12 Pericardial Disease
Introduction
Background
• The human pericardium is a double-layered sac around the heart, covering most of the surface of the heart and extending on to the proximal portion of the great vessels.
• The inner serous layer of the pericardium is attached to the myocardium, forming the visceral pericardium or epicardium.
• It reflects at the level of the great vessels and turns into the parietal pericardium, which is a fibroserous layer.
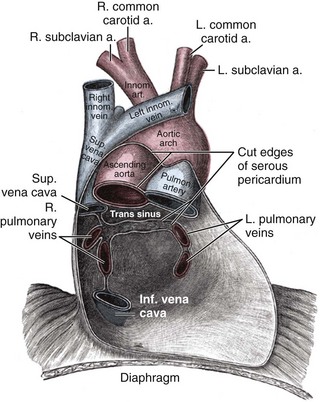
• Two sinuses are formed in the posterior pericardial cavity: The (upper) transverse sinus lies anterior to the superior vena cava and posterior to the pulmonary artery and ascending aorta. The (lower) oblique sinus lies posterior and inferior to the heart; the sinus is bounded by the reflection lines of both the left and the right pulmonary veins (Figure 12-1).
• Normal pericardial thickness is approximately 1 to 2 mm. Between the two layers, a small fluid collection of up to 30 mL is considered a normal finding. The pericardial fluid resembles an ultrafiltrate of plasma.
• The pericardium protects and restrains the heart as well as reduces friction. It isolates the heart from other structures in the mediastinum.
• A number of cardiac and systemic diseases involve the pericardial tissue, often with significant clinical consequences.
• Pericardial disease can impair cardiac chamber filling, especially on the thin-walled and low pressure right side of the heart, where constraint can decrease compliance.
• Usually, right ventricular (RV) compliance is greater than left ventricular (LV) compliance, and equalization can exaggerate the phenomenon of ventricular interdependence.
• Intrapericardial pressure is generally similar to intrapleural pressure, varying from approximately −6 mm Hg during inspiration to approximately −3 mm Hg at the end of expiration.
• When intrapericardial pressure drops during inspiration, RV filling and tricuspid inflow are enhanced.
• At the same time, the interventricular septum shifts to the left side of the heart, decreasing LV filling and transmitral flow; the opposite relationship is true for spontaneous exhalation.
Overview of Echocardiographic Approach
• Echocardiography is the most sensitive and specific method for evaluation of pericardial effusion (PE).
• Diagnostic echocardiography of the pericardium involves multiple views to fully understand the degree and localization of pericardial disease.
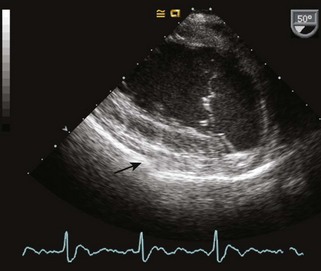
• Two-dimensional (2D) echocardiography is used for anatomic imaging of the pericardium and pericardial space (Figure 12-2).
• Transthoracic echocardiography (TTE) is the primary method in suspected pericardial disease, although in some cases, transesophageal views provide better images. The midesophageal (ME) four-chamber view, the ME RV inflow-outflow view, and the transgastric (TG) midpapillary short axis view are useful for anatomic imaging.
• M-mode echocardiography can be helpful for the diagnosis of PEs and interrogation of septal motion.
• Spectral Doppler echocardiography is used to interrogate cardiac chamber filling, hepatic and pulmonary vein flows, and overall diastolic function.
• Measurement of inferior vena cava (IVC) size and respiratory variation can be used to reconfirm pericardial disease in the setting of elevated RV filling pressures.
Pericardial Effusion
Background
• A wide variety of diseases can cause PEs, but most commonly, this is seen after cardiac surgery, in congestive heart failure, acute type A aortic dissections, and end-stage renal disease (Table 12-1).
• PEs become a clinical syndrome as soon as the fluid accumulation causes an increase in intrapericardial pressure and the patient develops symptoms.
• The rate of how fast fluid accumulates in the pericardial space is important. An effusion that is caused by a slow increase in pericardial fluid can become quite large before clinical symptoms occur. Conversely, relatively small fluid collections can cause cardiac tamponade when developing rapidly.
• When the patient is in a supine position, PEs are initially located posterior to the heart. As more pericardial fluid accumulates, the effusion is surrounding the heart and can cause cardiac tamponade (see “Cardiac Tamponade”). Loculated effusions are also possible, especially after cardiac surgery.
TABLE 12-1 OVERVIEW OF PERICARDIAL DISEASE ETIOLOGIES AND ASSOCIATED SYNDROMES
| Etiology | Clinical Endpoints |
|---|---|
| Idiopathic | |
| Infectious | |
| Bacterial | Acute pericarditis |
| Tuberculous | Acute pericarditis, constrictive pericarditis |
| Viral | Acute pericarditis |
| Parasitic | Acute pericarditis |
| Connective tissue disease | |
| Systemic lupus erythematosus | Pericarditis, pericardial effusion |
| Scleroderma | Pericarditis |
| Rheumatoid arthritis | Pericarditis, pericardial effusion |
| Wegener’s granulomatosis | Pericarditis, pericardial effusion |
| Post-myocardial infarction | |
| Dressler’s syndrome | Acute pericarditis, pericardial effusion |
| Ventricular rupture | Pericardial effusion, cardiac tamponade |
| Metabolic | |
| Uremia | Pericardial effusion |
| Myxedema | Pericardial effusion |
| Trauma | Pericardial effusion, cardiac tamponade |
| Postradiation | Acute pericarditis, constrictive pericarditis |
| Postoperatively after cardiac surgery | Pericardial effusion, cardiac tamponade, constrictive pericarditis |
| Neoplastic | |
| Primary pericardial and cardiac tumors | Pericardial effusion, cardiac tamponade |
| Metastatic disease | Pericardial effusion, cardiac tamponade |
| Congestive heart failure | Pericardial effusion |
| Aortic dissection, left ventricular rupture | Pericardial effusion, cardiac tamponade |
| Postoperatively after cardiac catheter or electrophysiologic procedures | Pericardial effusion, cardiac tamponade |
Overview of Echocardiographic Approach
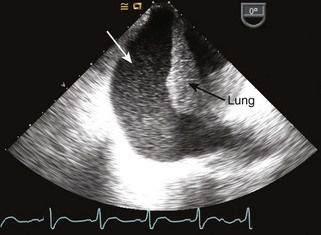
• On 2D images, a PE will appear as an echo-free space between both pericardial layers (Figure 12-3). This is the most useful imaging modality for the diagnosis of effusions.
• Transesophageal echocardiography (TEE) is especially useful for detection of posterior effusions and in the postoperative setting where retrosternal hematoma can impair transthoracic image quality.
• M-mode echocardiography can be useful as an additional tool for the detection of smaller effusions.
• In large PEs, spectral Doppler echocardiography should be considered to assess for markers of possible cardiac tamponade (see “Cardiac Tamponade”).
Anatomic Imaging
Step 1: 2D Image Acquisition
• 2D echocardiography will show an echo-free space between the visceral and the parietal pericardium.
• M-mode echocardiography images are best acquired using the parasternal long axis view in TTE imaging and the TG mid short axis view in TEE.
• In some instances, saline contrast can help to discriminate the pericardial space from the heart itself.
TABLE 12-2 TRANSTHORACIC VERSUS TRANSESOPHAGEAL ECHOCARDIOGRAPHY VIEWS FOR THE IMAGING OF PERICARDIAL EFFUSIONS
| TTE | TEE | |
|---|---|---|
| Useful echocardiographic views | Parasternal long axis | ME four-chamber |
| Parasternal short axis | ME RV inflow-outflow | |
| Apical four-chamber subcostal | Transgastric mid short axis | |
| Benefits and limits | Less invasive technique | Better detection of posterior effusion |
| Poor image quality after cardiac surgery | More invasive |
ME, midesophageal; RV, right ventricular; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography.
Step 2: Image Analysis
• Although grading scales are neither standardized nor validated, there is obvious correlation between the measured distance and the pericardial fluid volume. This has to be put into the perspective of the patient’s clinical presentation.
TABLE 12-3 ECHOCARDIOGRAPHIC GRADING OF PERICARDIAL EFFUSIONS
| Location of the Effusion | Distance between Pericardial Layers | |
|---|---|---|
| Small | Posterior only | <0.5 cm |
| Moderate | Anterior and posterior | 0.5-2 cm |
| Large | Anterior and posterior | >2 cm |
Pitfalls
• Surrounding PEs are hard to miss, and generally easy to diagnose, but localized PEs can be more difficult to identify and also have a more complex differential diagnosis, such as intrapericardial hematoma or pericardial mass.
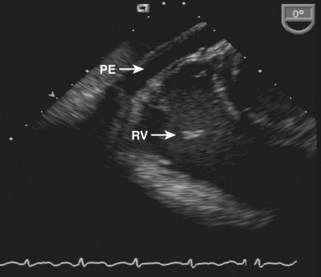
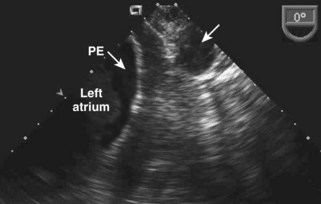
• Not only large circumferential effusions can cause the clinical picture of cardiac tamponade. In some cases, localized PEs can cause a tamponade-like picture, although not compressing all of the cardiac chambers (Figure 12-4).
Pericardial versus Pleural Effusion
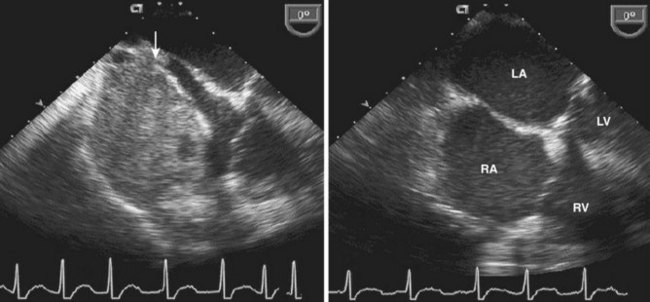
• Not every echo-free space around the heart is a PE. Differential diagnoses include pleural effusions, and a dilated descending thoracic aorta. On occasion a massively dilated left atrium (LA) may be mistaken for a pericardial effusion.
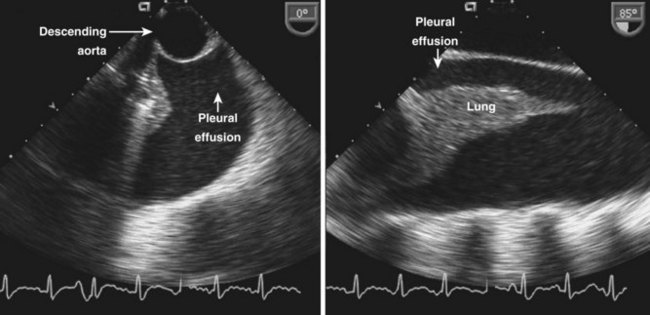
• Left-sided pleural effusions are visualized as echo-free spaces posterolateral to the descending thoracic aorta on the left (Figure 12-5). The partially collapsed lung is often visualized.
• In contrast, PEs are generally found between the descending thoracic aorta and the LA (Figure 12-6A). On occasion, an effusion may be first appreciated surrounding the left atrial appendage (LAA; see Figure 12-6B).
• Right-sided pleural effusions appear as echo-free spaces adjacent to the right atrium (RA). As opposed to PEs, right-sided pleural effusions are bounded inferiorly to the convex-shaped dome of the diaphragm adjacent to the liver. Similarly to the left side, the partially collapsed lung is often visualized (Figure 12-7).
Cardiac Tamponade
Background
• Whenever there is a rapid or massive collection of pericardial fluid, the pressure inside the pericardium increases and will eventually overcome the intracardiac pressure, leading to impaired cardiac chamber filling.
• Thin-walled chambers on the right side of the heart are usually affected first, unless there is loculated pericardial hematoma adjacent to the left heart causing localized compression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree