Fig. 20.1
Chest radiographs and CT of a patient with partial pericardial defect. (a) Chest PA view. The heart is displaced into the left chest; the right border of the heart is projected over that of the spine. There is abnormal deep notching (arrow) at the aortopulmonary window. (b) ECG-gated cardiac CT shows interposed lung tissue (arrowhead) between the ascending aorta and the pulmonary trunk
20.2.2 Pericardial Effusion/Hemorrhage/Cardiac Tamponade
Originated from the obstruction of venous or lymphatic drainage.
Common causes of pericardial effusion include heart failure, renal insufficiency, infection (bacterial, viral, or tuberculosis), neoplasm (carcinoma of lung or breast or lymphoma), and injury (from trauma or myocardial infarction).
Echocardiography:
Considered the first-line test of pericardial effusion because of its high sensitivity, specificity, low cost, and lack of ionizing radiation.
Loculated effusion in an anterior location is difficult to detect.
Characterization of pericardial effusion composition by CT:
A fluid with attenuation similar to that of water is likely to be a simple effusion.
Pericardial effusion with attenuation greater than that of water suggests malignancy, hemopericardium, purulent exudate, or effusion associated with hypothyroidism.
Pericardial fluid with lower attenuation suggests the possibility of chylopericardium.
Cardiac tamponade:
A life-threatening condition due to external cardiac compression that resulted from accumulation of pericardial fluid, pus, blood, gas, or tissue within the pericardial cavity.
Predisposing factors: trauma, inflammation, scarring, or neoplastic involvement of the pericardial space.
Imaging findings:
Enlargement of the superior vena cava with a diameter similar to or greater than that of the adjacent thoracic aorta
Enlargement of the IVC with a diameter greater than twice that of the adjacent abdominal aorta
Periportal lymphedema:
Reflux of contrast material within the IVC or the azygos vein
Enlargement of hepatic and renal veins (Figs. 20.2, 20.3, and 20.4)
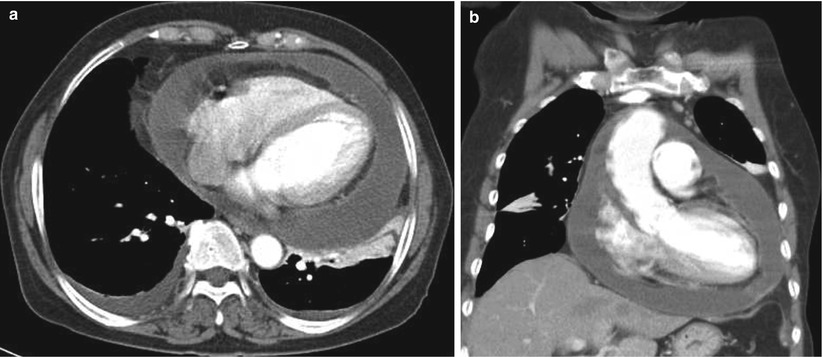
Fig. 20.2
Pericardial effusion. Axial (a) and coronal (b) CT images show large amount of pericardial effusion with a diffusely thickened pericardium. The attenuation of the pericardial effusion is grossly similar to that of pleural effusion
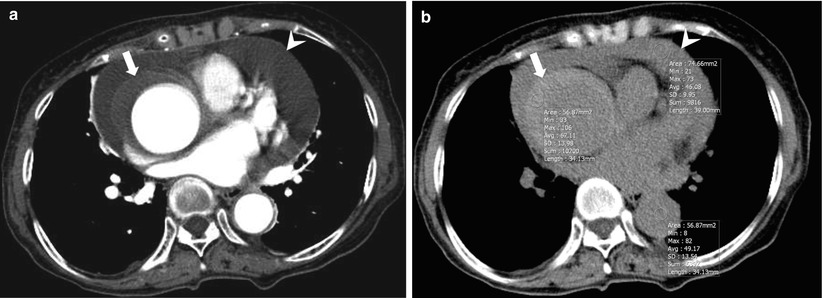
Fig. 20.3
Pericardial hemorrhage. (a) ECG-gated cardiac CT shows type A intramural hematoma (arrow) and small amount of pericardial effusion. (b) Precontrast CT shows high attenuating pericardial effusion suggesting hemorrhage (arrowhead). Note the high attenuation of the pericardial effusion (46 HU) which is similar to that of the lumen of the descending aorta (49 HU) and intramural hematoma (67 HU)
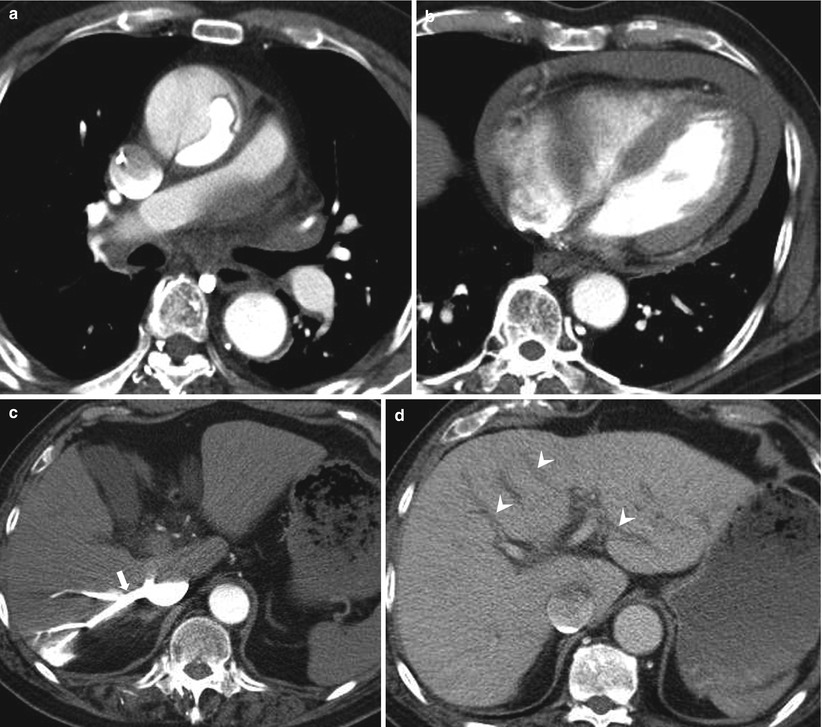
Fig. 20.4
Cardiac tamponade. (a) Cardiac CT angiography shows acute type A aortic dissection. (b) Axial CT image at the midportion of the left ventricle shows moderate amount of pericardial effusion and flattening of the anterior free wall of right ventricle. Arterial- (c) and delayed (d)-phase CT images at the liver level show contrast reflux (arrow) into the enlarged inferior vena cava and hepatic vein and periportal edema (arrowheads) which may be caused by increased right atrial pressure
20.2.3 Pericarditis
20.2.3.1 Acute Pericarditis
Acute inflammation of the pericardium with or without associated pericardial effusion.
Can occur as an isolated problem or as a manifestation of systemic disease.
Echocardiography:
Often recommended because it provides a rapid and accurate assessment of the pericardium and underlying cardiac function.
The presence of effusion helps to confirm the diagnosis.
Can diagnose or exclude the cardiac tamponade physiology when effusion is identified.
CT imaging:
Pericardial thickening is suggestive of acute pericarditis.
Pericardial irregularity may develop as the duration of inflammation increases.
In the case of pericardial effusion, initial characterization of fluid by attenuation.< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


