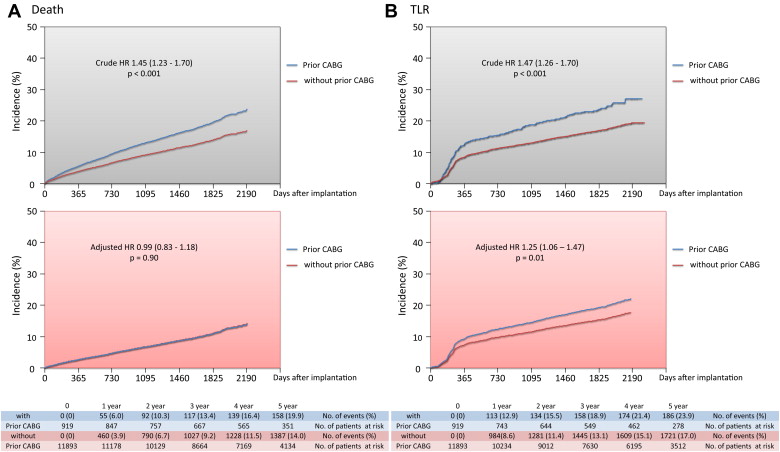
A paucity of data is available from large-scale studies evaluating the long-term outcomes of percutaneous coronary intervention in patients who had previously undergone coronary artery bypass grafting (CABG) in the drug-eluting stent era. Of 12,812 patients who had undergone sirolimus-eluting stent implantation in the j-Cypher registry, 919 (7.2%) had a history of CABG and had significantly higher crude 5-year mortality (19.9% vs 14.0%, p <0.001). After adjusting for confounders, the excess risk of death was no longer significant (hazard ratio 0.99, 95% confidence interval 0.83 to 1.18, p = 0.90), and the adjusted risk of target lesion revascularization was significantly higher in patients with previous CABG than in those without (hazard ratio 1.25, 95% confidence interval 1.06 to 1.47, p = 0.01). Of the patients with previous CABG, those who had undergone ≥1 saphenous vein graft intervention had significantly higher adjusted risks of cardiac death (hazard ratio 2.21, 95% confidence interval 1.26 to 3.76, p = 0.01), myocardial infarction (hazard ratio 2.56, 95% confidence interval 1.10 to 5.60, p = 0.03), target lesion revascularization (hazard ratio 2.65, 95% confidence interval 1.82 to 3.81, p <0.001), and definite stent thrombosis (hazard ratio 7.70, 95% confidence interval 1.99 to 29.1, p = 0.004) compared with those who underwent percutaneous coronary intervention only for the native coronary artery. In conclusion, the adjusted mortality was similar between patients with and without previous CABG, despite a significantly different risk of target lesion revascularization. Among the patients with previous CABG, those with saphenous vein graft intervention using a first-generation drug-eluting stent had worse clinical outcomes than those with a native coronary artery target only.
Although the use of drug-eluting stents (DESs) has reduced the incidence of repeat revascularization, coronary artery bypass grafting (CABG) remains the standard of care for patients with severe coronary artery disease. However, almost 40% of patients with previous CABG required either percutaneous coronary intervention (PCI) or redo CABG during 20 years of follow-up, and the proportion of patients with previous CABG in the total PCI population was as great as 17.5%. Acute coronary syndrome after CABG has been reported to be associated with worse clinical outcomes than acute coronary syndrome in patients without previous CABG. Furthermore, PCI for saphenous vein grafts (SVGs) remains challenging even after the introduction of DESs. Despite an increasing number of patients with previous CABG undergoing PCI, a paucity of data is available from large-scale studies evaluating the long-term outcomes of PCI in patients with previous CABG in the DES era. Therefore, we conducted a post hoc subgroup analysis using the 5-year follow-up data from the j-Cypher Registry to evaluate the long-term outcomes of patients with previous CABG who had undergone PCI compared with those of patients without previous CABG.
Methods
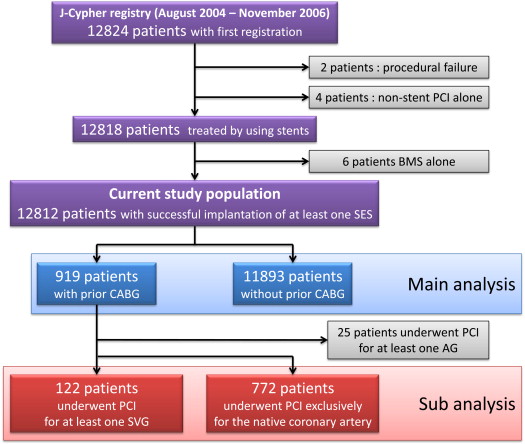
The design, patient enrollment, and long-term follow-up results of the j-Cypher Registry have been previously published. In brief, the multicenter observational registry included 12,824 consecutive patients (19,675 lesions) who had undergone an attempt of ≥1 sirolimus-eluting stent implantation from August 2004 to November 2006. Of those patients, 12 were excluded; 2 with procedural failure, 4 without stent use, and 6 with bare metal stent use only. The study population included the remaining 12,812 patients with successful implantation of ≥1 sirolimus-eluting stent (19,662 lesions). The baseline characteristics and clinical outcomes were compared on a patient basis between those with and without previous CABG. A subgroup analysis of patients with previous CABG was also conducted, comparing those patients who had undergone PCI for ≥1 SVG with those who had undergone PCI only for the native coronary artery.
