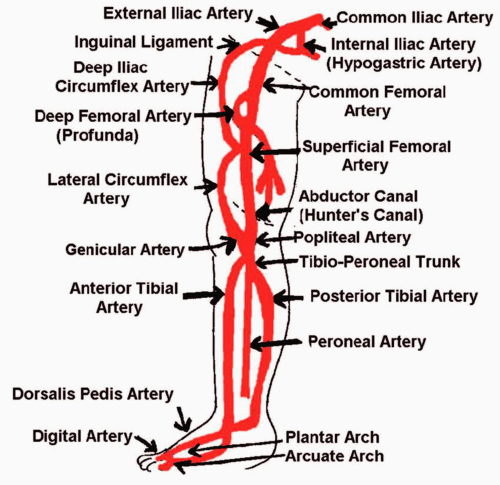
Peripheral Arterial Systems
I. LOWER EXTREMITY ARTERIES
A. Anatomy
(Fig. 3.1)
1. The common iliac arteries divide into the external and internal (hypogastric) iliac arteries at the level of the lumbosacral junction.
2. The internal iliac arteries are 3 to 4 cm in length. The branches of these arteries supply the pelvic wall, perineum, pelvic organs, and gluteal region.
3. The external iliac arteries are larger than the internal iliac arteries in an adult. When it passes underneath the inguinal ligament, the external iliac artery becomes the common femoral artery. The two branches of the external iliac artery are the inferior epigastric artery (supplying the abdominal muscles and skin) and the deep circumflex artery (supplying the abdominal muscles.)
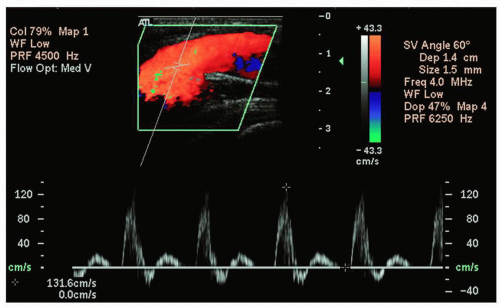
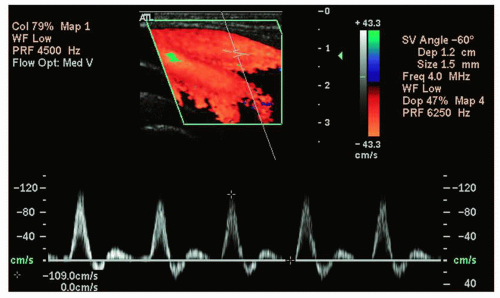
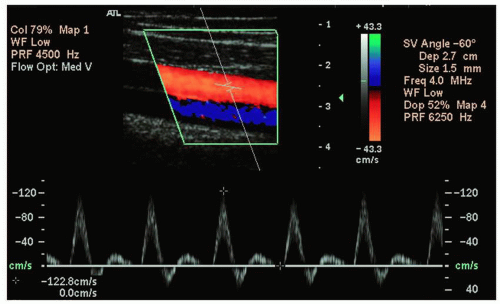
4. The common femoral artery (Fig. 3.2) divides into the superficial femoral artery and the deep femoral artery (profunda) (Fig. 3.3).
5. The superficial femoral artery (Fig. 3.4) passes through the adductor canal (Hunter’s canal) and enters the popliteal fossa. Here it becomes the popliteal artery.
6. The popliteal artery divides into the anterior tibial artery and the tibioperoneal trunk.
7. The anterior tibial artery is the first branch off the popliteal artery. It runs along the anterior surface of the interosseous membrane in the front of the leg. The anterior tibial artery becomes the dorsalis pedis artery in the foot.
8. The tibioperoneal trunk is the second branch off the popliteal artery. It quickly divides into the posterior tibial and peroneal arteries.
9. The posterior tibial artery extends down the medial and posterior region of the lower leg. It divides into the medial and lateral plantar arteries in the foot.
10. The peroneal artery extends down the lateral and posterior region of the lower leg, along the fibula.
11. The plantar arch consists of the deep plantar artery (branch of the dorsalis pedis) and the lateral plantar artery (branch of the posterior tibial artery). The plantar arch and the dorsal metatarsal arteries supply the digits.
B. Pathology
1. Arteriovenous fistulas
a. Arteriovenous fistulas can be either congenital or iatrogenic (caused by surgery and/or procedures involving puncture into an artery or a vein such as catheterization.)
b. These are abnormal communications between an artery and a vein.
2. Pseudoaneurysms
a. A pseudoaneurysm is a small pocket of moving blood connected to an artery through a small opening (the neck) and may be partly surrounded by thrombus.
b. These form due to interventional radiology procedures (e.g., cardiac catheterization using the common femoral artery), trauma, surgery, or infection. They can be felt as a pulsatile mass.
c. Compression with a transducer may help to clot the pseudoaneurysm off. An alternative therapy would be thrombin injection.
3. Peripheral artery aneurysms
a. Peripheral artery aneurysms develop when the wall of the artery weakens.
b. These are defined as a bulge or focal enlargement of 20% of the diameter of the vessel.
c. They are most likely to develop in the distal superficial femoral artery or the popliteal artery.
d. These may be bilateral and may be asymptomatic.
e. Thrombus may be present within the aneurysm.
f. A peripheral artery aneurysm that is 2 cm or greater in diameter usually requires repair.
4. Entrapment of the popliteal artery by the gastrocnemius muscle. This is a rare problem that is due to an abnormally positioned insertion of the muscle. It usually occurs in young men. Only a third of cases are bilateral.
5. Compartment syndrome. This is a collection of symptoms that are produced by an obstruction of a portion of the blood supply and increased pressure (often in the calf). This can be caused by an increase in blood (deep venous thrombosis, hemorrhage) or serous fluid (edema, lymph fluid) within the compartment. This can occur after revascularization of the calf artery due to prolonged acute ischemia. The most effective treatment is surgical opening of compartment to relieve pressure. Angiography is often used.
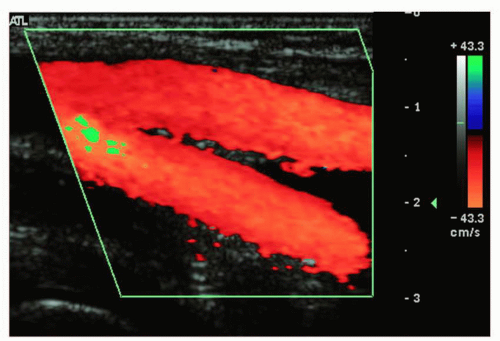 FIGURE 3.3. Sagittal color flow image of the right proximal superficial femoral artery and the deep femoral artery. |
6. Chronic occlusive lower extremity arterial disease
a. Causes:
(1) Atherosclerosis obliterans (ASO). Ninetynine percent of all chronic vascular disease in the United States is caused by ASO. ASO is the accumulation of plaque in the arterial system. Initially fibrous plaque is deposited under the intima. Fatty streaks may also appear under the intima. Eventually, it degenerates and forms complex plaque (fibrous material, plaque, and calcium). Ulcerations may occur which can hemorrhage.
(2) Thromboangiitis obliterans (TAO), also known as Buerger disease—A disease that causes inflammation of the arteries (or veins) preventing blood flow. Always starts in the plantar or palmar vessels and proceeds centrally, preventing collaterals from forming.
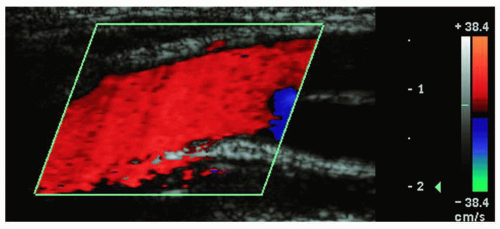
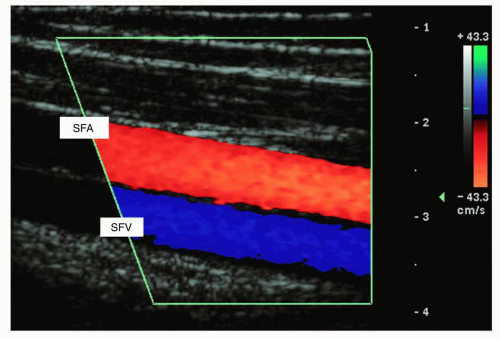 FIGURE 3.4. Sagittal color flow image of the right middle superficial femoral artery (SFA, red) and vein (SFV, blue). |
(3) Smoking history, hyperlipidemia, family history, diabetes, and hypertension—All these are precursors to peripheral arterial disease.
b. Symptoms:
(1) Claudication—pain produced by exercise (most common site is the calf) and relieved by rest. During exercise, there is an increased demand for blood to the muscles. Diseased arteries and collaterals cannot deliver the appropriate amount of blood needed (the arterioles are already dilated due to their diseased state). Pain occurs due to oxygen-starved muscles, and is relieved by rest.
(2) Instep claudication (in the foot)—produced by TAO. This causes severe pain.
(3) Rest pain is most severe at night, is due to more advanced disease, and is more commonly felt in the toes and top of the foot. Limbs must be lowered so gravity pulls more blood down to the muscles.
(4) Loss of hair on the lower extremities.
(5) Thickening and color changes of the toenails.
(6) Changes in skin color and appearance (tight, shiny skin).
(7) Decreased palpable pulses.
(8) Abnormal sensations in the affected limb (pins/needles, tingling).
(9) Redness of the foot due to dilated arterioles is present with more advanced disease.
(10) Evidence of a bruit or a thrill (abnormal noise). In severe stenosis (>90%) the bruit disappears because arterial flow decreases to the point that there is no longer any tissue vibration.
(11) Arterial ulcers—These may become gangrenous and are present with more advanced disease.
7. Acute occlusive lower extremity arterial disease
a. Causes:
(1) Physical compression or obstruction of a major artery.
(2) Entrapment by the gastrocnemius muscle on the popliteal artery.
(3) Obstruction caused by emboli—these may be thrown from a diseased heart valve or an aortic aneurysm.
(4) Hypercoagulation—certain chemotherapies or malignant diseases can cause this.
(5) Dissection of the intimal lining of a vessel—the flap may completely occlude blood flow.
(6) Masses or severe hemorrhage following trauma.
b. Symptoms:
(1) Pain—severe, unilateral claudication during exercise is a symptom of entrapment by the gastrocnemius muscle.
(2) Paralysis.
(3) Paresthesias—abnormal sensations within the affected limb.
(4) Pallor—pale skin tone, cool to the touch (hot to the touch may be caused by deep venous thrombosis).
(5) Absence of a pulse.
(6) Black toes—caused by thrown emboli or hypercoagulation. “Blue toe syndrome”—emboli lodged in the digital arteries causes cyanosis. Arteritis, ulcerated lesions, and sometimes angiography can cause this.
8. The most frequent sites of claudication and their indicated levels of disease:
a. Buttocks—this site indicates aortoiliac arterial disease.
b. Thighs—this site indicates iliac and/or common femoral artery disease.
c. Calves—this site indicates femoropopliteal arterial disease.
9. Sites of lower extremity occlusive disease and their effects:
a. The most common site of lower extremity occlusive arterial disease is the distal superficial femoral artery in the adductor canal. If there is only an isolated site of disease, it rarely produces symptoms of claudication due to proximity of branches from the deep femoral artery as well as pelvic and calf arteries that allow blood to flow from the pelvic area or upper thigh to the calf without using the superficial femoral artery. Also, the potential for collateralization in the thigh to the calf is very great.
b. The second most common site is the aortoiliac area. If the distal aorta is obstructed, it is possible for the blood to get to the external iliac arteries by way of branches given off by the internal iliac arteries. This would produce reverse flow in one or both internal iliac arteries. This would produce symptoms of claudication since the volume flow capacity of collaterals is much lower than the volume flow capacity of the aorta. Also, it is possible for one or both of the common iliac arteries to be occluded. If one is occluded, collaterals from the other side may provide blood flow. If both common iliac arteries were occluded, then the superior mesenteric artery, inferior mesenteric artery, lumbar arteries, or other collaterals would have to be used. This also produces symptoms of claudication. Bifurcations are common sites for arterial disease because of the turbulence that occurs at these sites.
c. If there is disease in the popliteal artery, collaterals from the deep femoral artery or genicular artery may alleviate symptoms of claudication. (The genicular arteries course from the superficial femoral arteries, run parallel to the superficial femoral arteries and the popliteal arteries, and anastomose at several sites along these arteries.)
d. Below the trifurcation (into the posterior tibial, anterior tibial, and peroneal arteries), single site disease is rarely significant due to the rich communications between the calf muscles. Symptoms are rarely produced.
C. History: Questions to Ask the Patient
1. The vascular laboratory must answer three basic questions:
a. Are the patient’s symptoms due to vascular disease?
b. How extensive is the vascular disease present?
c. Where is the disease located within the affected limb?
2. Questions to ask the patient:
a. Do you get pain in either leg upon exercising and does rest relieve it?
b. How far can you walk before the pain starts? (Number of blocks.)
c. Where exactly in your leg(s) is the pain present? (Site of pain is usually distal to the site of the occlusive disease.)
d. Is the pain present in both legs? Is one leg worse than the other?
e. Do you get pain in your toes, feet, or legs at night when you rest?
f. How long have you had this sore/ulcer?
g. Do you feel pins/needles or tingling in your limb?
h. Do you have diabetes? If so, what kind (non-insulin-dependent diabetes mellitus or insulin-dependent diabetes mellitus)? The presence of diabetes increases the chance of peripheral vascular disease by at least eight times. It is not unusual for diabetics to have a slow-healing ulcer on the sole of the foot. A problem with diabetics is neuropathy—neurons are damaged in extremities, causing pain, and the pain may or may not be related to vascular disease.
i. Do you have hypertension? If yes, are you taking medication to control your hypertension? Hypertension is a major source of stress to the vascular system and can accelerate the atherosclerotic process.
j. Do you have high cholesterol? Is heart disease present in you or your family? Have you ever had a stroke?
k. Do you smoke? If so, how many packs per day? For how many years? The risk for arterial disease increases dramatically as the number of years smoking and the number of packs per day increase. Decreased oxygen in the blood may produce symptoms of claudication. Nicotine adversely affects the endothelium and causes vasoconstriction.
3. Physical examination of the patient:
a. Look at the skin for any lesions/ulcers, redness, pallor, tightness and shininess, loss of hair, thickening and color changes of the toenails, color changes in the toes, and whether the skin feels cool, hot, or warm to the touch.
b. Feel for pulses in the common femoral arteries, popliteal arteries, posterior tibial arteries and the dorsalis pedis arteries. Grade the pulses according to
0 for absent; 1 for intermittent or unsure; 2 for weak; 3 for full and bounding.
0 for absent; 1 for intermittent or unsure; 2 for weak; 3 for full and bounding.
c. Feel for lumps (swollen lymph nodes) that support the diagnosis of cellulitis, which is an infection of the dermal tissues in the limb and presents with hot and red tissues often in the shin and the top of the foot.
d. Feel for thrills or vibrations, which could indicate an aneurysm, pseudoaneurysm, or an arteriovenous fistula.
e. Pseudoaneurysms are often felt as a pulsatile mass.
4. The severity of symptoms depends on:
a. The degree of arterial obstruction within the limb.
b. The degree of collateralization. Symptoms in legs with vascular causes are the result of “regional hypotension.” Collaterals take time to develop, so acute disease can be more painful than chronic disease.
5. Four appropriate places for arterial auscultation:
a. Carotid artery
b. Abdominal aorta
c. Femoral artery
d. Popliteal artery
6. Three conditions that can produce a palpable thrill or vibration:
a. A patent hemodialysis graft.
b. Poststenotic turbulence.
c. Arteriovenous fistula. Flow in the proximal artery greatly increases (especially during diastole) because the fistula causes a marked decrease in resistance. Flow in the proximal vein also increases and is more pulsatile.
D. Diagnostic Examinations
1. Duplex Doppler examination:
a. Begin with the patient in the supine position, with his or her leg bent slightly and relaxed out to the side. Using a 5.0- or 7.0-MHz linear-array transducer in a transverse plane, start to image just above the crease of the groin.
b. Locate the common femoral artery.
c. Slide your transducer down the leg to evaluate the other vessels. When you get to the popliteal artery, bring your transducer behind the knee. This will place the artery posterior to the vein on the screen since you are now in a posterior approach.
d. Although few protocols require a detailed look at the calf arteries, to evaluate the posterior tibial artery, slide your transducer up the medial aspect of the calf starting at the ankle.
e. The posterior tibial artery is located (with this approach) between the tibia and the fibula, just underneath a fascial plane.
f. The peroneal artery is located posterior to this.
g. The anterior tibial artery is located by placing the transducer on the anterior surface of the lower leg midway between the knee and the ankle. It is seen anterior to the fascial plane between the tibia and the fibula.
h. Obtain gray-scale images in sagittal and transverse planes, color images, and Doppler signals (maintaining a 60-degree angle of insonation) with peak systolic velocity measurements from the following vessels:
(1) Common femoral artery (Fig. 3.5)
(2) Profunda (deep femoral artery)
(4) Popliteal artery
(5) Posterior tibial artery, if necessary
(6) Peroneal artery, if necessary
(7) Anterior tibial artery, if necessary
(8) External iliac artery, common iliac artery, and distal aorta Doppler waveforms may be obtained if necessary.
2 Segmental pressure examination
(a) Due to the Bernoulli effect, segments of the limb distal to significant occlusive disease will have decreased pressures.
(b) The patient must be supine so gravity does not affect the pressures (hydrostatic pressure artifact). For every 1 cm the limb is above the heart, the pressure decreases by 0.74 mm Hg.
(c) The width of the cuff should be 20% to 25% greater than the diameter of the limb, or 40% greater than the circumference of the limb.
(d) The peak systolic pressure is obtained by placing a cuff (the widest possible) over the desired segment of the limb and inflating to a pressure that is enough to occlude any blood flow through that segment (at least 20 mm Hg past the disappearance of a Doppler-detected pulse). Slowly the cuff is deflated and any portion of the arterial system below the cuff can be used to determine the pressure of the segment beneath the cuff. (Usually dorsalis pedis and posterior tibial artery are used.) The first flow of blood is the peak systolic pressure.
(e) Different patients have different pressures, so we must normalize the pressure results from the limb to the patient’s systemic blood pressure. Usually, peak systolic pressure values from segments are divided by the higher of the two brachial peak systolic pressures.
(f) The most common index used is the ankle-tobrachial index (ABI).
(g) Disadvantages of the segmental pressure examination:
(1) You cannot discriminate between stenosis and occlusion.
(2) You cannot pinpoint the precise location of disease.
(3) When the patient is obese, the pressures may be falsely elevated. When the patient is extremely thin, the proximal thigh pressure may be falsely low. This is due to the cuff/limb ratio artifact. (The width of the cuff should be 20% to 25% greater than the width of the limb.)
(4) There is difficulty in discriminating between common femoral artery and external iliac artery disease.
(5) Calcified vessels yield falsely elevated pressures (seen with diabetics and chronic renal disease patients). An index of 1.25 or higher indicates falsely elevated pressures. Patients (mostly diabetic) who are not able to tolerate the amount of pressure required to “crush” stenotic arteries must be evaluated with other techniques such as duplex Doppler imaging or arteriography. A toe pressure using photoplethysmography (PPG) may also be used. Toe pressures are used to confirm abnormally high ABIs resulting from calcification of vessels. Toe arteries are rarely affected by atherosclerosis or calcification.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree