Pericardial Effusion and Cardiac Tamponade
Michael Yeung
High-Yield Findings
Amount of pericardial fluid (large >2 cm)
Right atrial systolic collapse (>1/3 systolic period)
Right ventricular diastolic collapse
Respiratory variation in tricuspid (>40%) and mitral (>25%) inflow
Fixed and dilated inferior vena cava (>2 cm)
Key Views
Parasternal long axis (PLAX) —initial screening of effusion/differentiation between pleural and pericardial effusion
Parasternal short axis (PSAX) —assessment of RV diastolic collapse
Apical four chamber (A4C) —use respirometer for evaluation of TV/MV respiratory variation
Subcostal —good view for sizing full extent of pericardial effusion as well as assessment of RA systolic collapse and RV diastolic collapse
Anatomy and Physiology of the Pericardium
The pericardium consists of two layers: The visceral pericardium, which is adjacent to the epicardial surface of the heart and the parietal pericardium, which is a thicker, fibrous layer that encases most of the heart.
The pericardial space, located in between these two layers, contains approximately 10 to 50 mL of pericardial fluid and allows the transmission of changes in intrathoracic pressure to the cardiac chambers. Therefore during inspiration; for example, both the intrathoracic pressure, pulmonary capillary wedge pressure (PCWP), and LV diastolic pressure fall in concert with minimal change in LV filling.
The pericardium serves as a mechanical barrier between the heart and its adjacent mediastinal structures, a lubricant between the pericardial layers as well as a mechanical restraint on cardiac volume. This restraint is the reason why pressure and volume changes of one ventricle affect the other (ventricular interdependence).
In the normal respiratory cycle, inspiration leads to a decrease in intrathoracic pressure, allowing for an increase in blood flow through the right side of the heart. Under normal conditions, the cardiac chambers and pericardium are compliant enough to accommodate for this increase in blood flow.
In tamponade ventricular interdependence is exaggerated as transmission of changes in tamponade intrathoracic pressure to the ventricles and ventricular
compliance is diminished by an increase in intrapericardial pressure. During inspiration intrathoracic pressure decreases with a decrease in PCWP. LV diastolic pressure; however, does not decrease to the same degree because of increased intrapericardial pressure. This results in a reduction in LV filling pressure (PCWP-LV diastolic pressure) and is reflected in a reduced mitral E wave peak velocity. Increased venous return and reduced LV filling promotes increased RV filling reflected in an increased tricuspid E wave peak velocity. Reciprocal changes occur during expiration where LV filling is promoted to the detriment of RV filling.
Pulsus paradoxus is a clinical manifestation of increased ventricular interdependence in tamponade, with a decrease in systolic blood pressure >10 mmHg during inspiration.
The electrocardiographic sign of electrical alternans corresponds to the pendulum-like swinging of the heart within a large pericardial effusion now that the heart is not restrained by the pericardium.
Once intrapericardial pressures exceed intracardiac pressures, chamber collapse is seen beginning with the lowest pressure chambers.
Key Point:
The rate of accumulation is just as important as the size of the pericardial effusion. A small but rapidly accumulating effusion may lead to tamponade with only 500 cc whereas a chronic effusion can accommodate up to 2000 cc of pericardial fluid before presenting with hemodynamic compromise.
Etiology of Pericardial Disease and Effusions
Idiopathic
Infectious
Viral: Echovirus, coxsackievirus, adenovirus, Hepatitis B, HIV
Bacterial: Pneumococcus, Staphylococcus, Streptococcus, Mycobacterium
Fungal: Histoplasmosis, coccidiomycosis
Immune/inflammatory
Connective tissue disease: SLE, Rheumatoid arthritis, Scleroderma
Postmyocardial infarction: Dressler’s syndrome
Uremic
Postcardiac surgery
Drug-induced: Procainamide, hydralazine, isoniazid, cyclosporine
Neoplastic disease
Direct extension: Lung carcinoma, breast carcinoma
Metastatic: Lymphoma, melanoma
Primary cardiac tumor
Mechanical
Blunt chest trauma
Procedure related: Percutaneous coronary intervention, implantation of pacemakers/defibrillators
Post-myocardial infarction free wall rupture
Differential Diagnosis of Echolucent Space Surrounding the Heart
Epicardial fat: Usually presents as an isolated echolucent area anterior to the right ventricular free wall and spares the posterior pericardium. Epicardial fat can
sometimes be identified as having a granular or specked appearance when compared to blood or pericardial fluid. Epicardial fat is more prevalent in the elderly, females, diabetics, patients with dyslipidemia and the obese.
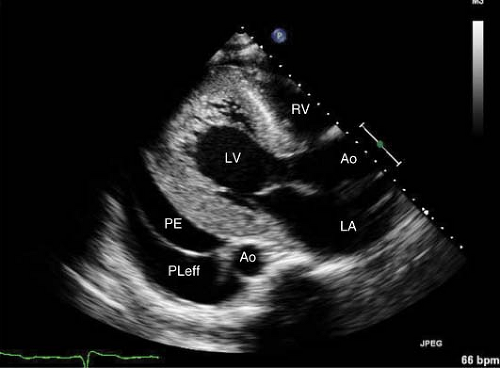
Figure 15-1. PLAX view of a pericardial effusion anterior to the descending aorta and a pleural effusion posterior to the aorta.
Pleural effusion: In the PLAX view, effusions seen anterior to the proximal descending thoracic aorta are pericardial whereas effusions that track posterior to the thoracic aorta are left-sided pleural effusions (Fig. 15-1). Left pleural effusions tend to localize primarily in the posterior–lateral aspect of the heart, while most pericardial effusions are present circumferentially unless it is loculated due to adhesions from surgery or an inflammatory process.
Simple pericardial effusion: This tends to initially accumulate posteriorly in the oblique sinus. It is best seen in the PLAX view.
Loculated pericardial effusion: Are often seen after cardiac surgery, mediastinal radiation or in long-standing inflammatory conditions that allows fibrin strands and adhesions to deposit along the pericardial space. This may lead to a localized increase in intrapericardial pressure with the absence of traditional echocardiographic signs of respiratory variation and diastolic collapse because of the absence of free-flowing fluid.
Key Point:
Pericardial effusion and hematoma may be difficult to visualize immediately postcardiac surgery. Additional examination by transesophageal echocardiography should be considered if clinical suspicion for tamponade is high.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


