bronchial asthma and chronic obstructive pulmonary disease (COPD) (Jobst 1995). It has been reported to help con-trol disabling breathlessness (Linde et al 1986), asthma (Blackwell 2004) and improve lung function and quality of life in COPD (Neumeister et al 1999). Acupuncture used pre- and postoperatively may reduce postoperative pain, the risk of infection and improve recovery rate.
The techniques used and the evidence base
Needling is the biggest cause of adverse effects in acupuncture (Halvorsen et al 1995, Rampes & James 1995). Many respiratory patients have contraindications to needling and to the use of certain body acupuncture points (acupoints). Therefore a combination of non-invasive body and ear acupuncture (auriculotherapy) is used to overcome these limitations. Each can be used on its own, but they are more effective if used together or with another treatment modality. Acupuncture treatment is based on evidence from different levels of research, from systematic reviews (Ezzo 2000) to clinical opinion.
Non-invasive options include acupressure, laser, magnetic and electrical stimulation (Baxter 1994, Kenyon 1983, 1988, Lawrence et al 1998) and have been found to be as effective as needling in the body (Vickers 1986). In auriculotherapy, electrical stimulation was more effective than needling for pain relief (Oleson 1998). Acupressure, where no equipment is required, is an invaluable tool for both therapist and patient, and it can be used as a home treatment to enhance and maintain the effect of treatment. Acupressure was found to reduce dyspnoea and be a useful adjunct for patients undergoing a pulmonary rehabilitation programme (Maa et al 1997). Laser acupuncture was of benefit in the treatment of sinusitis, asthma and pnuemonia (Ridge 2005). Unpublished case studies have also shown that non-invasive methods can be as effective as needling and in some cases, more effective.
How do acupuncture techniques work?
Stimulation of an acupoint activates A-delta, A-beta and C afferents, which inhibit the sensory and affective components of pain via gating and descending inhibitory pathways (Lund et al 2006). Endorphins and serotonin are released which, as well as having an analgesic effect, have been shown to effect cell growth and healing. (Kishi et al 1996, Pakala & Benedict 1998). Stimulation of certain acupoints activates cortical areas of the brain that have controlling effects on symptoms being treated (Zhang 1986). The traditional concept is one of energy flowing within meridians. The energy becomes imbalanced by disease and acupoints are chosen to create a re-balance. Active points that require treatment are detectable by electrical skin resistance measurement and by palpation for tenderness. Acupoints and meridians have a high concentration of gap junctions (Mashanskii et al 1983), facilitating intercellular communication and thereby mediating the effects of acupuncture.
Auriculotherapy (ear acupuncture)
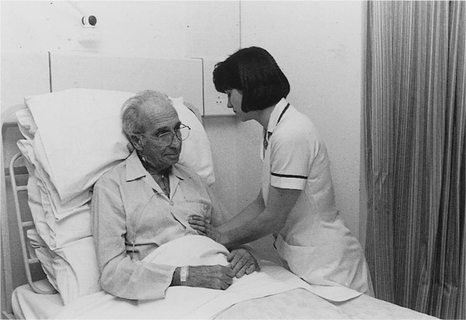
Auriculotherapy (Fig. 5.1) is safer than body acupuncture, quicker and access is easier. It is therefore useful in situations such as critical care. Patients contraindicated to body acupuncture, for example those with heart conditions, can be safely treated via the ear. Certain drugs will reduce the effectiveness of body acupuncture, for example corticosteroids acting as a partial opiate antagonist, but these same drugs do not reduce the effectiveness of auriculotherapy. Every anatomical structure and physiological function of the body is represented by an acupoint on the ear (Nogier 1981, Oleson 1998, Practical Ear Needling Therapy 1980). These points become active when disease is present and are detected by palpation for tenderness, ideal when treating pain; and electrical resistance measurement, ideal for non-painful conditions. Stimulation of these points has an effect on the corresponding body area or function. An electromagnetic balancing is achieved, internal opiates are released and there can be an immediate reflex effect on, for example, pain. Tiny gold-plated magnets can be placed over selected points between treatments, creating constant pressure and a magnetic field to prolong the effectiveness of treatment. The patient can apply additional pressure to obtain further relief of symptoms, thus reducing the frequency and number of visits required. Auriculotherapy is one of the safest and most effective ways of dealing with conditions more complicated than pain. In addition to treatment, it can also be used for prevention and diagnosis (Lichstein et al 1974).