Death was regarded as cardiac in origin unless obvious noncardiac causes could be identified. Any death during the index hospitalization was regarded as cardiac in origin. Sudden death was defined as unexplained death in previously stable patients. Myocardial infarction was adjudicated according to the definition in the Arterial Revascularization Therapy Study. Stroke during follow-up was defined as ischemic or hemorrhagic stroke requiring hospitalization with symptoms lasting 24 hours. Target lesion revascularization (TLR) was defined as either PCI or CABG resulting from restenosis or thrombosis of the target lesion that included the proximal and distal edge segments and the ostium of the side branches. Definite stent thrombosis was defined according to the Academic Research Consortium definition.
The relevant review boards of all 37 participating centers approved the study protocol, and all patients provided written informed consent.
Categorical variables and ordinal variables are expressed as numbers and percentages. Frequency analysis was performed using the chi-square test. Continuous variables are expressed as the mean ± SD and/or range or median and range and/or interquartile range and were compared using the unpaired t test or the Wilcoxon rank sum test, depending on their distributions. The cumulative incidence was calculated using the Kaplan-Meier method and compared using the log-rank test. Because late events are common after sirolimus-eluting stenting, landmark analyses at 1 year were performed to evaluate the difference in TLR and stent thrombosis outcomes after 1 year. The patients who survived free of either TLR or stent thrombosis at 1 year were included for additional survival analysis. Consistent with our previous report, the multivariate Cox proportional hazard model was used, adjusting for all baseline patient characteristics listed in Table 1 . The hazard ratios and 95% confidence intervals were computed. Univariate and multivariate correlates for individual end points can be found in the online supplement ( Supplementary Tables 1 and 2 ).
| Variable | Previous CABG | p Value | ||||
|---|---|---|---|---|---|---|
| Yes (n = 919) | No (n = 11,893) | |||||
| Native Coronary Artery Target Only (n = 772) | ≥1 SVG Target (n = 122) | p Value (Native vs SVG) | Total | |||
| Age (yrs) | 69.2 ± 9.2 | 70.7 ± 7.7 | 0.09 | 69.4 ± 9.0 | 68.3 ± 10.4 | 0.002 |
| Age ≥80 yrs ∗ | 96 (12) | 15 (12) | 0.97 | 113 (12) | 1,551 (13) | 0.52 |
| Men ∗ | 612 (79) | 96 (79) | 0.88 | 729 (79) | 8,914 (75) | 0.003 |
| BMI (kg/m 2 ) | 23.7 ± 3.4 | 23.5 ± 3.1 | 0.59 | 23.7 ± 3.4 | 24.0 ± 3.4 | 0.008 |
| BMI <25.0 kg/m 2 ∗ | 513 (67) | 85 (70) | 0.48 | 616 (67) | 7,716 (65) | 0.19 |
| Hypertension ∗ | 581 (75) | 97 (80) | 0.31 | 696 (76) | 8,854 (75) | 0.39 |
| DM ∗ | 376 (49) | 66 (54) | 0.27 | 452 (49) | 4,860 (41) | <0.001 |
| Insulin-treated DM | 118 (15) | 21 (17) | 0.59 | 141 (15) | 1,062 (8.9) | <0.001 |
| Current smoker ∗ | 77 (10) | 10 (8) | 0.54 | 87 (9.5) | 2,517 (21) | <0.001 |
| eGFR <30 ml/min/1.73 m 2 | ||||||
| Without hemodialysis ∗ | 50 (6.5) | 12 (10) | 0.17 | 62 (6.8) | 566 (4.8) | 0.007 |
| With hemodialysis ∗ | 72 (9.3) | 9 (7) | 0.49 | 84 (9.1) | 596 (5.0) | <0.001 |
| Acute coronary syndrome ∗ | 118 (15) | 32 (26) | 0.003 | 154 (17) | 3,024 (25) | <0.001 |
| STEMI | 8 (1.0) | 5 (4) | 15 (1.6) | 1,238 (10) | ||
| Non–STEMI | 9 (1.2) | 3 (3) | 13 (1.4) | 293 (2.5) | ||
| Unstable angina pectoris | 101 (13) | 24 (20) | 126 (14) | 1,493 (13) | ||
| Emergent procedure | 56 (7.3) | 19 (16) | 0.002 | 77 (8.4) | 1,848 (16) | <0.001 |
| Presence of shock | 6 (0.8) | 2 (2) | 0.35 | 8 (0.9) | 165 (1.4) | 0.17 |
| Previous myocardial infarction ∗ | 300 (39) | 55 (45) | 0.19 | 367 (40) | 3,117 (26) | <0.001 |
| Previous stroke ∗ | 91 (12) | 15 (12) | 0.87 | 109 (12) | 1,109 (9.3) | 0.01 |
| Peripheral vascular disease ∗ | 151 (20) | 30 (25) | 0.20 | 184 (20) | 1,339 (11) | <0.001 |
| Previous heart failure ∗ | 167 (22) | 28 (23) | 0.74 | 201 (22) | 1,590 (13) | <0.001 |
| Previous PCI ∗ | 470 (61) | 83 (68) | 0.13 | 564 (61) | 5,381 (45) | <0.001 |
| Multivessel coronary disease ∗ | 771 (99.9) | 122 (100) | 0.69 | 918 (100) | 6,131 (52) | <0.001 |
| Target of proximal LAD ∗ | 148 (19) | 6 (5) | <0.001 | 154 (17) | 6,436 (54) | <0.001 |
| Target of unprotected LMCA ∗ | 44 (5.7%) | 1 (1) | 0.02 | 46 (5.0) | 536 (4.5) | 0.48 |
| Target of in-stent restenosis ∗ | 125 (16) | 25 (21) | 0.24 | 153 (17) | 1,794 (15) | 0.20 |
| Target of chronic total occlusion ∗ | 117 (15) | 11 (9) | 0.07 | 130 (14) | 1,460 (12) | 0.10 |
| Side branch stenting ∗ | 33 (4.3) | 1 (1) | 0.06 | 34 (3.7) | 696 (5.9) | 0.007 |
| EF (%) | 53.3 ± 13.7 | 51.7 ± 15.0 | 0.28 | 53.0 ± 14.0 | 58.2 ± 13.3 | <0.001 |
| EF ≤40% | 135 (18) | 25 (21) | 0.42 | 166 (18) | 1,090 (11) | <0.001 |
| Vessels treated per patient (n) | 1.24 ± 0.48 | 1.29 ± 0.45 | 0.36 | 1.26 ± 0.49 | 1.33 ± 0.56 | <0.001 |
| Multivessel stenting | 172 (22) | 35 (29) | 0.12 | 214 (23) | 3,354 (28) | 0.001 |
| Lesions treated per patient (n) | 1.49 ± 0.70 | 1.52 ± 0.79 | 0.58 | 1.49 ± 0.72 | 1.54 ± 0.81 | 0.04 |
| Reference diameter preoperatively <2.5 mm ∗ | 262 (35) | 22 (19) | <0.001 | 295 (33) | 4,323 (37) | 0.01 |
| Stents per patient (n) | 1.98 ± 1.23 | 1.76 ± 1.19 | 0.07 | 1.94 ± 1.22 | 2.00 ± 1.29 | 0.20 |
| Total stent length per patient (mm) | 42.8 ± 28.5 | 37.8 ± 28.1 | 0.07 | 42.0 ± 28.5 | 42.5 ± 28.3 | 0.55 |
| Total stent length >28 mm ∗ | 439 (57) | 53 (43) | 0.006 | 501 (55) | 6,602 (56) | 0.56 |
| Intravascular ultrasound ∗ | 338 (44) | 44 (36) | 0.12 | 392 (43) | 5,671 (48) | 0.003 |
∗ Used for multivariate analyses adjusting for baseline characteristics.
All statistical analyses were performed using JMP, version 9.03 (SAS Institute, Cary, North Carolina) and Statistical Package for Social Sciences, version 17.0 (SPSS, Chicago, Illinois). All reported p values were 2-sided, and p values <0.05 were regarded as statistically significant.
Results
Of the 12,812 patients with successful implantation of ≥1 sirolimus-eluting stent (19,662 lesions), 919 patients (7.2%) with 1,369 lesions had a history of CABG ( Figure 1 ). The most recent date of CABG was available for 815 patients (88.7%). The interval from the most recent CABG and the index PCI included was within 30 days for 41 patients (5.0%), 31 to 365 days for 119 patients (14.6%), and >365 days for 655 patients (80.4%; median 1,895 days, interquartile range 548 to 4,023). The baseline patient characteristics were significantly different between the patients with and without previous CABG ( Table 1 ). Patients with previous CABG were older and had a greater prevalence of co-morbidities, including diabetes mellitus, impaired renal function with or without maintenance hemodialysis, and reduced left ventricular function. However, the prevalence of current smokers and an acute coronary syndrome presentation were lower in patients with previous CABG than in those without previous CABG. Furthermore, patients with previous CABG more often had a history of myocardial infarction, stroke, heart failure, and PCI. Regarding the lesion characteristics, the patients with previous CABG included those with significantly more complex lesion characteristics, such as in-stent restenosis, chronic total occlusion, severe calcification, and small reference vessel diameter. In contrast, a culprit lesion for ST-segment elevation myocardial infarction was less prevalent in patients with previous CABG ( Table 2 ).
| Variable | Previous CABG | p Value | ||||
|---|---|---|---|---|---|---|
| Yes (n = 919, 1,369 Lesions) | No (n = 11,893, 18,293 Lesions) | |||||
| Native Coronary Artery Target Only (n = 772, 1,147 Lesions) | ≥1 SVG Target (n = 122, 186 Lesions) | p Value (Native vs SVG) | Total | |||
| Lesion characteristics | ||||||
| Lesion location | <0.001 | <0.001 | ||||
| Native | 1,147 (100) | 44 (24) | 1,200 (88) | 18,293 (100) | ||
| LAD | 193 (17) | 8 (4) | 201 (15) | 7,639 (42) | ||
| LCx artery | 331 (29) | 12 (7) | 345 (25) | 3,999 (22) | ||
| RCA | 482 (42) | 21 (11) | 508 (37) | 6,115 (33) | ||
| LMCA | 141 (12) | 3 (2) | 146 (11) | 540 (3.0) | ||
| SVG | 0 (0.0) | 142 (76) | 144 (11) | 0 (0.0) | ||
| AG | 0 (0.0) | 0 (0) | 25 (1.8) | 0 (0.0) | ||
| Culprit lesion for STEMI | 8 (0.7) | 6 (3) | 0.002 | 16 (1.2) | 1,305 (7.1) | <0.001 |
| In-stent restenosis | 147 (13) | 25 (13) | 0.82 | 175 (13) | 2,021 (11) | 0.048 |
| Chronic total occlusion | 140 (12) | 11 (6) | 0.01 | 153 (11) | 1,641 (9.0) | 0.006 |
| Severe calcium | 198 (17) | 7 (4) | <0.001 | 206 (15) | 1,580 (8.6) | <0.001 |
| Bifurcation | 235 (21) | 9 (5) | <0.001 | 248 (18) | 3,467 (19) | 0.44 |
| Side branch stenting | 36 (3.1) | 1 (1) | 0.045 | 37 (2.7) | 720 (3.9) | 0.02 |
| Lesion length ≥30 mm | 194 (17) | 18 (10) | 0.01 | 218 (16) | 2,614 (15) | 0.09 |
| Reference vessel diameter preoperatively <2.5 mm | 318 (28) | 26 (14) | <0.001 | 356 (27) | 5,388 (30) | 0.009 |
| Procedural characteristics | ||||||
| SES use | 1,050 (92) | 158 (85) | 0.004 | 1,241 (91) | 16,307 (89) | 0.08 |
| Intravascular ultrasound | 447 (39) | 57 (31) | 0.03 | 516 (38) | 7,697 (42) | 0.002 |
| Direct stenting | 163 (15) | 63 (36) | <0.001 | 234 (18) | 4,040 (23) | <0.001 |
| Postdilation | 480 (44) | 64 (37) | 0.09 | 561 (43) | 7,632 (44) | 0.87 |
| Maximum inflation pressure | 18.3 ± 3.4 | 18.3 ± 3.3 | 0.85 | 18.3 ± 3.4 | 17.7 ± 3.4 | <0.001 |
| Stents used per lesion (n) | 1.33 ± 0.83 | 1.16 ± 0.68 | 0.005 | 1.30 ± 0.79 | 1.30 ± 0.72 | 0.82 |
| Stent length per lesion (mm) | 31.1 ± 19.9 | 26.7 ± 17.4 | 0.007 | 30.4 ± 19.6 | 29.6 ± 16.9 | 0.14 |
| Minimum stent size | 2.89 ± 0.39 | 3.11 ± 0.41 | <0.001 | 2.92 ± 0.40 | 2.89 ± 0.39 | 0.006 |
The in-hospital mortality was similar between the patients with and without previous CABG (9 [0.98%] vs 97 patients [0.82%], p = 0.60). Regarding long-term follow-up, the median follow-up interval for the surviving patients was 1,699 days (interquartile range 1,184 to 1,928). The cumulative incidence of death, cardiac death, and sudden death at 5 years was significantly greater in patients with previous CABG than in those without. However, after adjusting for confounders, the excess risk of previous CABG relative to no previous CABG for death, cardiac death, and sudden death was no longer significant ( Figure 2 and Table 3 ).