Pericardial Diseases
Pericardial disease is a small but important subset of cardiovascular illness. Clinical trial data and published society guidelines1 are sparse; board questions should focus on the most basic aspects of these diseases. We review the three most common presentations that are encountered by the cardiologist: acute pericarditis, pericardial effusions, and constrictive pericarditis.
Acute Pericarditis
Presentation and Diagnosis
Acute pericarditis is a common chest pain syndrome, occurring in up to 5% of cases presenting with non-myocardial infarction chest pain to an emergency setting.2 The diagnosis of acute pericarditis is made by a constellation of clinical symptoms, presence of a pericardial friction rub, characteristic ECG changes, and the presence of a pericardial effusion (Table 57.1). Elevation of inflammatory biomarkers serves as a supportive criterion for the diagnosis. Reasonable diagnostic certainty of acute pericarditis is present if findings in two of these four categories support the diagnosis. In practice, the transience of a pericardial friction rub makes it an unreliable marker of disease and significant weight is put on the rise of inflammatory markers during periods of symptom activity. The classic symptoms of acute pericarditis include the presence of sharp, pleuritic chest pain that is exacerbated by recumbency and improved by leaning forward. The pain often times radiates to one or both trapezius muscles. A pericardial friction rub is pathognomonic for pericarditis, but its inconsistency and transience make it less reliable as a diagnostic criterion. The electrocardiogram demonstrates a characteristic progression over time, with diffuse ST elevation and PR depression (representing epicardial injury of the ventricles and atria, respectively) early on (Fig. 57.1), followed by symmetric T-wave inversions, which eventually progress to normalization of the ST/T-wave segments. Serologic testing demonstrates elevation in the erythrocyte sedimentation rate (ESR) and/or C-reactive protein (CRP). Finally, echocardiographic demonstration of a pericardial effusion supports the presence of pericardial inflammation. The use of delayed enhancement imaging with gadolinium by cardiac magnetic resonance imaging is emerging as another imaging tool to demonstrate pericardial inflammation (Fig. 57.2).3
TABLE
57.1 Diagnostic Criteria for Acute Pericarditisa
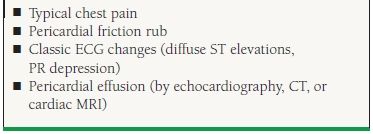
aRise in inflammatory markers, including ESR and CRP are supportive of the diagnosis. Two out of four major criteria are required for reasonable diagnostic certainty.
Adapted from Imazio M, et al. Controversial issues in the management of pericardial disease. Circulation. 2010;121:916–928.
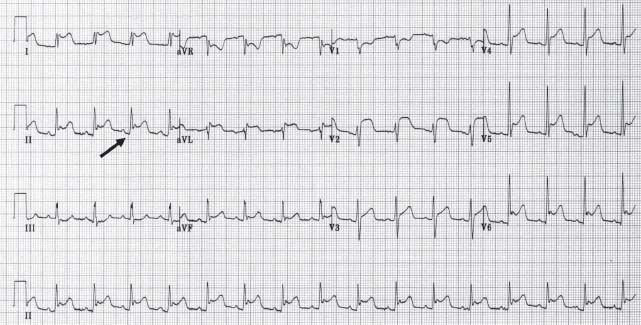
FIGURE 57.1 Classic ECG changes consistent with earliest stage of acute pericarditis. Diffuse ST-segment elevation with ST depression in aVR. Diffuse PR depression (blackarrow) with PR elevation in aVR.

FIGURE 57.2 Cardiac MRI. Delayed imaging following administration of gadolinium, short axis view. There is uptake of contrast in both the visceral (white arrow) and parietal layers (red arrow) of the pericardium, suggesting active inflammation of the pericardium.
Etiology
There is a long differential diagnosis for the etiology of acute pericarditis (Table 57.2).4 The frequency of etiology depends on the geographic population selected. In developed countries, idiopathic pericarditis represents the vast majority of cases. It is believed that most cases of idiopathic pericarditis represent the sequelae of a viral infection. An exhaustive virologic workup is rarely done in clinical practice, so the terms “idiopathic” and “viral” pericarditis are often used synonymously. Systemic autoimmune disease, chest radiation, open heart surgery, neoplastic disease, hypothyroidism, uremia, and acute myocardial infarction occur with enough frequency that they should be entertained in most cases. Tuberculous pericarditis is more common in developing countries and should be considered in patients with the appropriate exposure. Overall, the prognosis for idiopathic pericarditis is good. However, the risk of complications, including recurrence, tamponade, and constriction, is higher in patients with the following characteristics: female gender, large effusion or tamponade, and aspirin/nonsteroidal anti-inflammatory drug (NSAID) failure. Patients who have a specific underlying etiology (as opposed to idiopathic or viral pericarditis) are more likely to present with fevers, subacute onset, large pericardial effusion, elevation in cardiac troponin, and failure of NSAID treatment. These patients are also at increased risk for pericarditis-related complications of recurrence, tamponade, and constriction.5
TABLE
57.2 Etiology of 100 Consecutive, Hospitalized Acute Pericarditis Patients
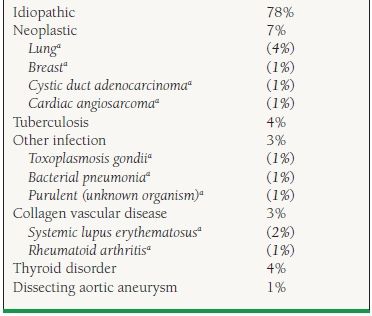
aDenotes specific etiologies under subcategory. Percentages in parentheses demonstrate how cases are divided within the subcategory. Adapted from Zaya R, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378–382.
