Peripheral Venous Systems
I. LOWER EXTREMITY VEINS
A. Anatomy
1. During inspiration, intrathoracic pressure decreases, intraabdominal pressure increases, outflow from the peripheral veins decrease, and blood moves from the abdomen to the chest. During expiration, intrathoracic pressure increases, intraabdominal pressure decreases, and outflow from the peripheral veins increases (Fig. 5.1). Several factors determine the rate of blood that returns to the heart, including the following:
a. The calf muscle pump
b. Venous valves
c. Respiratory related pressures in the thorax
d. Venous pressure
e. Cardiac factors
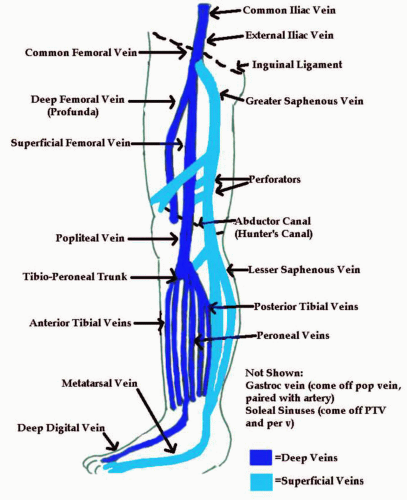
2. The venous system in the lower extremity is composed of a deep venous system and a superficial venous system. In the lower extremity, blood flows from the superficial system to the deep system. The reverse is true for the upper extremity.
3. The superficial system in the lower extremity is composed of the greater and lesser saphenous veins and their branches. The greater saphenous vein extends into the subcutaneous tissues from the medial aspect of the common femoral vein (at the level of the proximal thigh) to the level of the foot. The normal diameter of the greater saphenous vein is 3 to 5 mm at the level of the saphenofemoral junction and 1 to 3 mm at the level of the ankle. The lesser saphenous vein extends into the subcutaneous tissues from the posterior aspect of the popliteal vein to the level of the ankle. The diameter of the lesser saphenous vein is normally 2 to 4 mm at the level of the saphenopopliteal junction and 1 to 2 mm at the level of the ankle.
4. The deep system in the lower extremity is composed of the common femoral vein, the superficial femoral vein, the deep femoral vein, the popliteal vein, the posterior tibial veins, the anterior tibial veins, and the peroneal veins.
5. The external iliac vein continues into the common femoral vein at the level of the inguinal ligament. The common femoral vein lies just medial and slightly deep to the common femoral artery. Several centimeters distal to the bifurcation of the common femoral artery and 6 to 8 cm distal to the level of the inguinal ligament, the common femoral vein bifurcates into the superficial and deep femoral veins.
6. The deep femoral vein (also known as the profunda) lies medial to the deep femoral artery and extends deep and laterally. Usually only the proximal portion can be seen.
7. The superficial femoral vein lies medial and slightly deep to the superficial femoral artery. It is deep and just posterior to the superficial femoral artery as the vein proceeds down the medial thigh into the adductor canal. The adductor canal is formed by a separation in the tendinous insertion of the adductor magnus muscle. Since the canal is deep in the medial thigh and consists of dense tissue, it is often difficult to visualize the distal superficial femoral vein in larger patients.
8. The distal superficial vein turns into the popliteal vein as it enters the popliteal space behind the knee. The popliteal vein lies anterior to the popliteal artery.
9. The first deep branches of the popliteal vein are the anterior tibial veins. These veins are paired and travel with the anterior tibial artery along the anterior surface of the interosseous membrane in the front of the leg to the dorsal aspect of the foot.
10. The next branch of the popliteal vein is the tibioperoneal trunk, which quickly divides into the posterior tibial veins and the peroneal veins.
11. The posterior tibial veins are paired and travel with the posterior tibial artery along the medial and posterior area of the lower leg, posterior to the tibia.
12. The peroneal veins are paired and travel with the peroneal artery along the lateral and posterior region
of the lower leg, medial to the posterior aspect of the fibula.
of the lower leg, medial to the posterior aspect of the fibula.
13. The gastrocnemial veins and soleal veins (or sinuses) are deep veins that drain the gastrocnemius muscle and the soleal muscle. The gastrocnemius veins are paired with an artery and they drain into the popliteal vein. The soleal sinuses do not have arteries that accompany them and vary in size and extent. They drain into the posterior tibial veins and the peroneal veins. Venous sinuses act as a reservoir for venous blood and are an important part of the calf muscle pump.
14. The perforators (or communicating veins) connect the deep and superficial veins. The majority of perforating veins can be seen passing through the subcutaneous tissues to the deep tissues of the medial calf. Normal perforating veins are difficult to visualize due to their small size. Insufficient perforating veins can be visualized with the patient in the upright position.
15. There are 100 to 200 valves in each leg. The soleal sinuses do not have valves.
B. Pathology
1. Deep venous thrombosis (DVT)
a. Millions of individuals are affected each year in the United States with DVT. Up to 50% will develop a pulmonary embolism. It is the third leading cause of death in the United States, with over 1 million deaths attributed to it each year. It is estimated that approximately 90% of all pulmonary emboli originate in the leg or pelvis.
b. Major risk factors for developing DVT are the Virchow triad:
(1) Stasis
(2) Trauma
(3) Hypercoagulability (can be due to pregnancy, cancer, estrogen intake/birth control pills, or myeloproliferative disorders)
c. Those with increased risk for DVT include the elderly, postsurgical patients, cancer patients, and posttraumatic patients.
d. Valvular incompetence and pulmonary emboli are the most frequent complications of DVT.
e. As the risk for DVT increases, so does the risk for pulmonary emboli. Pulmonary emboli are rare in healthy ambulatory patients and when DVT exists below the knee. Some cases of DVT originate below the knee and progress to higher regions of the leg. Once thrombus is found above the knee, the risk for pulmonary embolism increases significantly.
f. The major symptoms of DVT are leg swelling (edema), often seen in venous disease due to increased capillary pressure; pain and redness; and superficial varicose veins.
g. The Homans sign is the presence of calf pain when the foot is dorsiflexed. However, this is not a reliable symptom for DVT. The clinical symptoms alone are not enough to diagnose DVT.
h. For every 100 patients with symptoms of DVT, there are 15 to 35 patients who do not have DVT but some other vascular disorder or nonvascular problem. In diagnosing DVT, the clinical findings are about 50% accurate. Other causes of redness, pain, and swelling of the lower extremities can include: a muscle strain or tear, a direct injury of the leg, a Baker cyst, cellulitis, lymphangiitis, congestive heart failure, extrinsic compression, and complications of chronic venous insufficiency.
i. Patients who are short of breath, have severe chest pain, and low pulse-oximetry values are suspected of having a pulmonary embolus; then the clinician should check for DVT.
j. Anticoagulation is the number one way to treat DVT. Types of anticoagulants are heparin and coumadin. Thrombolytic therapy, which includes streptokinase and urokinase, is another treatment method used to dissolve the clot. A thrombectomy can be performed only when anticoagulation and thrombolytic agents don’t work and there’s a clot in the iliofemoral area or impending limb loss (as with phlegmasia cerulea dolens). A Greenfield filter may also be placed in the inferior vena cava to decrease
the risk for pulmonary embolism in a patient that has DVT and cannot be anticoagulated.
the risk for pulmonary embolism in a patient that has DVT and cannot be anticoagulated.
k. Some unusual forms of DVT:
(1) Phlegmasia alba dolens. Consistent with a painful, swollen white leg (“milk leg”), iliofemoral thrombosis, there is increased frequency of this in the postpartum period.
(2) Phlegmasia cerulea dolens. Consistent with a painful, swollen cyanotic (blue) leg, iliofemoral and greater saphenous vein thrombosis is the most severe form of limb thrombosis.
(3) May-Thurner syndrome. When the left common iliac vein courses posterior to the right common iliac artery, DVT more often occurs on the left side.
(4) Klippel-Trenaunay-Weber syndrome is the congenital absence or atresia of the deep veins. Some deep venous segments may be grossly enlarged.
2. Venous insufficiency
a. In many patients, venous insufficiency is caused by damage to the valves from DVT. It develops in approximately half of the patients with acute DVT.
b. With venous insufficiency, the valves fail to function properly, and blood is allowed to flow in the incorrect direction (reflux).
c. When there is valvular incompetence, the hydrostatic pressure is sufficient enough to distend the veins (which are highly elastic) and the blood is allowed to pool.
d. Chronic stasis causes the veins to become inflamed. Expansion of the veins exerts pressure on the surrounding tissues causing pain. The constant pooling of the blood and the increased hydrostatic pressure causes fluid to leak out into the tissues (edema).
e. Symptoms of venous insufficiency:
(1) Deep vein incompetence is associated with pain or swelling or both.
(2) Perforator incompetence is associated with swelling and skin changes in the gaitor zone (the medial ankle can be red to purple or brown).
TABLE 5.1. THE DIFFERENCE BETWEEN ARTERIAL AND VENOUS ULCERS | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
(3) Superficial incompetence is associated with varicose veins.
(4) Venous stasis ulcers may form near the medial malleolus (Table 5.1).
(5) It is important to determine whether a person has primary or secondary varicose veins:
(a) Primary varicose veins are due to hereditary weakness or absence of valves and can be aggravated by pregnancy and obesity.
(b) Secondary varicose veins are due to disease in the deep system.
(6) Venous insufficiency can be treated medically or surgically. If there is only superficial incompetence, varicose veins can be removed by sclerosing or vein stripping. Compression cuffs on the legs (which mimic the muscle pump) or elastic support stockings can be used.
f. Causes of venous insufficiency:
(1) Occasionally the calf muscle pump itself may not produce enough energy to give adequate venous return. This happens with patients who are paraplegic, inactive, or sitting for long periods of time. They become prone to phlebitis and eventually DVT.
(2) A congenital defect of the valve cusps not opposing each other when they are closed causes reflux down the superficial veins. If the patient has increased venous pressure due to heart or pulmonary hypertension or congestive heart failure, reflux is increased and produces symptoms.
(3) A previous DVT episode causes the veins to enlarge so that the valve cusps no longer coapt. This leads to valve incompetency. Also, the valves may become thickened and small bits of chronic DVT adhere to the valves, preventing closure. When deep vein valves are destroyed, the calf pump enlarges, causing increased intravenous pressure, the perforator valves become nonfunctional due to increased pressure, then the superficial venous system becomes incompetent as the increased pressure and volume is transferred.
3. Lymphedema. Lymphedema is painless, firm swelling that progresses over time. The patient may develop recurrent bouts of cellulitis. Primary lymphedema
is idiopathic and/or congenital. Secondary lymphedema is due to an obstruction or inflammation.
is idiopathic and/or congenital. Secondary lymphedema is due to an obstruction or inflammation.
4. Cellulitis. Cellulitis is an infection of the dermal tissues of the limb. It results in increased blood flow to the leg. It presents with hot and red tissues, often in the shin and top of the foot.
C. History: Questions to Ask the Patient
1. About half of the people with DVT have no symptoms at all. Pulmonary embolism may be the first indication that something is wrong. Ask:
a. Have you had any pain in your legs?
b. Have you had any swelling in either leg? If you have, is it worse late in the day?
c. Have you ever had any blood clots in your legs?
d. Have you had any recent surgery?
e. Have you taken any long trips?
f. Have you recently given birth?
g. Do you take birth control pills or hormone replacement therapy?
h. Have you ever had any skin discolorations or an ulcer on either leg?
i. Does either leg feel hot to the touch?
j. Do you have cancer?
k. Do you have any myeloproliferative disorders?
2. Evaluate the patient’s legs for any swelling, discolorations (may be brown in color), lesions, ulcers, redness (or other color changes such as blue or white), whether they feel hot to the touch, and superficial varicose veins. Have the patient dorsiflex the foot to see if he or she develops pain in the calf (Homans sign). Feel for any lumps—swollen lymph nodes support the diagnosis of cellulitis. Feel for any palpable “cords,” which is actually a thrombosed superficial vein.
D. Diagnostic Examinations
1. Duplex Doppler examination
a. Begin with the patient in the supine or in the reverse Trendelenberg position, with the leg bent slightly and relaxed out to the side.
b. Using a 5.0- to 7.0-MHz transducer in the transverse plane, start to image just above the crease of the groin.
c. Locate the common femoral vein. Evaluate the vein by compressing it until it is collapsed completely.
d. Continue in this fashion down the leg, evaluating the other vessels, compressing every 2 to 3 cm (Fig. 5.2).
e. When you get to the popliteal vein, slide your transducer behind the patient’s knee. This posterior approach will place the vein anterior to the artery on the screen.
f. The posterior tibial and peroneal veins may be evaluated by placing the transducer on the medial surface of the lower leg and sliding up from the ankle. With this approach, these veins are located between the tibia and the fibula. The posterior tibial veins are more anterior and just beneath a fascial plane connecting the tibia and the fibula. The peroneal veins are more posterior and just anterior and medial to the fibula.
g. You may also follow the calf veins in a posterior approach as they split off the popliteal vein. The anterior tibial vein may be found by placing the transducer on the anterior surface of the lower leg. They are located between the tibia and fibula, just anterior to the fascial plane between the two bones. They resemble “ants on a bridge.” Check for masses pressing on the veins (Baker cysts or lymph nodes.)
h. Obtain compression/noncompression gray scale images, color images, and duplex Doppler signals with augmentation (squeezing of the distal body part to cause a sudden rush of flow) of the following vessels:
(1) Common femoral vein with the origin of the greater saphenous vein (Fig. 5.3)
(2) Proximal superficial femoral vein with deep femoral vein (Fig. 5.4)
(3) Middle superficial femoral vein (Fig. 5.5)
(4) Distal superficial femoral vein (Fig. 5.6)
(5) Popliteal vein (Fig. 5.7)
(6) Posterior tibial veins (Fig. 5.8)
(7) Peroneal veins
(8) Anterior tibial veins, if necessary (Fig. 5.9)
i. In addition, the common femoral vein may be interrogated with Doppler while the patient performs the Valsalva maneuver. This indirectly evaluates for obstruction in the pelvic veins.
j. The calf is not always evaluated in some medical centers since it is rare for DVT in the calf to cause pulmonary emboli. However, in other places it is evaluated routinely due to the 20% incidence of the clot traveling further up the leg, as well as the increased incidence of significant venous insufficiency after untreated calf DVT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree