Fig. 3.1
Rest ECG showing diffuse ST elevation
Cardiac echocardiography (Fig. 3.2) showed circumferential pericardial effusion and normal dimensions and function of the cardiac chambers, mild mitral regurgitation, and mild inferior vena cava (IVC) dilatation that collapses with inspiration. No signs of cardiac tamponade.
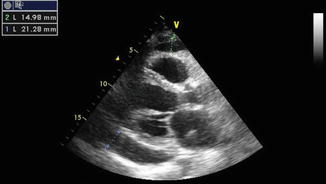
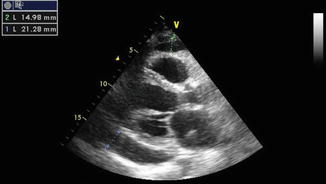
Fig. 3.2
Two-dimensional transthoracic echocardiogram showing the parasternal long-axis view. A moderate-sized pericardial effusion is present posteriorly
The thoracic CT and the clinical history showed no signs of malignancy.
After 3 days, ECG findings changed (Fig. 3.3).
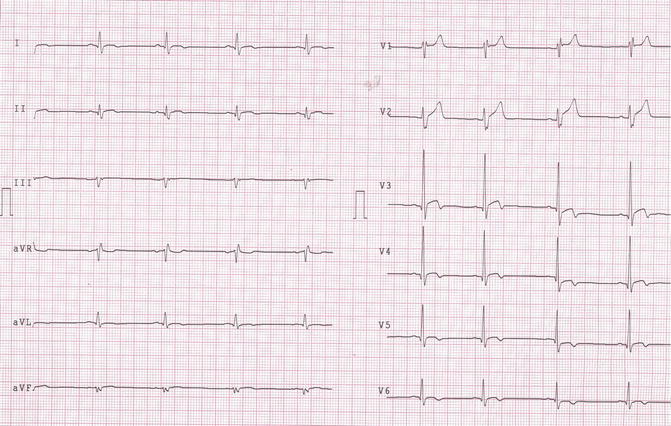
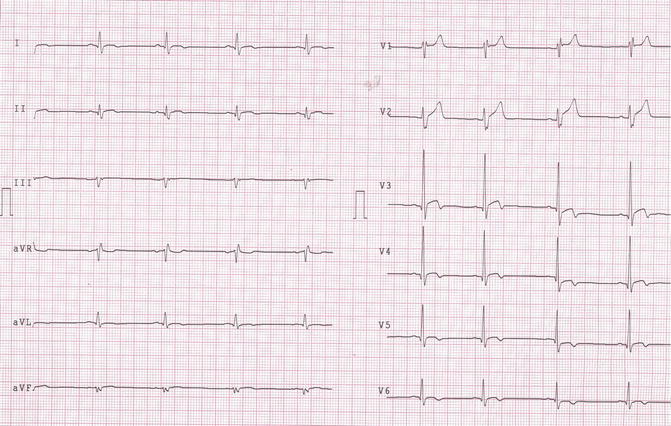
Fig. 3.3
Control ECG showing T-wave inversion in DI, aVL, V3, V4, V5, and V6
Final Diagnosis
Recurrent idiopathic acute pericarditis.
The patient was treated with colchicine in combination with nonsteroidal anti-inflammatory drugs (NSAID).
3.2 Pericarditis
Pericarditis is an inflammation of the pericardium, often with fluid accumulation. Pericarditis can be acute, chronic (defined as persistent after 6 months), and recurrent. Acute pericarditis is a common disorder with an annual incidence of 27.7 new cases per 100,000 inhabitants in Europe [1]. Nevertheless, this disease may occur as an isolated entity or manifestation of an underlying factor. Acute pericarditis is diagnosed in about 5 % of patients hospitalized to the emergency department with nonischemic chest pain [2]. In developed countries, acute pericarditis is idiopathic in 85–90 % of cases [3].
Etiology of Acute Pericarditis
Idiopathic
Infectious
Viral
Bacterial
Tuberculous
Fungal
Parasites
Neoplastic disease
Acute myocardial infarction (early pericarditis): within 1 or 3 days after a heart attack
Dressler syndrome
Autoimmune disorders
Uremia
Myocarditis
Trauma (severe injury to the chest)
Radiotherapy (especially in breast cancer and lung cancer patients)
Cardiac surgery
Adverse drug reaction (such as penicillin and chemotherapy medicines)
Clinical History and Examination
Patients with pericarditis usually report a prodrome of fever, gastrointestinal disorders, or myalgias. Typically, pericarditis comprises chest pain, ECG alterations, and laboratory signs of inflammation [4]. Absence of common inflammation markers (erythrocyte sedimentation rate and C-reactive protein) could be present in up to 20 % of cases, especially in the initial stage of the disease and with previous anti-inflammatory therapies [5]. Assessment of vital sign is important. The presence of hypotension, dyspnea, reduced cardiac tones, and signs of elevated venous tone (jugular distension, liver tenderness) may indicate cardiac tamponade, which requires an urgent treatment. Chest pain is usually of abrupt onset, stabbing or sharp, and substernal but may be radiated to arms, neck, or jaw. Chest pain is more intense in supine position and lighter in prone position. Pericardial rubs are due to the friction of inflamed pericardial layer and fibrin, auscultated usually in patients leaning frontward, at the left sternal border, throughout the whole cardiac cycle. The rub of pericarditis might be transient, and it is important for the clinicians to auscultate the heart repeatedly [6].
Electrocardiogram might be normal during pericarditis. Further, pericardial effusion can lead to a decrease in the amplitude of the QRS voltage, while the P waves are less frequently affected [7]. Nonetheless, it must be considered that low QRS voltage is a weak predictor of pericardial effusion and the correlation between the decrease in QRS amplitude and the amount of fluid is poor [8]. The etiology of changes in repolarization during pericarditis is still debated. Typical ECG alterations are divided into four stages [9]:
Stage 1: ST elevation in all standard leads except aVR and V1 with upward concavity. Elevation of more than 0.5 mV is uncommon.
Stage 2: ST segment returns to the baseline and T-wave amplitude decreases.
Stage 3: Inversion of T waves, usually not too deep.
Stage 4: Return to normal.
Depending on the time of presentation, some stages might be absent, and different stages might be present in different leads at the same time. Therefore, ST elevation and T-wave inversion can be observed simultaneously in different leads, but their coexistence in the same lead is uncommon, and it should suggest an acute coronary syndrome. A typical alteration in ECG, during pericarditis, is PR segment depression ≥0.5 mV compared to TP segment: these findings are usually an early alteration, and it is shown in almost 80 % of cases.
Chest radiography is useful to exclude secondary causes of chest pain (pneumonia, pneumothorax, traumatism) and might show enlarged heart in case of pericardial effusion.
Echocardiography has a pivotal role for the assessment of the cardiac function and presence and quantification of pericardial effusion. A large pericardial effusion with diastolic collapse of the right atrium, respiratory variation of mitral inflow (decrease in E wave of >20 % during inspiration), and dilated inferior vena cava with reduced collapsibility may suggest cardiac tamponade.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