Some useful body points
| CV 17 | On the sternum roughly midway between the nipples. Useful for shortness of breath and in conjunction with breathing exercises, works well by applying straight pressure to the point on exhalation. |
| PC 6 | In the centre of the anterior aspect of the forearm, three fingers’ breadth from the anterior wrist crease. Effective for hyperventilation, stress reduction and relief of nausea and vomiting (Stainton & Neff 1994). |
| LI 4 | Adduct the thumb, find the high point of the interosseus muscle and press towards the second metacarpal. One of the most useful points in the body. Useful for pain relief and stress reduction. |
AIRWAY CLEARANCE TECHNIQUES
Airway clearance techniques are used to facilitate mucociliary clearance. Under normal circumstances the mucociliary clearance mechanism is extremely effective and efficient but in the presence of many respiratory diseases and following anaesthesia and surgical procedures, airway clearance techniques may be required to enhance mucociliary clearance. There is as yet no evidence to support the use of any one airway clearance technique over any other (Accurso et al 2004, Prasad & Main 1998, Pryor 2005, Pryor et al 2006). Practice tends to be influenced by culture and patient preference. The airway clearance techniques available to patients may be determined by the skills of the therapist (Hardy et al 1994) and the financing of healthcare provision. When a device, for example positive expiratory pressure (PEP) or oscillating PEP (Acapella®, Flutter® or RC-Cornet®), is included in an airway clearance regimen, meticulous cleaning and thorough drying of the equipment after use is essential to prevent the possibility of infection from the device. Other techniques, for example intermittent positive pressure breathing and glossopharyngeal breathing, may also assist in the clearance of secretions and have additional effects.
If an airway clearance technique is required in the long term, it is important to negotiate rather than prescribe a physiotherapy home programme to increase adherence to treatment (Carr et al 1996). Programmes must be realistic and appropriate general physical activities should be encouraged. Revision of techniques at intervals is important to assess the effectiveness of the regimen and to correct and update techniques as necessary. Currie et al (1986) recognized the importance of reassessment in maintaining adherence to treatment.
Traditionally airway clearance techniques have been associated with head-down tipped positioning, but this is now used only if individual patient benefit is identified on assessment. Several systematic reviews have been undertaken looking at airway clearance in people with cystic fibrosis (Elkins et al 2006a, Main et al 2005, van der Schans et al 2000). Chest physiotherapy (postural drainage and percussion) was compared with no chest physiotherapy (van der Schans et al 2000). It was concluded that airway clearance techniques may have short-term effects in the context of increasing mucus transport, but no evidence was found on which to draw conclusions concerning the long-term effects. Elkins et al (2006a) studied PEP and Main et al (2005) compared ‘conventional’ chest physiotherapy (postural drainage and percussion) with other contemporary airway clearance techniques (active cycle of breathing techniques, autogenic drainage, PEP, oscillating PEP and high-frequency chest wall oscillation). There appeared to be no advantage of ‘conventional’ chest physiotherapy over the other airway clearance techniques, in the primary outcome measure of lung function. In the review by Elkins et al (2006a), there was an indication that individuals prefer regimens that can be self-administered.
Holland & Button (2006) reviewed the place of airway clearance techniques in chronic respiratory disease and proposed a physiological rationale for the use of airway clearance techniques in chronic obstructive pulmonary disease taking into consideration the presence of bronchiectasis, amount of sputum expectorated, degree of airflow obstruction and presence of decreased lung elastic recoil.
Active cycle of breathing techniques
The active cycle of breathing techniques (ACBT) has been shown to be effective in the clearance of bronchial secretions (Pryor et al 1979, Wilson et al 1995) and to improve lung function (Webber et al 1986) without increasing hypoxaemia (Pryor et al 1990) or airflow obstruction (Pryor & Webber 1979, Pryor et al 1994, Thompson & Thompson 1968).
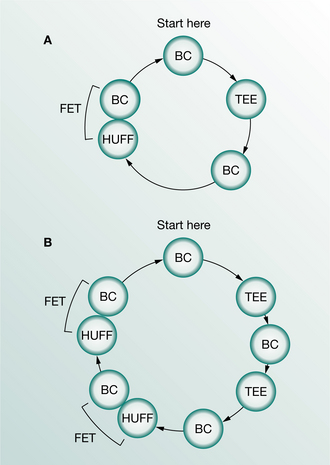
The ACBT is a flexible regimen that can be adapted for any patient in whom there is a problem of excess bronchial secretions and can be used with or without an assistant. It is a cycle of breathing control, thoracic expansion exercises and the forced expiration technique (FET) (Fig. 5.2). The original studies of ‘the forced expiration technique’ (Hofmeyr et al 1986, Pryor et al 1979, Webber et al 1986) used this cycle of techniques, but people began to use a regimen of huffing alone or other variations on the FET (Falk et al 1984, Reisman et al 1988) and the literature became confusing. In order to emphasize the use of thoracic expansion exercises and the periods of breathing control, in addition to the FET, the whole regimen was renamed the active cycle of breathing techniques (ACBT) (Webber 1990). The regimen did not change in practice and the early studies on the FET were controlled clinical trials on the ACBT.
Thoracic expansion exercises
Thoracic expansion exercises are deep breathing exercises emphasizing inspiration. Inspiration is active and is usually combined with a 3-second end- inspiratory hold before passive relaxed expiration. The postoperative manoeuvre of a 3-second hold at full inspiration has been shown to decrease collapse of lung tissue (Ward et al 1966). This ‘hold’ may also be of value in patients with medical chest conditions to allow for asynchronous ventilation as air flows more quickly into healthy, unobstructed areas than into diseased and obstructed regions. Pendelluft flow is that which takes place between parallel respiratory units with different time constants (Mead et al 1970).
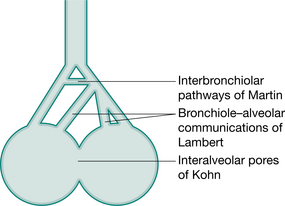
In the normal lung, the resistance to airflow via the collateral ventilatory system is high and there is little movement of gas through these channels. With increasing lung volume and in the presence of lung pathology, resistance decreases allowing air to flow via the collateral channels – the interalveolar pores of Kohn, bronchiole–alveolar communications of Lambert and interbronchiolar pathways of Martin (Menkes & Traystman 1977) (Fig. 5.3) and to come in behind secretions. These collateral channels are not present in infants and young children and it is unknown when, in the developmental process, they become patent.
The effectiveness of thoracic expansion exercises, in re-expanding lung tissue and in mobilizing and clearing excess bronchial secretions, can also be explained by the phenomenon of interdependence (Mead et al 1970). This is the effect of expanding forces exerted between adjacent alveoli. At high lung volumes the expanding forces between alveoli are greater than at tidal volume and may assist in re-expansion of lung tissue (Fig. 5.4). About three expansion exercises are usually appropriate before pausing for a few seconds for a period of breathing control. Too many deep breaths may produce the effects of hyperventilation, are tiring and reduce the number of huffs undertaken within the time period. The thoracic expansion exercises may be undertaken consecutively or patients may like to take a normal-sized breath in between.
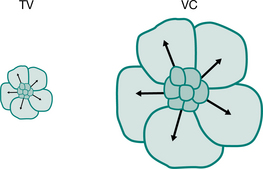
Figure 5.4 Interdependence. The effect of expanding alveoli at tidal volume (TV) and vital capacity (VC).
Thoracic expansion exercises can be facilitated with proprioceptive stimulation by placing a hand, either the patient’s or the physiotherapist’s, over the part of the chest wall where movement of the chest is to be encouraged (Fig. 5.5). There may be an initial increase in ven- tilation to this part of the lung (Tucker et al 1999) and there should be an increase in chest wall movement.
Forced expiration technique (FET)
With any forced expiratory manoeuvre there is dynamic compression and collapse of the airways downstream (towards the mouth) of the equal pressure point (West 2004). This is an important part of the clearance mechanism of either a huff or cough. At lung volumes above functional residual capacity, the equal pressure points are located in lobar or segmental bronchi (Macklem 1974). As lung volume decreases, during a forced expiratory manoeuvre, the equal pressure points move distally into the smaller more peripheral airways. Figure 5.6 is a static representation of the dynamic state of a forced expiratory manoeuvre (huff or cough). The pleural pressure at this instance is +20 cmH2O, the elastic recoil pressure of the lungs is +5 cmH2O and consequently the peripheral pressure is +25 cmH2O. There is a downward gradient from +25 cmH2O at the alveolus to zero at the mouth and, somewhere along the airway, the pressure within the airway will equal the pleural pressure. Proximal to this, dynamic collapse and compression of the airway takes place. The dynamic collapse and compression during a forced expiratory manoeuvre is effective from points, choke points (Dawson & Elliott 1977), downstream of the equal pressure point.