Treatment
The mainstay of treatment for acute pericarditis is the use of nonsteroidal anti-inflammatory medications. The choice of drug is usually based on clinician experience and drug toxicity; there is a lack of head-to-head comparative trials that would demonstrate the superiority of one over the other. Typical regimens include aspirin (2,400 to 3,200 mg daily), indomethacin (150 mg/d), and ibuprofen (3,200 mg/d). Specific circumstances for choosing aspirin over other NSAIDs include acute pericarditis occurring in the postmyocardial infarction period, as well as chronic kidney disease.6,7 The optimal duration of treatment is unknown. One general approach is to maintain the maximum dose of NSAID until normalization of CRP or ESR (usually 1 to 2 weeks), followed by gradual tapering of the medication, usually over a period of 3 to 4 weeks.8,9 Treatment failure and recurrent symptoms are oftentimes related to inadequate dose and duration of NSAID treatment.
Colchicine has been demonstrated to be beneficial by randomized controlled trials in both first presentation and recurrent presentations of pericarditis.8–10 Patients taking colchicine (loading dose 1 to 2 mg on day 1, followed by maintenance dose 0.5 to 1 mg daily thereafter), demonstrate fewer recurrent episodes. The total duration of colchicine should be for at least 3 months, certainly well past the resolution of symptoms and elevation of inflammatory markers. In the special circumstance of acute pericarditis occurring in the postpericardiotomy setting, the COlchicine for the Prevention of the Postpericardiotomy Syndrome (COPPS) trial also demonstrates the efficacy and safety of colchicine in preventing pericarditis and its complications following open heart surgery.11
Corticosteroids are oftentimes used in acute pericarditis but their role is controversial. Observational data would suggest that they may actually increase the risk for recurrent pericarditis.8 Furthermore, the dosages used are controversial, as one retrospective study suggests that lower doses of corticosteroids may be as effective as higher doses (prednisone 0.2 to 0.5 mg/kg/d vs. 1 mg/kg/d), with lower occurrences of side effects.12 In our opinion, their use in patients with acute pericarditis, particularly those thought to be idiopathic or viral, should be restricted to cases with refractory symptoms (particularly when patients have been receiving optimal doses of NSAIDs and colchicine with evidence of ongoing inflammation) or to cases where they are used to treat a systemic autoimmune process. In the post–myocardial infarction setting, glucocorticoids should be avoided, as their use may be associated with the development of free wall rupture.
Recurrent Pericarditis
Recurrent pericarditis manifests in two different patterns, intermittent or incessant. In cases of intermittent pericarditis, patients will have symptom-free intervals of 6 weeks or greater while off all treatment. In contrast, incessant pericarditis is marked by return of symptoms within a 6 week period, either in the tapering or discontinuation phase of some or all anti-inflammatories.13 Incessant pericarditis is particularly common in patients treated with corticosteroids; observational studies would suggest that corticosteroids are a risk factor for this complication of acute pericarditis. Recurrence of symptoms often coincides with objective findings of pericardial inflammation, particularly elevations of CRP and/or ESR. However, in some cases, patients will demonstrate their stereotypic symptoms without objective findings of inflammation. The treatment approach for recurrent pericarditis is similar to acute pericarditis. Nonsteroidal anti-inflammatories should be the backbone of therapy, along with the use of colchicine. Treatment with maximum doses tolerated should be maintained for at least 1 to 2 weeks or until symptoms and inflammatory markers normalize. Tapering of NSAIDs should be performed over at least a 3 to 4 week period. For some patients with recalcitrant disease, the period of tapering may require several months. Colchicine has been demonstrated to decrease the recurrence rate in patients with recurrent pericarditis.10 Patients should take it for 3 months; for those who require longer periods for NSAID taper, colchicine is continued until NSAIDs have been successfully weaned. Corticosteroids should be reserved only for refractory cases; they may also be considered in patients who demonstrate highrisk features, including evidence for transient constrictive pericarditis on echocardiography or CMR. Weaning of corticosteroids can be problematic, as symptoms often recur when doses are being tapered. We recommend the use of concomitant NSAIDs and colchicine when attempting to wean corticosteroids (triple therapy). Minimizing time on glucocorticoids is an important goal. Even in the presence of recurrent symptoms, we recommend continuing to wean doses as long as objective markers of inflammation are controlled by other anti-inflammatory agents. The prognosis for recurrent, idiopathic pericarditis is good, with no reported cases of constrictive pericarditis and approximately 3.5% cases of tamponade (usually occurring during initial attack).
Pericardial Effusion
Pericardial effusions come to attention in a variety of ways: they are discovered incidentally or as part of an evaluation for pericarditis, or they present symptomatically with symptoms and signs of tamponade.
Presentation and Diagnosis
The classic symptoms of tamponade include hypotension and dyspnea; patients may present with lower extremity edema, if the effusion has had a very slow rate of growth. Physical signs include tachycardia, elevated jugular venous pressure, and the presence of an exaggerated pulsus paradoxus. Electrocardiographic manifestations of a pericardial effusion include low voltage and, in extreme cases, electrical alternans. Pericardial effusion can be detected by a variety of testing, including echocardiography, CT, and MRI. Echocardiography is generally the test of choice with its widespread availability and its ability to provide twodimensional (2-D) imaging with concomitant hemodynamic data. The diagnostic echocardiographic findings for tamponade include the presence of a pericardial effusion, evidence of ventricular interdependence (demonstrated by variation of mitral and tricuspid inflow velocities by pulsed-wave Doppler), inferior vena cava (IVC) plethora, and collapse of the right atrium (Fig. 57.3), left atrium, and/or right ventricle (RV) (Fig. 57.4). In clinical practice, the diagnosis of early tamponade is challenging and is made by an appraisal of the clinical scenario and available data. Unfortunately, no single clinical or echocardiographic sign is completely reliable and a summation of all accessible information is necessary. On rare occasions, the diagnosis of tamponade is in question and a Swan–Ganz catheter is used to adjudicate a diagnosis. Classic hemodynamic findings include tachycardia; elevated right atrial (RA) pressure; an “M” pattern in the RA waveform, with a preserved x descent and blunted y descent; equalization of diastolic pressures in the RA, RV, and pulmonary capillary wedge pressure (PCWP); and a low normal or depressed cardiac output/index. No single hemodynamic finding is pathognomonic or completely sensitive for tamponade either. In cases where a patient is symptomatic and has a moderate to large effusion by echocardiography, the demonstration of an elevated RA pressure and a low normal or depressed cardiac index should, without other explanation, be sufficient to make a diagnosis.14
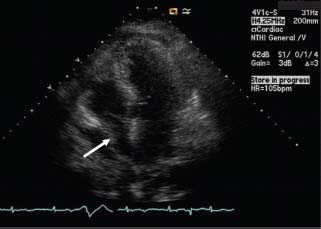
FIGURE 57.3 Transthoracic echocardiography, 4 chamber view. Collapse of the RA free wall (white arrow) during late atrial diastole.
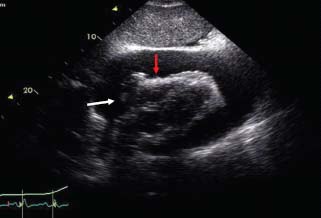
FIGURE 57.4 Transthoracic echocardiography, subcostal view. There is inversion of the RA (white arrow) and RV free wall (red arrow) during mid-diastole.
Etiology
The etiology of pericardial effusions includes the differential diagnosis of acute pericarditis; commonly encountered scenarios being idiopathic or viral pericarditis, malignancy, rheumatologic disease, tuberculosis, myocardial infarction, and post open heart surgery. Iatrogenic causes, including cardiac perforations from interventional and electrophysiology procedures, may manifest dramatically with tamponade from relatively small effusions accumulating within minutes. On occasion, effusion may be present as a result of elevated intracardiac filling pressures, such as in pulmonary hypertension or congestive heart failure. Finally, patients with myxedema or hypothyroidism may occasionally manifest with pericardial effusions. According to published series, compared to cases of acute pericarditis, patients with large pericardial effusions often have specific etiologies that are identifiable rather than the majority of cases being idiopathic (Table 57.3).15
TABLE
57.3 Differences in Etiologic Diagnosis of Large Pericardial Effusions in Two Major Series
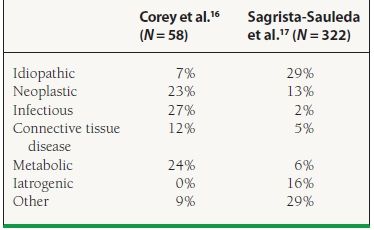
Adapted from Imazio M, et al. Medical therapy of pericardial disease Part II: noninfectious pericarditis, pericardial effusion and constrictive pericarditis. J Cardiovasc Med. 2010;11:785–794.



