Percutaneous interventions for valvular heart disease are rapidly gaining momentum. Transcatheter aortic valve implantation for aortic stenosis in patients with high surgical risk and percutaneous mitral valve repair with the MitraClip have been shown to be noninferior to surgery. Little is known about the combination of these interventions in patients with mixed valvular disease. The investigators present 2 patients, both with acute device successes but contrasting outcomes, and attempt to glean some insights from these patients.
Percutaneous treatment of degenerative aortic stenosis (AS) has recently gained momentum, with the results of the first randomized study showing a clear mortality advantage of transcatheter aortic valve implantation (TAVI) over conservative treatment in a high-risk cohort of patients with AS. Nevertheless, questions remain with regard to this promising treatment, including optimal patient selection. One instance in which the benefits of TAVI may be doubtful is in patients with mixed valvular disease, in particular concomitant moderate to severe mitral regurgitation (MR). However, with the advent of various percutaneous mitral valve therapies, in particular the mitral edge-to-edge leaflet repair or the MitraClip (Abbott Vascular, Redwood City, California), the option of fully percutaneous treatment appears to be feasible for such patients. The experience is nevertheless limited and the paradigm likely different from surgical interventions. Hence, we present the first 2 such patients with double-valve disease treated fully percutaneously but with starkly contrasting outcomes.
Case Descriptions
Case 1
A 72-year-old woman presented with New York Heart Association class III to IV heart failure. Echocardiography revealed significant mixed valvular disease with severe degenerative AS, moderate to severe degenerative MR due to annular calcium, and moderate functional tricuspid regurgitation. Her left ventricular ejection fraction (LVEF) was 45%. In view of a high surgical risk due to previous coronary bypass surgery, frailty, and a high logistic European System for Cardiac Operative Risk Evaluation score of 51%, she initially underwent successful transfemoral TAVI with a CoreValve self-expanding bioprosthesis (Medtronic, Inc., Minneapolis, Minnesota), 1 of the 2 available TAVI devices. Of note, all her bypass grafts were patent.
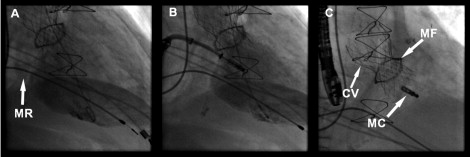
However, the patient was readmitted 2 months later for heart failure, which appeared to be due to MR that had not improved after TAVI. The CoreValve showed excellent function on echocardiography, with a negligible transaortic valve gradient and trivial aortic regurgitation (AR). Percutaneous mitral valve repair was subsequently performed successfully with the MitraClip. Her MR was reduced from 3+ to 1+ ( Figure 1 ), with a moderate reduction in tricuspid regurgitation as well. She reported marked functional improvement (New York Heart Association class II) and remains well >3 months after the procedure.
Case 2
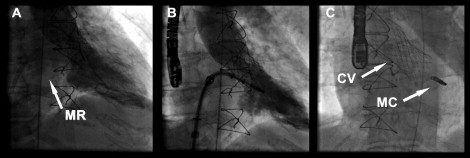
An 84-year-old man presented with a non–ST-segment elevation acute coronary syndrome. Eight years previously, he had undergone coronary bypass grafting and aortic valve replacement with a 23-mm MitroFlow bioprosthesis (Sorin Group, Milan, Italy). He had a history of previous stroke, chronic obstructive lung disease, hypertension, hyperlipidemia, and chronic renal insufficiency. Coronary angiography showed severe native 3-vessel disease. All bypass grafts were patent except an occluded venous bypass to the right coronary artery with low feasibility for percutaneous revascularization. Transesophageal and transthoracic echocardiography revealed moderate valvular and paravalvular AR in a degenerated bioprosthesis as well as moderate to severe MR, the latter likely from a combination of degenerative and ischemic causes. There was moderate calcification of the mitral apparatus and tethering of the P2 segment of the mitral valve. His LVEF was reduced at 37%, with hypokinesia in the inferior wall, but his left ventricular dimensions were normal at this point. During this admission, he was also found to have intermittent Mobitz type 2 atrioventricular block, and a single-chamber pacemaker was implanted. As for the acute coronary syndrome, he was treated medically. Two months later, he returned with decompensated heart failure. Investigations now revealed worsening AR, from 2+ to 3+. In view of his high surgical risk and a logistic European System for Cardiac Operative Risk Evaluation score of 65%, the patient underwent successful transfemoral TAVI with a 26-mm CoreValve prosthesis, albeit for an off-label indication. Unfortunately, he was readmitted again 2 months later with heart failure. His CoreValve was functioning well, with minimal AR. His LVEF remained 36%, but the left ventricle was now dilatated. MR remained moderate to severe. Medical treatment was intensified, but he returned again 4 months later with another decompensation. MitraClip implantation was then performed, with good acute results and reduction of MR to <2+ ( Figure 2 ). Postprocedurally, however, the patient developed worsening heart failure intractable to medical therapy. Repeat echocardiography showed subjective worsening of his LVEF despite only mild residual MR. The risk for surgical intervention was too high. He finally succumbed to heart failure and died 3 weeks after the procedure.