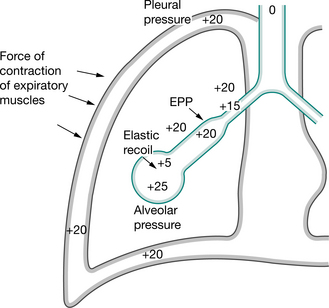
Figure 5.6 Forced expiratory manoeuvre: huff or cough.
(Pryor 1991. In Pryor JA (ed) Respiratory care, p 84. Reproduced with permission of Elsevier, Edinburgh)
A series of coughs without intervening inspirations was advocated by Mead et al (1967) to clear bronchial secretions, but clinically a single continuous huff down to the same lung volume is as effective and less exhausting. Hasani et al (1994) compared cough with the FET and concluded that both were equally effective in clearing lung secretions, but that the FET required less effort.
The mean transpulmonary pressure during voluntary coughing is greater than during a forced expiration. This results in greater compression and narrowing of the airways, which limits airflow and reduces the efficiency of bronchial clearance (Langlands 1967). In 1989 Freitag et al demonstrated an oscillatory movement, ‘hidden’ vibrations, of the airway walls in addition to the squeezing action produced by the forced expiratory manoeuvre.
The viscosity of mucus is shear-dependent (Lopez-Vidriero & Reid 1978) and the shear forces generated during a huff should reduce mucus viscosity (Selsby & Jones 1990). This, together with the high flow of a forced expiratory manoeuvre, would also be expected to aid mucus clearance and the expectoration of sputum.
When mobilizing and clearing peripheral secretions, it is an unnecessary expenditure of energy to start the huff from a high lung volume. A huff from mid-lung volume is more efficient and probably more effective. To huff from mid-lung volume a medium-sized breath should be taken in and, with the mouth and glottis open, the air is squeezed out using the chest wall and abdominal muscles. It should be long enough to loosen secretions from the more peripherally situated airways and should not be just a clearing noise in the back of the throat. However, if the huff is continued for too long it may lead to unnecessary paroxysmal coughing. Too short a huff may be ineffective (Partridge et al 1989) but when secretions have reached the upper airways, a shorter huff or a cough from a high lung volume is used to clear them.
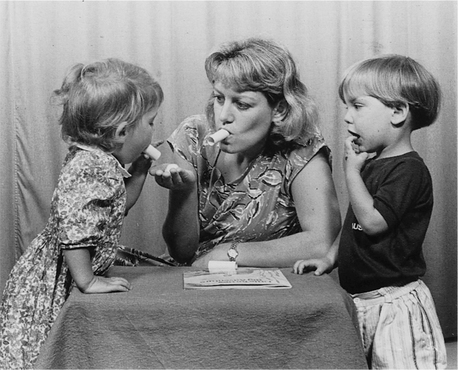
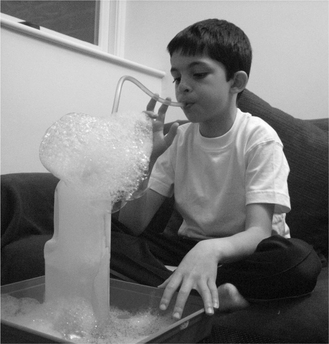
The huff is a forced but not violent manoeuvre. To be maximally effective, the length of the huff and force of contraction of the expiratory muscles should be altered to maximize airflow and to minimize airway collapse. A peak flow mouthpiece, or similar piece of tubing, may improve the effectiveness of the huff as it should help to keep the glottis open. Some people find huffing through a tube, at a tissue or a cotton wool ball, helpful in perfecting the technique. The huff can be introduced to children as blowing games (Thompson 1978) and from about the age of 2 years they are usually able to copy others huffing (Fig. 5.7).
An essential part of the forced expiration technique is the pause for breathing control after one or two huffs, to prevent any increase in airflow obstruction. The length of the pause will vary from patient to patient. In a patient with bronchospasm or unstable airways or in one who is debilitated and fatigues easily, longer pauses (perhaps 10–20 seconds) may be appropriate. In patients with no bronchospasm the periods of breathing control may be considerably shorter (perhaps two or three breaths or 5–10 seconds).
In the tetraplegic patient, clearance of secretions from the upper airways is difficult because maximum lung volume cannot be achieved and the equal pressure points will therefore never reach the largest airways (Morgan et al 1986). Secretions can be cleared from the smaller airways, but accumulate in the larger upper airways. The use of glossopharyngeal breathing may assist clearance from the upper airways.
The techniques of breathing control, thoracic expansion exercises and the forced expiration technique should be used flexibly and adapted for, and by, each patient during each treatment session. One set of thoracic expansion exercises may be followed by the forced expiration technique (see Fig. 5.2A) but if secretions loosen slowly, it may be more appropriate to use two sets of thoracic expansion exercises (see Fig. 5.2B) interspersed with a period of breathing control. Most surgical patients will benefit from the 3-second hold with the thoracic expansion exercises and there is rarely an indication, in the surgical patient, for the use of chest clapping. Wound support may be more suitable than chest compression during huffing and coughing (Fig. 5.8).
In many patients, medical and surgical, secretions can be cleared effectively using the ACBT in the sitting position, but on occasions gravity-assisted positions may be indicated, for example a lung abscess. Cecins et al (1999) studied the effects of gravity (positions with and without a head-down tilt) in a group of patients with cystic fibrosis, bronchiectasis and immotile cilia syndrome, using the ACBT. There were no significant differences in lung function or in the weight of sputum expectorated during treatment. Most of the patients preferred the horizontal position and felt less breathless without a head-down tilt.
Autogenic drainage
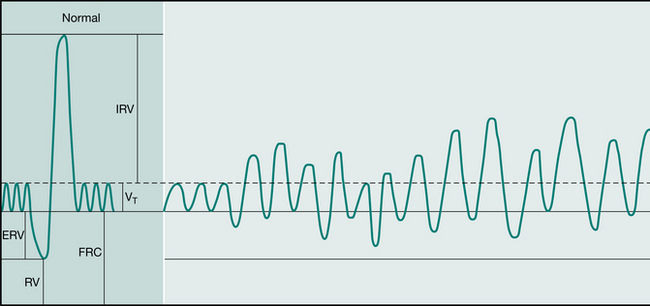
Autogenic drainage (AD) aims to maximize airflow within the airways, to improve ventilation and the clearance of mucus (Chevaillier 2002). Chevaillier developed this concept in Belgium in the late 1960s but little was published until 1979 (Dab & Alexander 1979). Autogenic drainage utilizes gentle breathing at different lung volumes to loosen, mobilize and clear bronchial secretions.
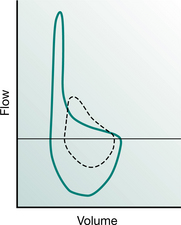
In people with pressure-dependent airway collapse the increase in airflow, with an unforced compared with a forced expiratory manoeuvre, can be demonstrated using the flow–volume loop (Fig. 5.9). Many people with chronic respiratory disease will have a degree of pressure-dependent airway collapse, but in the absence of pressure-dependent collapse it is not possible to move outside the flow–volume loop, i.e. to increase airflow with an unforced expiratory manoeuvre.
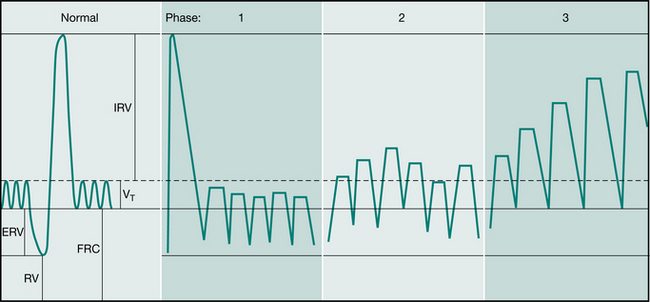
Chevaillier originally described three phrases: ‘unstick’, ‘collect’ and ‘evacuate’ (Schöni 1989) (Fig. 5.10). The breathing technique is that of a slow breath in, keeping the upper airways (mouth and glottis) open. It is recommended that the breath in be held for 2–4 seconds. This ‘hold’ facilitates more equal filling of lung segments, by allowing for the variation in time constants within different lung regions (collateral ventilation). Expiration is performed keeping the upper airways open, as if sighing. The expiratory force is balanced so that the expiratory flow reaches the highest rate possible without causing airway compression. Air flow at a high velocity enhances shear forces. As mucus is mobilized it can be both heard and felt (by placing the hands on the chest) (Fig. 5.11). This cycle is repeated through varying lung volumes.
Breathing at low lung volumes is said to mobilize peripheral mucus. This is the first or ‘unstick’ phase. It is followed by a period of breathing around the individual’s tidal volume which is said to ‘collect’ mucus from the middle airways. Then, by breathing around high lung volumes, the ‘evacuate’ phase, expectoration of secretions from the central airways is promoted. When sufficient mucus has been collected in the large airways it may be cleared by coughing or huffing. Coughing before this point is discouraged (Chevaillier 2001 personal communication, Chevaillier 2002). Autogenic drainage is usually undertaken in the sitting or supine lying positions.
A short-term study compared AD with the ACBT (Miller et al 1995), but this was not the ACBT as outlined above. In a long-term study of patients with cystic fibrosis, AD was compared with postural drainage and per- cussion, with an assistant (Davidson et al 1992). AD was found to be at least as effective as the conventional treatment and the patients expressed a marked preference for AD.
In Germany the practice of AD was modified (David 1991, Kieselmann 1995) and not split into the three phases, as the patients found breathing at low lung volumes uncomfortable. This technique is known as modified autogenic drainage (M AD) (Fig. 5.12). The patient breathes around tidal volume while breath holding for 2–3 seconds at the end of each inspiration. Coughing is used to clear mucus from the larynx (Kieselmann 1995).
Chest clapping
Chest clapping is performed using a cupped hand with a rhythmical flexion and extension action of the wrist. The technique is often performed with two hands but, depending on the area of the chest, it may be more appropriate to use one hand. For the infant, chest clapping is performed using two or three fingers of one hand or using a soft rubber facemask (Chapter 10). Single-handed chest clapping is probably the technique of choice for self-chest clapping as it is difficult to coordinate two-handed clapping at the same time as using thoracic expansion exercises.
Mechanical percussion has been shown to increase intrathoracic pressure (Flower et al 1979) and chest clapping may have a similar effect, but this change in intrathoracic pressure has not been correlated with an increase in the clearance of bronchial secretions. Andersen (1987, personal communication) hypothesized that the air-filled alveoli would buffer increases in intrathoracic pressure and markedly reduce the mechanical effect of chest clapping.
Some studies (Campbell et al 1975, Wollmer et al 1985) have demonstrated an increase in airflow obstruction when chest clapping is included in an airway clearance regimen, but other studies (Gallon 1991, Pryor & Webber 1979) have shown no increase in airflow obstruction with chest clapping.
Chest clapping has been shown to cause an increase in hypoxaemia (Falk et al 1984, McDonnell et al 1986) when performed for short periods only (less than 30 seconds) but when combined with three to four thoracic expansion exercises there was no decrease in oxygen saturation (Pryor et al 1990).
In a group of clinically stable patients with cystic fibrosis, no advantage was shown when self-chest clapping was used in addition to thoracic expansion exercises (Webber et al 1985), but this cannot be extrapolated to either all medical chest conditions or to acute chest problems.
If a patient feels that self-chest clapping is beneficial but the physiotherapist thinks it is tiring and may be causing hypoxaemia, the patient should be monitored using an oximeter. If oxygen desaturation of clinical significance occurs during the self-chest clapping, the patient should be encouraged to omit the clapping but to continue with the thoracic expansion exercises. Patients studied by Carr et al (1995) felt that self-chest clapping was useful when they were clinically stable, but more particularly when they were unwell. The benefits of chest clapping remain uncertain, but if chest clapping is considered to be clinically beneficial for an individual it should be continued, provided there are no adverse effects.
Chest shaking, vibrations and compression
The therapist’s hands are placed on the chest wall and, during expiration, a vibratory action in the direction of the normal movement of the ribs is transmitted through the chest using body weight. This action augments expiratory flow (McCarren & Alison 2006) and may help to mobilize secretions. It is unknown whether airway closure will be increased if the vibratory action is continued into the expiratory reserve volume, but these techniques are frequently combined with thoracic expansion exercises, which would be likely to counteract any resulting airway closure.
