Rapid supraventricular tachycardia
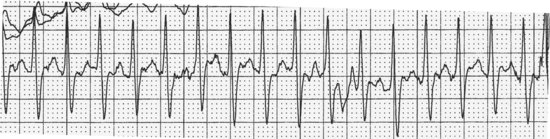
DESCRIPTION
A narrow complex rhythm which is fast, usually over 160 and sometimes even over 200 beats per minute. Generally P waves are buried in T waves or QRS complexes and can’t be seen. Typically, the rhythm starts and stops abruptly.
HABITAT
This can be found anywhere, and is often seen in young, healthy folk with no heart disease. The sudden onset of this arrhythmia may bring the victim to the Emergency Department. Episodes may happen at random, but can be triggered by cardiac stimulants (lots of caffeine, alcohol, etc.), an unexpected question from the Chief Resident, or one’s new girlfriend/boyfriend showing up before you’ve broken up with your current beau.
CALL
“Get the adenosine!”
RESEMBLANCE TO OTHER ARRHYTHMIAS
This one is usually pretty easy. It is a narrow complex rhythm (unless the baseline QRS is wide with a bundle branch pattern, in which case you may have problems!), fast and regular, and starts and stops abruptly. You could conceivably be confused by a really fast sinus tachycardia, but you should see P waves with normal orientation preceding each QRS, and sinus tachycardia will speed up and slow down gradually. If it’s narrow, fast, and irregular (break out those calipers or paper clips) then it’s probably atrial fibrillation. If it’s narrow complex, regular, and 150 beats a minute, it may be atrial flutter with 2:1 atrioventricular (AV) block (see above). If it’s wide, slow, and irregular you are really stupid and are looking in the wrong section. If you are trying to decide if it is an AV nodal reentrant tachycardia or a macroreentrant tachycardia with orthodromic conduction, you should not be reading this Field Guide. If you want to know what those words mean, however, there is a wonderful reference for you: Ganz LI and Friedman PL. Supraventricular tachycardia. N Engl J Med 1995;332:162–73. If you can understand it all you can help write the next edition of this Field Guide!
CARE AND FEEDING
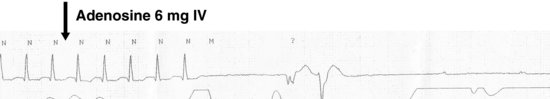
This rhythm is usually easy to convert back to sinus rhythm with various drugs or maneuvers which affect conduction through the AV node. If you are pretty sure the patient does not have an ulcerated 99% stenosis in the carotid artery, you can apply pressure over one carotid artery. The resultant vagal reflex may slow conduction through the AV node enough to terminate the tachycardia with the resumption of sinus rhythm, leaving you looking like a magician to amazed bystanders. On the other hand, if the patient strokes … Adenosine, verapamil, diltiazem, or β-blockers administered intravenously will all usually promptly convert the rhythm back to sinus, often after a terrifying pause where all those present reaffirm their faith to their respective deities.
Terror after intravenous adenosine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


