Chapter 55
Peripheral Arterial Disease
1. What are the key components of the vascular physical examination?
 Blood pressure measurements in both arms
Blood pressure measurements in both arms
 Carotid pulse palpation for upstroke and amplitude, and auscultation for bruits
Carotid pulse palpation for upstroke and amplitude, and auscultation for bruits
 Auscultation of the abdomen and flank for bruits
Auscultation of the abdomen and flank for bruits
 Palpation of the abdomen for aortic pulsation and its maximal diameter
Palpation of the abdomen for aortic pulsation and its maximal diameter
 Palpation of brachial, radial, ulnar, femoral, popliteal, dorsalis pedis, and posterior tibial pulses; pulse intensity is scored as follows: 0, absent; 1, diminished; 2, normal; 3, bounding
Palpation of brachial, radial, ulnar, femoral, popliteal, dorsalis pedis, and posterior tibial pulses; pulse intensity is scored as follows: 0, absent; 1, diminished; 2, normal; 3, bounding
 Performance of the Allen test when knowledge of hand perfusion is needed
Performance of the Allen test when knowledge of hand perfusion is needed
 Auscultation of the femoral arteries for the presence of bruits
Auscultation of the femoral arteries for the presence of bruits
 Inspection of the feet for color, temperature, and integrity of the skin, and for ulcers
Inspection of the feet for color, temperature, and integrity of the skin, and for ulcers
 Observation of other findings suggestive of severe PAD, including distal hair loss, trophic skin changes, and hypertrophic nails
Observation of other findings suggestive of severe PAD, including distal hair loss, trophic skin changes, and hypertrophic nails
2. Can the location of the patient’s lower extremity claudication help to localize the site of occlusive disease?
 Occlusive iliac artery disease may produce hip, buttock, and thigh pain, as well as calf pain.
Occlusive iliac artery disease may produce hip, buttock, and thigh pain, as well as calf pain.
 Occlusive femoral and popliteal artery disease usually produces calf pain.
Occlusive femoral and popliteal artery disease usually produces calf pain.
 Occlusive disease in the tibial arteries may produce calf pain or, more rarely, foot pain and numbness.
Occlusive disease in the tibial arteries may produce calf pain or, more rarely, foot pain and numbness.
3. What noninvasive tests are used in the assessment of lower limb claudication?
 Ankle-brachial index (ABI): The ankle-brachial index is the ankle systolic pressure (as determined by Doppler) divided by the brachial systolic pressure. An abnormal index is less than 0.90. The sensitivity is approximately 90% for diagnosis of PAD. (See Question 4 for further details.)
Ankle-brachial index (ABI): The ankle-brachial index is the ankle systolic pressure (as determined by Doppler) divided by the brachial systolic pressure. An abnormal index is less than 0.90. The sensitivity is approximately 90% for diagnosis of PAD. (See Question 4 for further details.)
 Pulse volume recordings (PVRs): Pulse volume recordings measure changes in volume of toes, fingers, or parts of limbs that occur with each pulse beat as blood flows into or out of the extremity. A toe-to-brachial index of less than 0.6 is abnormal, and values of less than 0.15 are seen in patients with rest pain (toe pressures of less than 20 mm Hg).
Pulse volume recordings (PVRs): Pulse volume recordings measure changes in volume of toes, fingers, or parts of limbs that occur with each pulse beat as blood flows into or out of the extremity. A toe-to-brachial index of less than 0.6 is abnormal, and values of less than 0.15 are seen in patients with rest pain (toe pressures of less than 20 mm Hg).
 Duplex ultrasonography: Duplex ultrasonography is a noninvasive method of evaluating arterial stenosis and blood flow. This method can localize and quantify the degree of stenosis. Ultrasonography is dependent on operator skill.
Duplex ultrasonography: Duplex ultrasonography is a noninvasive method of evaluating arterial stenosis and blood flow. This method can localize and quantify the degree of stenosis. Ultrasonography is dependent on operator skill.
 Transcutaneous oxygen tension measurements: These measurements are useful in assessing tissue viability for wound healing. Measurements greater than 55 mm Hg are considered normal and less than 20 mm Hg are associated with nonhealing ulcers.
Transcutaneous oxygen tension measurements: These measurements are useful in assessing tissue viability for wound healing. Measurements greater than 55 mm Hg are considered normal and less than 20 mm Hg are associated with nonhealing ulcers.
 Exercise testing: This testing determines treadmill walking time and preexercise and postexercise ABI. In those without significant PAD, the ABI is unchanged after exercise. In patients with PAD, the ABI falls after exercise. This test is more sensitive for detecting disease than a resting ABI alone.
Exercise testing: This testing determines treadmill walking time and preexercise and postexercise ABI. In those without significant PAD, the ABI is unchanged after exercise. In patients with PAD, the ABI falls after exercise. This test is more sensitive for detecting disease than a resting ABI alone.
Experts emphasize that the ABI is a continuous variable below 0.90. Values of 0.41 to 0.90 are considered to be mildly to moderately diminished; values of 0.40 or less are considered to be severely decreased. An ABI of 0.40 or less is associated with an increased risk of rest pain, ischemic ulceration, or gangrene. Patients with long-standing diabetes or end-stage renal disease on dialysis and elderly patients may have noncompressible leg arterial segments caused by medial calcification, precluding assessment of the ABI. These patients are best evaluated using digital pressures and with assessment of the quality of the arterial waveform in the PVR studies. A system for interpretation of the ABI is given in Table 55-1.
TABLE 55-1
INTERPRETATION OF THE ANKLE-BRACHIAL INDEX
| ABI | Interpretation |
| >1.30 | Noncompressible |
| 1.00-1.29 | Normal |
| 0.91-0.99 | Borderline (equivocal) |
| 0.41-0.90 | Mild to moderate PAD |
| 0.00-0.40 | Severe PAD |
ABI, Ankle-brachial index; PAD, peripheral arterial disease.
Modified from Hiatt WR: Medical treatment of peripheral arterial disease and claudication, N Engl J Med 344:1608-1621, 2001.
5. What are the recommended medical therapies and lifestyle interventions in patients with lower extremity PAD?
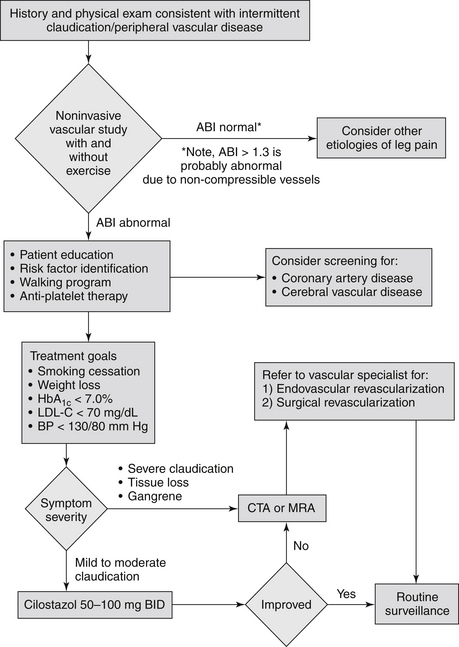
A supervised exercise regimen is recommended as the initial treatment modality for patients with intermittent claudication. Supervised exercise training is recommended over unsupervised exercise training. Cilostazol treatment can lead to a modest increase in exercise capacity. Because agents with similar biologic effects have been shown to increase mortality in patients with heart failure, this drug should not be used in patients with heart failure. Smoking cessation must be strongly emphasized to the patient. Other measures include general secondary prevention interventions. Recommended medical therapies and lifestyle interventions in patients with lower extremity PAD are summarized in Box 55-1. An algorithm for the management of patients with suspected peripheral arterial disease is presented in Figure 55-1.