The vibratory action may be either a coarse movement (chest shaking) or a fine movement (chest vibrations). Physiotherapists have tended to adopt the techniques that they find the most helpful clinically. Vibrations are commonly used in infants and children, where the chest wall is more compliant than in adults (Chapter 10). Chest vibrations and shaking should never be uncomfortable and should be adapted to suit the individual patient. Some patients, doing their own chest physiotherapy, find self-chest vibrations helpful. One hand is placed on top of the other on the appropriate part of the chest wall and vibrations or shaking are carried out during expiration. With the hands in a similar position, chest compression throughout expiration may be helpful to augment the forced expiratory manoeuvre of the huff. When in side lying, selfcompression can be given over the side of the chest with the upper arm and elbow and the hand of the other arm.
The physiotherapist or the patient’s carer may give compression during huffing or coughing. Some patients find this helpful, but others prefer to be unsupported. Postoperative patients usually find that supporting the wound facilitates both huffing and coughing (Fig. 5.8). With fractured ribs and other chest injuries, shaking of the chest wall would be inappropriate but compressive support may assist the clearance of secretions.
In the paralysed patient the technique of rib springing may be used, where compression of the chest wall is continued throughout expiration and overpressure is applied at the end of the breath out. By releasing the hands quickly, inspiration is encouraged. This technique is inappropriate in the non-paralysed patient and may be harmful as compression against a reflexly splinted chest wall may produce rib fractures. Assisted coughing for the paralysed patient is described in Chapter 16.
In the drowsy, semicomatose patient (for example, the chronic bronchitic in respiratory failure with sputum retention), chest compression similar to, but less vigorous than, rib springing may stimulate a deeper inspiration. Chest shaking or chest vibrations are often used during the expiratory phase of a manual hyperinflation treatment to assist the clearance of secretions (Chapters 8 and 10). Care must be taken when using the techniques of chest shaking, vibrations and compression if there are signs of osteoporosis or metastatic deposits affecting the ribs or vertebral column.
A study by McCarren & Alison (2006) of people with cystic fibrosis compared the expiratory flow rates and frequencies of airflow oscillation of vibration and percussion (chest clapping) with positive expiratory pressure and the oscillating positive expiratory pressure of the Flutter® and Acapella®. They concluded that vibration produced greater expiratory flow rates and a higher peak expiratory/peak inspiratory flow ratio, although the Flutter® and Acapella® had higher oscillation frequencies. Their clinical recommendation was that if patients were unable to cough or huff effectively, vibration could be used.
High-frequency chest wall oscillation
High-frequency chest wall oscillation (HFCWO) (also known as high-frequency chest wall compression (HFCWC) or high-frequency chest compression (HFCC)) commonly provides compression of the chest wall at frequencies of 5–20 Hz. Usually this compressive force is created using an inflatable jacket adjusted to fit snugly over the thorax. This is linked to an air-pulse generator, which delivers intermittent positive pressure airflow into the jacket. As a result the jacket rapidly expands, compressing the chest wall, producing a transient (hence oscillatory) increase in airflow in the airways (Fig. 5.13).
It is hypothesized that mucus clearance is enhanced as a consequence of this airflow oscillation and vibration of the airway walls. The proposed mechanism is that increased mucus / airflow interaction leads to increased cough-like shear forces and decreased mucus viscoelasticity (King et al 1983, Tomkiewicz et al 1994). Furthermore, HFCWO creates an expiratory bias to airflow and it is hypothesized that this promotes movement of mucus downstream toward the mouth. It has also been suggested that HFCWO may enhance ciliary activity (Chang et al 1988, Freitag et al 1989, Hansen et al 1994, King et al 1984, 1990).
There is short-term evidence to support increased mucociliary clearance with HFCWO in patients with cystic fibrosis. Some studies have demonstrated a significant increase in sputum clearance after HFCWO in comparison with baseline or control, but no significant difference in efficacy between HFCWO and other airway clearance techniques including postural drainage and percussion (PD&P), positive expiratory pressure (PEP) and high-frequency oral oscillation (HFOO) (Braggion et al 1995, Scherer et al 1998). Other studies, comparing HFCWO with PD&P, have demonstrated significantly more sputum clearance with HFCWO over PD&P (Hansen & Warwick 1990, Kluft et al 1996). Benefits in airway clearance with HFCWO have also been reported in other conditions including asthma, chronic obstructive pulmonary disease, neuromuscular disease, postoperative patients and those requiring long-term ventilatory support (Allan et al 2003, Chiappetta & Beckerman 1995, Perry et al 1998, Wen et al 1996, Whitman et al 1993).
Different studies have used different protocols in the application of HFCWO (Arens et al 1994, Braggion et al 1995, Darbee et al 2005, Kluft et al 1996, Oermann et al 2001, Stites et al 2006, Varekojis et al 2003, Warwick & Hansen 1991, Warwick et al 2004). Most commonly, a total treatment time of 30 minutes covering six frequencies between 6–25Hz has been used and standard manufacturers’ guidelines suggest 10–30 minutes of total treatment time (Electromed 2006, Hill-Rom 2006). Early animal studies found 13 Hz to be an optimum treatment frequency (Gross et al 1985, King et al 1983) and some manufacturers suggest 10 minutes each at 10, 12 and 14 Hz (Electromed 2006). However, more recently it has been recommended that an individual ‘tuning’ method should be used to identify optimum treatment frequencies, which vary among individuals and according to the waveform of the machine used (Milla et al 2006).
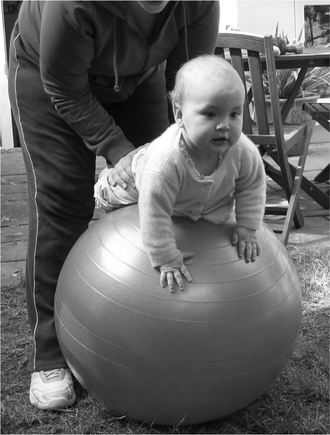
Infants and young children
For infants and young children regular physical activity is important, not just for airway clearance but for the many other benefits it provides. Physical activity is possible even in the infant, for example, playing on a gym ball (Fig. 5.14). In babies who have a chronic respiratory disorder (with increased airway secretions) an additional airway clearance technique may be necessary (e.g. modified postural drainage and percussion, positive expiratory pressure (PEP) or assisted autogenic drainage (AD)). For young children, trampolining (Fig. 5.15) and, when they are able to cooperate, bubble PEP (Fig. 5.24) are fun. At an older age, other airway clearance techniques can be added.
Insufflation/exsufflation-assisted cough
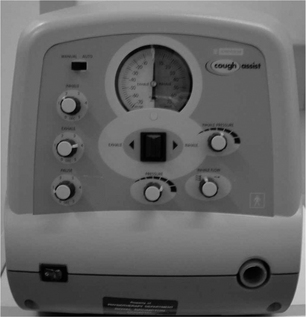
A mechanical insufflator/exsufflator uses positive pressure to deliver, to the upper airway, a maximal lung inhalation followed by an abrupt switch to negative pressure. The rapid change from positive to negative pressure is aimed at simulating the airflow changes that occur during a cough, thereby assisting sputum clearance. In 1953 various portable devices were manufactured to deliver mechanical insufflation/exsufflation (e.g. OEM Cof-flater portable cough machine, St Louis). The most commonly used mechanical insufflator/exsufflator today is the CoughAssistTM (Emerson, Massachusetts) (Fig. 5.16). Initial investigations showed mechanical insufflation/exsufflation to be effective at removing foreign bodies from anaesthetized dogs (Bickerman 1954).
Beck & Barach (1954) demonstrated clinical and radiographic improvements in 92 of 103 acutely ill patients with respiratory tract infections, with the use of mechanical insufflation/exsufflation. Seventy-two patients had bronchopulmonary lung disease and 27 had chest wall or neuromuscular disease. Improvement was more evident in patients with neuromuscular disease. The cardiovascular effects of mechanical insufflation/exsufflation were evaluated by Beck & Scarrone (1956) who found that patients demonstrated an increase in mean heart rate of 17 beats per minute and an increase in systolic blood pressure of 8 mmHg. There was also an increase in cardiac output of 2.1 litres per minute and echocardiograph changes reflective of rotation of the heart during normal coughing.
Mechanical insufflation/exsufflation has been shown to increase peak cough flow (PCF) in patients with neuromuscular disease (Bach 2003, Chatwin et al 2003, Mustfa et al 2003, Sancho et al 2004, Sivasothy et al 2001). An increase in PCF is thought to improve the efficacy of the cough and thus assist in secretion removal. Mustfa et al (2003) and Sancho et al (2004) found a significant improvement from baseline PCF with mechanical insufflation/exsufflation for both bulbar and non-bulbar motor neuron disease patients, although non-bulbar patients had the greatest change in PCF. Mechanical insufflation/exsufflation has not been shown to increase PCF in patients with chronic obstructive pulmonary disease (Sivasothy et al 2001, Winck et al 2004).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree