Indication
Class
Symptomatic patients with favorable characteristicsa for PTMC
I
Symptomatic patients with contraindication or high risk for surgery
I
As initial treatment in symptomatic patients with unfavorable anatomy but without unfavorable clinical characteristicsa
IIa
Asymptomatic patients without unfavorable characteristicsa and high thromboembolic risk
IIa
Previous history of embolism
Dense spontaneous contrast in the left atrium
Recent or paroxysmal atrial fibrillation
Asymptomatic patients without unfavorable characteristicsa and high risk of hemodynamic decompensation
IIa
Systolic pulmonary pressure > 50 mmHg at rest
Need for major noncardiac surgery
Desire of pregnancy
20.4 Pre-procedural Evaluation
Transthoracic echocardiography (TTE) is the most useful imaging tool for obtaining comprehensive information about the MV. The severity and extent of fusion, thickening, shortening, calcification, thrombus, and mitral regurgitation are all meticulously studied. A semiquantitative score of the MV pathology has been used to predict the efficacy of PTMC and select the appropriate patient (Table 20.2). A score of less than 9 with not more than mild MR is considered most suitable for PTMC [2]. With a higher MV morphology score and/or moderate degree of MR, one should balance the risk of PTMC and surgical open mitral commissurotomy (OMC). PTMC is an option if the patient is a high-risk candidate for OMC. The MV morphology score however does not quantify commissural fusion or calcification. As splitting of the fused commissure is essential for relief of MS, commissural fusion and calcification must be studied in detail.
Table 20.2
Mitral valve morphology score by echocardiography
Grade | Mobility | Subvalvular thickening | Leaflet thickening | Calcification |
|---|---|---|---|---|
1 | Highly mobile valve with only leaflet tips restricted | Minimal thickening just below the mitral leaflets | Leaflets near normal in thickness (4–5 mm) | A single area of increased echo brightness |
2 | Leaflet mid- and base portions have normal mobility | Thickening of chordal structures extending to one-third of the chordal length | Mid-leaflets normal, considerable thickening of margins (5–8 mm) | Scattered areas of brightness confined to leaflet margins |
3 | Valve continues to move forward in diastole, mainly from the base | Thickening extended to distal third of the chords | Thickening extending through entire leaflet (5–8 mm) | Brightness extending into midportions of the leaflets |
4 | No or minimal forward movement of the leaflets in diastole | Extensive thickening and shortening of all chordal structures extending down to the papillary muscles | Considerable thickening of all leaflet tissue (>8–10 mm) | Extensive brightness throughout much of leaflet tissue |
Transesophageal echocardiography (TEE) is necessary to exclude thrombus in the LA, especially in the appendage. It is desirable in all patients before PTMC and mandatory in patients with atrial fibrillation or previous embolism and in patients with suboptimal TTE images.
20.5 Balloon Catheters for PTMC
Inoue’s method using an inflatable nylon-latex balloon catheter (NLBC) is the most widely used technique and is described in detail below. Two types of NLBC are currently available: Inoue balloon catheter (Toray, Tokyo, Japan) and Accura balloon catheter (Vascular Concepts Limited, Hallstead, United Kingdom). The NLBC is designed to expand initially in its distal portion and then sequentially in its waist and proximal part. The low compliance in its waist allows the balloon to take a dumbbell shape centered in the narrowest part of the mitral valve and expand to the desired diameter (Fig. 20.1). The differences between Inoue and Accura balloon catheters are shown in Table 20.3.
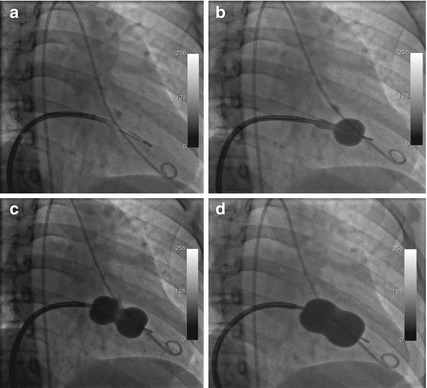
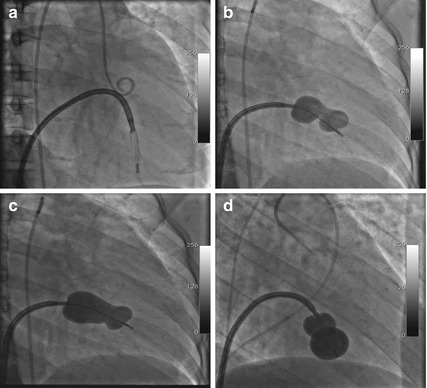




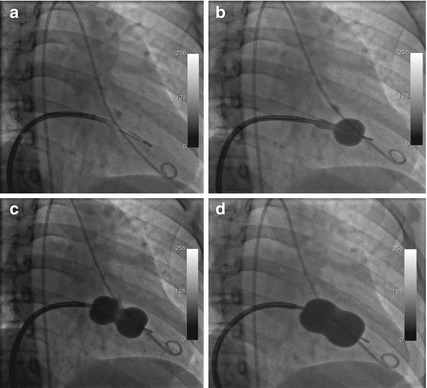
Fig. 20.1
Fluoroscopy in right anterior oblique view: (a) ideal position of the balloon catheter on entry pointing toward the LV apex; (b) and (c) inflation of the distal balloon followed by positioning across the mitral valve and inflation of the proximal balloon; (d) full inflation and dilatation of the valve orifice to the desired diameter
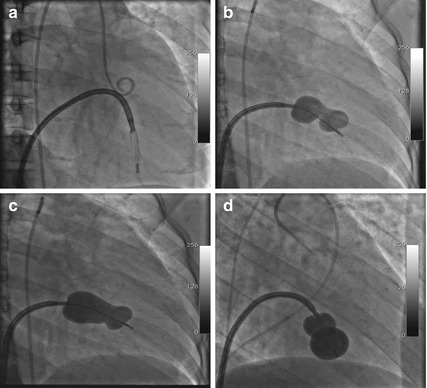
Fig. 20.2
Fluoroscopy in right anterior oblique view: (a) improper position of the balloon catheter pointing inferiorly and posteriorly into the chordae; (b) and (c) distortion of the distal and proximal parts of the balloon by subvalvular apparatus; (d) both distal and proximal parts of the balloon inflated in the LV below the valve orifice. These clues indicate entrapment of the balloon catheter
Table 20.3
Differences between Accura and Inoue balloon catheters
Feature | Inoue catheter | Accura catheter |
|---|---|---|
Construction | Triple lumen | Double lumen |
Shaft size | 12 French | 11 French |
Contrast dilution recommended | 1:4 | 1.6–1.8 |
Blood seepage between layers | Possible | No |
Prevention of deflation failure | Yes | No |
Vent holes | Yes (n = 2) | No |
Vent tube | Yes | No |
Balloon size achievable | + 4 mm (22–26 mm) | + 3 mm (23–26 mm) |
Cost | More | Less |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


