What is the next best step for diagnosis?
A. Cardiac catheterization
B. Cardiac MRI
C. Chest x-ray
D. Echocardiography
E. No further imaging, proceed to surgery immediately
49. What is the most common clinical finding in a 7-year-old patient with an anomalous right coronary artery from the left sinus?
A. Palpitations
B. Chest pain with exertion
C. No symptoms
D. Congestive heart failure
E. Syncope
50. A 10-year-old boy with a bicuspid aortic valve is scheduled for repair of a dental cavity. On the basis of the 2007 ACC/AHA endocarditis guideline statement, administration of which of the following antibiotics for this boy would be in closest accordance with current recommendations for endocarditis prophylaxis?
A. None
B. Procaine penicillin, 1 million U intramuscularly (IM), immediately prior to the procedure
C. Amoxicillin, 50 mg/kg, 1 hour prior to the procedure
D. Amoxicillin, 50 mg/kg orally, immediately after the procedure
E. Clindamycin, 20 mg/kg IM, immediately prior to the procedure
51. On the basis of the 2007 ACC/AHA endocarditis guidelines, which of the following conditions (all 5 years after their event) would warrant antibiotic prophylaxis against infectious endocarditis (IE) before a dental procedure?
A. Small residual ventricular septal defect after primary surgical closure
B. Heart transplantation
C. Bicuspid aortic valve with mild aortic regurgitation and a history of IE
D. Device closure of a secundum atrial septal defect
E. Extended end-to-end coarctation repair with a 10-mm Hg residual gradient
Answers
1. ANSWER: E. The supplemental laboratory criteria used in the diagnosis of suspected incomplete Kawasaki disease include albumin ≤3.0 g/dL, anemia for age, elevation of alanine aminotransferase, platelets after 7 days ≥450, 000/mm3, white blood cell count ≥15, 000/mm3, and urine ≥10 white blood cells/high-power field.
2. ANSWER: C. A patient with an isolated small to medium (>3 mm but <6 mm) coronary artery aneurysm in a major coronary artery is classified as risk level III. Recommended follow-up includes:
• Aspirin therapy should be continued until the aneurysms regress.
• Patients <11 years of age should have no physical activity restrictions.
• Patients 11 to 20 years of age should have stress tests every other year with myocardial perfusion performed to guide physical activity recommendations.
• Patients should be seen annually by a pediatric cardiologist with an echocardiogram and electrocardiogram.
• If a stress test shows myocardial ischemia, then coronary angiography should be performed.
3. ANSWER: E. Cholesterol screening should be performed on all children with a positive family history of dyslipidemia or premature coronary vascular disease or dyslipidemia. Screening should also be performed on all children with unknown family history or the following risk factors: overweight or obese, hypertension, cigarette smoking, or diabetes mellitus. This child was appropriately screened given his positive family history of premature coronary vascular disease. Pharmacotherapy should not be started until the child is 8 years of age. At this age, weight management should be the focus to lower the LDL level.
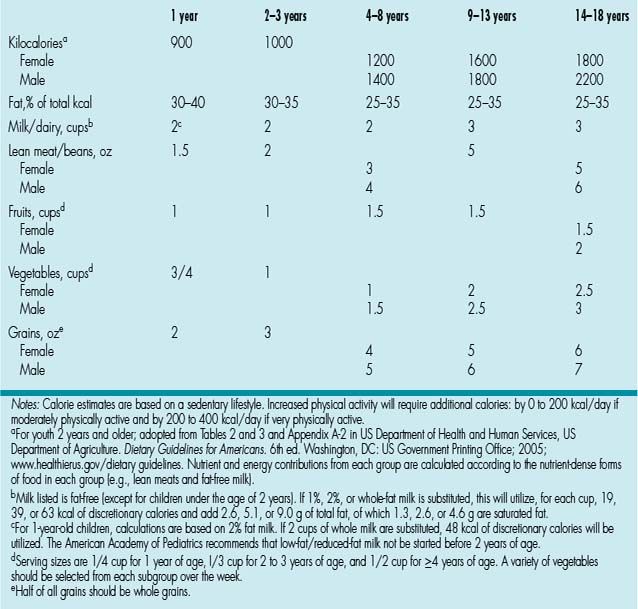
4. ANSWER: A. Recommendations are based on age and gender if 4 years or older. In this age group the total fat intake should be 25% to 35% of daily calories (62 to 85 g) with the percentage of saturated fat being 10% (or 20 to 24 g) (Table 8.1).
5. ANSWER: B. More information is needed for a conclusive diagnosis, but the patient has history and physical examination findings consistent with Marfan syndrome, in addition to a family history of aortic aneurysm.
FBN1 has been identified as the causal gene in Marfan syndrome. It is also associated with Shprintzen-Goldberg syndrome, Weill–Marchesani syndrome, and ectopia lentis syndrome. TGFBR1 is associated with Loeys–Dietz syndrome and familial thoracic aortic aneurysm syndrome. COL3A1 is associated with Ehlers–Danlos syndromes. ADAMTS10 is associated with Weill–Marchesani syndrome. ACTA2 is associated with familial thoracic aortic aneurysm syndrome.
6. ANSWER: B. This condition is inherited in an autosomal dominant pattern. Mutations in the FBN2 gene cause congenital contractural arachnodactyly.
7. ANSWER: C. β-Blockers are generally given to most patients with Marfan syndrome and aortic root dilation. Use of Losartan has increased in recent years. ACE inhibitors, ARBs, and calcium channel blockers are also used in patients with β-blocker intolerance. Digoxin usually has no role in this disease process.
8. ANSWER: A. To confirm a diagnosis of hypertension, three blood pressure measurements are needed. This patient has two blood pressures that place him >95%, and the concern is that he has stage 1 hypertension. A single third blood pressure measurement could be performed at a later date. Alternatively, ambulatory blood pressure monitoring could be used. This is especially useful if there is any concern of “white-coat” hypertension. In addition, a thorough history and physical should be performed to identify any possible causes. If the patient does have stage 1 hypertension, then he needs a diagnostic workup.
9. ANSWER: D. Pre-hypertension is defined as average systolic or diastolic blood pressure levels that are ≥90th percentile but <95th percentile. A thorough history and physical examination should be performed, and further testing performed if indicated. It is reasonable to start with lifestyle changes, and blood pressure should be repeated in 6 months.
10. ANSWER: B. The patient has auscultation findings consistent with aortic regurgitation. The systolic ejection murmur is secondary to increased stroke volume. The blowing diastolic murmur is the aortic regurgitation. Widened pulse pressure is often found in aortic stenosis, especially if it is moderate or severe. Widened pulse pressure occurs because there is an increased stroke volume that causes distension of the peripheral arteries and elevation in systolic blood pressure. Diastolic blood pressure is reduced because the regurgitation into the left ventricle leads to a rapid fall in pressure. A systolic ejection click is typically associated with the presence of a bicuspid aortic valve, which would be expected in a patient with physical findings of aortic stenosis/regurgitation
11. ANSWER: E. The diagnosis of the rheumatic fever is diagnosed based on the Jones criteria. The probability is high if there is group A streptococcal infection as well as two major criteria or one major and two minor criteria. The five major criteria are migratory arthritis, carditis and valvulitis, central nervous system involvement/Sydenham chorea, erythema marginatum, and subcutaneous nodules. The four minor criteria are arthralgia, fever, elevated ESR or CRP, and prolonged PR interval. The patient has one major criteria—valvulitis. To confirm the diagnosis, one more major criterion would need to be present. Otherwise, two minor criteria would be required to make the diagnosis.
12. ANSWER: B. In a patient with penicillin allergy, amoxicillin should also be avoided. A narrow-spectrum cephalosporin, such as cephalexin, for 10 days would be appropriate. In patients with a severe hypersensitivity reaction to penicillin, other choices include Azithromycin, but a 5-day course is recommended, and Clindamycin for a 10-day course.
13. ANSWER: A. According to the 2009 guidelines for the diagnosis and management of syncope, there are several high-risk criteria that require hospitalization or intense evaluation (Table 8.2).
Table 8.2 Risk Stratification
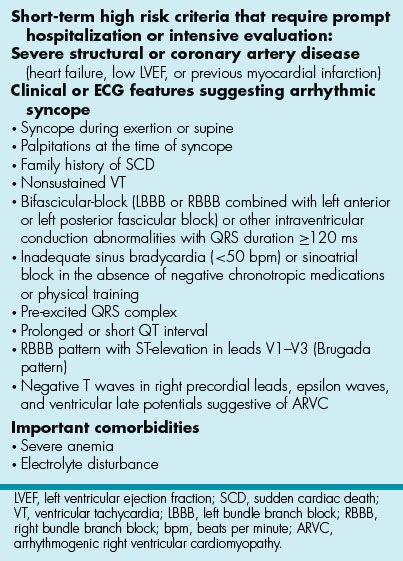
14. ANSWER: E. This patient is at high risk for major cardiovascular events based on her episodes happening with exercise and having palpitations prior to the syncope. Therefore, it is reasonable to admit her to the hospital and do inpatient monitoring while a thorough work-up is performed.
15. ANSWER: C. Endomyocardial biopsy is the gold standard for establishing the diagnosis of myocarditis, although it only yields diagnostic information in 10% to 20% of cases. Currently biopsy is a class IIb recommendation in the current American College of Cardiology/American Heart Association guidelines for the treatment of heart failure.
16. ANSWER: A. Patients with sickle cell anemia have chronic anemia and therefore have increased cardiac output. This causes the heart to become enlarged, as can be seen on chest x-ray. Increased cardiac output can cause a flow murmur heard over the left parasternal area. Thrombotic crisis will cause acute chest syndrome, but this is usually not cardiac in nature. A patient with sickle cell anemia may have prolonged PR interval and nonspecific ST changes seen on ECG, but it is rare for arrhythmias to develop. Iron overload causes the cardiac abnormalities seen with thalassemia major.
17. ANSWER: D. The majority of patients with Duchenne’s will have normal echocardiograms, including normal ventricular size and function. As the disease progresses, posterior epicardial thinning and dilated cardiomyopathy are the autopsy and echocardiographic findings. The progression of cardiac findings occurs independently from the progression of skeletal muscle changes.
18. ANSWER: A. The American Heart Association recommends using a blood pressure cuff with a bladder that is at least 40% of the arm circumference and 80% of the upper arm length. Utilizing a blood pressure cuff with measurements less than this can lead to falsely elevated measurements. Given the recent increase in pediatric obesity rates, it is important to remember that a child-size blood pressure cuff may not be appropriate for all children. While he may have a coarctation, his blood pressure should be accurately measured before undertaking further evaluation. Whether or not this child’s blood pressure is elevated, his severe obesity should be addressed. When taking an auscultatory blood pressure, the patient should be positioned in a seated position with their back flat to a firm surface. The arm should be at the level of the heart. Positioning the arm below the heart may lead to venous congestion and falsely elevated readings. There are a total of five Korotkoff sounds described. Phase 1 is considered to be the SBP and is the first appearance of faint clear tapping sounds that gradually increases and are heard for at least two consecutive beats. Phase 2 is the softening of sounds, which may have a swishing nature. During phase 3, the sounds become more sharp and crisp again compared to phase 2, but less intense than phase 1. There is no described clinical significance of phase 2 or phase 3. Phase 4 is the distinct abrupt muffling of sounds, which become soft and blowing. Phase 5 is the point at which all sounds disappear. There has been debate over the years as to whether phase 4 or 5 should be used for determining DBP. Currently the AHA recommends using phase 5.
19. ANSWER: E. There are multiple methods for the determination of blood pressure. The current gold standard for blood pressure determination in the clinical setting is utilizing a mercury sphygmomanometer. Owing to toxicity and environmental issues, these are rapidly starting to fall out of favor and are being replaced by aneroid devices. However, the error rate compared to mercury devices varies between 1% and 44% with the higher error rate being attributed to lack of regular calibration. When auscultating blood pressure, it is the first and fifth Korotkoff sounds that should be used (see question 18 explanation). When measuring blood pressure through auscultatory methods, it is recommended that the cuff be deflated at a rate of 2 to 3 mm Hg/s. Deflating too slowly may lead to an artificially high diastolic readings and deflating too quickly has been reported to lead to artificially elevated systolic readings. The oscillometric technique of blood pressure determination measures the oscillations in a blood pressure cuff during gradual deflation. The point of maximal oscillation correlates with the mean intraarterial blood pressure. This technique has the advantage of being less susceptible to external noise, but more susceptible to movement and low frequency vibration. This method is often used in ambulatory blood pressure monitoring devices and many home blood pressure monitors.
20. ANSWER: B. Patients with an isolated ASD typically will exhibit left-to-right shunting. Given that the difference in atrial pressures is relatively small, the velocity of shunting across the defect is not high enough to cause a murmur. The increased volume in the right atrium may cause a diastolic flow murmur across the tricuspid valve (if the Qp:Qs is >2:1). The systolic ejection murmur is caused by increased stroke volume across a normal pulmonary valve.
21. ANSWER: C. The constellation of symptoms in this patient is consistent with a decrease in the left-to-right shunting. The prominent S2 and paradoxical splitting indicate that the pulmonary pressures are high. As the child breathes in, RV outflow increases and the splitting resolves but with expiration the RV outflow decreases and the increased pulmonary pressures result in faster and louder closer of the pulmonary valve. If the decrease in left-to-right shunt was from the ASD becoming smaller than you would expect the splitting to be physiologic and the P2 to be of normal intensity. The diastolic murmur has resolved because the decreased left to right shunt has reduced the flow across the tricuspid valve.
22. ANSWER: E. In the setting of an untreated ASD, pulmonary vascular obstructive disease is more likely to occur in females than males. The reason for this is unclear. Pulmonary vascular disease has an occurrence of ~5% to 10% in the setting of untreated ASDs. Pulmonary vascular disease is an uncommon complication of untreated ASDs, and if it develops, it typically does so after age 20 years. Approximately 50% of patients with untreated ASDs over age 60 years and 15% of those over 40 years will develop atrial fibrillation. The vast majority (~90%) of secundum ASDs <4 mm will close spontaneously by 4 years of age.
23. ANSWER: D. This infant has signs of pulmonary overcirculation: poor feeding, tachypnea, and poor weight gain. The appropriate dose of furosemide for this patient is 1 mg/kg/dose given twice daily. One can make the case that surgical repair should be entertained in the near future but that is not one of the options. In the “patient management” type of questions always note patient age, vital signs, and lesion. Management questions will be fairly straightforward if one notes these details in the question stem.
24. ANSWER: C. The murmur described in this vignette is consistent with that of a Stills murmur. It is a common innocent murmur of childhood and thought to be periodically found in 75% to 85% of school aged children. It is classically described as being musical in nature and having the qualities listed in the question stem. The true cause of this murmur is unknown, but there are many theories including physiological narrowing of the left ventricular outflow area, systolic/diastolic hypermobility of the mitral valve chordae, small aortic diameter, the presence of left ventricular false tendons or increased aortic flow volume and velocity. Given its position, it is important to differentiate a Stills murmur from that of HCM or a VSD. The murmur of HCM would be expected to get louder with Valsalva or standing (maneuvers that decreases venous return). A VSD would not be affected by physiologic maneuvers and has a harsh quality.
25. ANSWER: B. The murmur described in the vignette is most consistent with a neonatal transitional murmur of peripheral pulmonary stenosis. Infants born prematurely and of low birth weight are more likely to have this murmur. In about 2/3 of infants, this will disappear by 6 weeks of age. The position of this murmur with radiation to the axilla and back are the hallmarks of peripheral pulmonary stenosis. Persistence beyond 6 to 9 months of age warrants further evaluation for branch pulmonary artery stenosis. A murmur of pulmonary valve stenosis would best be heard at the left upper sternal border. A right-to-left shunt at the ventricular level would result in systemic desaturation. A PDA has a continuous murmur as does an AV fistula.
26. ANSWER: A. In 2007 the American Heart Association significantly revised the guidelines for infective endocarditis prophylaxis. Prior guidelines had included not only patients considered to be in the highest risk category but also those in the moderate risk category. The new guidelines are based on the evidence that in most patients prophylaxis provides little benefit and the risk of potential adverse outcome from the medication outweighs possible benefit for all except the most high-risk patients. The highest risk patients include:
1. Patients with prosthetic heart valves, including bioprosthetic and homograft valves.
2. Patients with prosthetic material used for cardiac valve repair.
3. Patients with a prior history of IE.
4. Patients with unrepaired cyanotic congenital heart disease, including palliative shunts and conduits.
5. Patients with completely repaired congenital heart defects with prosthetic material or device, whether placed by surgery or by catheter intervention, during the first 6 months after the procedure.
6. Patients with repaired congenital heart disease with residual defects at the site or adjacent to the site of the prosthetic device.
7. Patients with “valvulopathy” in a transplanted heart. Valvulopathy is defined as documentation of substantial leaflet pathology and regurgitation.
It is recommended that prophylaxis be given for procedures that will likely result in bacteremia. These include dental procures involving manipulation of gingival tissue or the periapical region of the teeth or perforation of the oral mucosa. In regard to respiratory procedures, there is little direct evidence that bacteremias caused during these procedures lead to IE. The AHA does not recommend routine prophylaxis for respiratory procedures unless they involve incision or biopsy of the respiratory tract mucosa. Procedures in which prophylaxis would be indicated include tonsillectomy, adenoidectomy, or bronchoscopy with biopsy. The new guidelines no longer recommend prophylaxis for any GI (including diagnostic colonoscopy or esophagogastroduodenoscopy) or GU procedures, even in those patients with the highest risk lesions unless there is an active or ongoing infection of the GI or GU tract. Routine prophylaxis for either vaginal or caesarian section is not indicated unless there is an active infection which may increase the risk of IE, such as chorioamnionitis. Additional high-risk procedures would be those involving infected skin or musculoskeletal structure.
27. ANSWER: B. Gram-positive cocci, particularly Viridans group streptococcus are responsible for the vast majority of IE. Antibiotics choice should be tailored and directed against these pathogens. The first-line therapy for high-risk patients undergoing high-risk procedures (see question 9 explanation) is Amoxicillin. For patients who are unable to tolerate oral ampicillin, IV cephalosporin is appropriate. For patients with penicillin allergies who can take oral medications, Cephalexin, Clindamycin, Azithromycin, or Clarithromycin are appropriate. The medication is typically given as a single dose 30 to 60 min before beginning the procedure.
28. ANSWER: B. Dexrazoxane is an EDTA-like chelating agent that has been shown to significantly decrease both clinical and subclinical cardiotoxicity associated with doxorubicin and epirubicin. The exact mechanism of the cardioprotective effect is unknown. There is evidence that starting dexrazoxane either at the initiation of chemotherapy or after a cumulative dose of 300 mg/m2 may be beneficial. Often it is given once the aforementioned threshold is reached. At present there is debate as to whether it should be routinely used in children. There is evidence that it does reduce cardiotoxicity related to doxorubicin and epirubicin, but there is emerging data that it may lessen the effectiveness of the chemotherapy. Children are at increased risk of cardiotoxicity from anthracycline when compared to adults.
29. ANSWER: B. There are three phases of anthracycline-related cardiotoxicity. The greatest risk factor for any of these phases is related to the total cumulative anthracycline dose. The acute phase occurs within 1 week of the infusion (with higher doses cardiac dysfunction may be more immediate). This is often a transient phenomenon and can have a wide spectrum of findings from minor ECG abnormalities and sinus tachycardia to severe ventricular dysfunction and fulminant heart failure. Acute toxicity occurs in 1% of pediatric patients. Early onset chronic progressive cardiomyopathy occurs within the first year of treatment. This is a nontransient depression in myocardial function that is due to damage or death of myocytes. It occurs in ~2% of patients. Late onset toxicity occurs at least 1 year after treatment. Within 6 years of treatment, 65% of children who received 228 to 550 mg/m2 of anthracycline have some abnormality of cardiac structure or function. The risk of clinical heart failure 15 to 20 years following chemotherapy is 4% to 5%.
30. ANSWER: C. Studies in children with idiopathic PAH (IPAH) and hereditary PAH (HPAH) have shown that the survival of those treated prior to the advent of targeted therapies (1950s to 1990s) was 66%, 52%, and 35% for 1, 3, and 5 years, respectively. Studies utilizing targeted therapies such as sildenafil, bosentan, and IV prostacyclin have shown considerable improvement in the mortality as well as the symptoms associated with PAH. The 1-, 3-, and 5-year mortality rates improved to 94%, 88%, and 81% from a number of studies. The most likely presenting symptoms in children with PAH are dyspnea and fatigue. Children are unlikely to present with right heart failure as an initial finding as they are often quite active and dyspnea on exertion is an early symptom. Children or adults who develop PAH as a result of unrepaired congenital heart disease such as a large VSD typically have a lower mortality than those with IPAH or HPAH as it takes more time for secondary PAH to develop.
31. ANSWER: D. According to the 2008 AAP Committee on Nutrition Guidelines, patients with diabetes mellitus are at particular risk of coronary complications from hyperlipidemia. The most appropriate next step would be to start a statin at this time since the LDL is marked elevated. Review the tables in this guideline statement prior to the board exam for a quick study aid on the topic of hyperlipidemia screening and management in children.
32. ANSWER: C. This patient’s examination is most consistent with someone who has pulmonary vascular disease. After longstanding left-to-right shunting through a large VSD, the patient has now developed elevated pulmonary vascular resistance and elevated RV pressure. The shunt has reversed and is now right to left, hence the systemic desaturation. The right and left ventricular pressures are likely equal, and there is low velocity flow across the VSD that is inaudible. As a result of the increased pulmonary pressures, she has developed right ventricular hypertrophy (RVH) resulting in the parasternal lift. LVH would present as a lift or heave along the apex. As a result of the RVH and the increased pulmonary pressures, she has developed audible tricuspid regurgitation. As result of the RVH, the murmur is displaced more rightward than normal. If the murmur were from increased pulmonary flow, it would be expected along the upper left sternal border and would likely be ejection in quality.
33. ANSWER: B. See AAP guideline statement.
34. ANSWER: A. The sister with a long QT should be restricted to class IA activities. She is asymptomatic but has baseline QT prolongation (QTc >470 ms or more in males, >480 ms or more in females) so she should be restricted to class 1A sports. Only if she had genetically proven type 3 LQTS, the restriction limiting participation to class IA activities may be liberalized. But the sisters have LQT1.
The sister with genotype-positive/phenotype-negative LQTS (i.e., identification of a LQTS-associated mutation in an asymptomatic individual with a nondiagnostic QTc) may be allowed to participate in competitive sports. The risk of sudden cardiac death is not zero, but there are no compelling data available to justify restricting these individuals from competitive activities.
Because of the strong association between swimming and LQT1, both sisters should refrain from competitive swimming.
The presence of an ICD would restrict both sisters to class IA activities.
35. ANSWER: A. DCRV is an acquired lesion that generally presents in older children and in adulthood. Narrowing of the RV outflow tract develops in patients with membranous VSDs due to hypertrophy of muscle in the right ventricular infundibulum. When anomalous bands of muscle divide the RV cavity into two chambers, DCRV can occur.
DCRV has been reported to be in association with VSD in 63% to 90% of patients.
36. ANSWER: D. The risk of infective endocarditis coincides with severity of regurgitation, not with abnormal structure of a competent valve. Paradoxical emboli are rare with ostium primum defects in contrast to ostium secundum defects because emboli that originate in the lower extremities are carried by IVC blood toward the mid portion of the atrial septum. SVC streaming targets the lower atrial septum, but emboli rarely originate in the upper extremities. Spontaneous closure of the ventricular component of an AVSD is rare and has been attributed to occlusion by tricuspid leaflet tissue derived from the bridging leaflets. The chief determinant of symptoms in a nonrestrictive ostium primum atrial septal defect is coexisting left AV valve regurgitation. Severe preoperative regurgitation results in early congestive heart failure, higher postoperative mortality, and increased risk of more than moderate postoperative regurgitation.
The incidence of congenital heart disease with Down syndrome is ~40% to 50% compared with an incidence of 0.8% for infants with normal chromosomes. Complete AVSD accounts for two-thirds of the CHD observed in Down syndrome.
37. ANSWER: D. Neurocardiogenic (vasovagal) syncope is very common in the teenage population. The most cost-effective initial evaluation includes taking a detailed history to insure that there is no family history of sudden death. After the history and physical examination, the next appropriate test is an ECG if the patient has had no previous evaluation. The other tests listed may be considered if further evaluation is needed or the examination and history raise suspicion of specific pathology.
38. ANSWER: A. Chest wall pain is the most common cause of chest pain in children. Types of chest wall pain include costochondritis, Tietze syndrome, nonspecific (idiopathic) chest wall pain, precordial catch syndrome, slipping rib syndrome, hypersensitive xiphoid syndrome, trauma and muscle strain, and sickle cell disease. Other, less common causes of chest pain include asthma, infection, pericarditis, gastrointestinal, and pneumothorax. Least common are cardiac causes of chest pain that include HCM, aortic stenosis, pericarditis, arrhythmias, coronary insufficiency, dissecting aortic aneurysm, and mitral valve prolapse. The most common causes of coronary insufficiency in children are Kawasaki disease, Williams syndrome, anomalous origin of the coronary arteries and coronary arteriovenous and coronary cameral fistulae.
39. ANSWER: B. Pulsus paradoxus is defined as an exaggeration of the normal variation during the inspiratory phase of respiration, in which the blood pressure declines as one inhales and increases as one exhales. It is one of the hallmarks of cardiac tamponade. It is also a sign that is indicative of several other conditions including pericarditis, chronic sleep apnea, croup, and obstructive lung disease such as asthma or COPD.
Normally, inspiration results in negative intrathoracic pressures which cause an increase in systemic venous return to the right heart, it increases the capacity of the pulmonary vascular bed to a greater degree. This ultimately leads to a decrease in left sided output even though there is increased systemic venous return to the right. In cardiac tamponade, right ventricular filling causes restriction to left ventricular filling. With inspiration, this decreased left ventricular filling, coupled with the increased capacity of the pulmonary vascular bed, results in a greater reduction in systemic output and therefore a greater decline in systolic pressure (>10 mm Hg). To measure pulsus paradoxus, one should listen for the difference between the first Korotkoff sound (intermittent and heard only during exhalation) and the second Korotkoff sound (a constant sound not dependent on respiratory cycle) as a reflection of the pulsus paradoxus; this is best accomplished by slow deflation of the BP cuff, but can also be observed by a difference in systolic BP recorded on an invasive arterial pressure monitoring line in relationship to respiration.
40. ANSWER: B. Early diastolic murmurs begin immediately after S2 and are decrescendo in nature. High-pitched early diastolic murmurs are due to aortic regurgitation with higher diastolic pressure in the aorta. They are heard best with the diaphragm at the left midsternal border. This murmur radiates to the apex and is decrescendo in nature due to a decrease in intensity of the murmur as the diastolic pressure gradient equalizes. This is also why the murmur is accentuated when the patient leans forward and exhales.
Pulmonary valve regurgitation also produces an early diastolic murmur that is generally low pitched, but can be high pitched if pulmonary hypertension is present. They are also heard at the left midsternal border or at the left upper sternal border, however radiation of this murmur is down the left sternal border. Patients with significant pulmonary regurgitation have murmurs with to and fro qualities due to increased forward volume load during ejection across the pulmonary valve.
Tricuspid and mitral valve stenosis cause mid-diastolic or late diastolic murmurs. These murmurs are produced during the early filling phase of diastole when blood crosses a narrow or thickened AV valve (mid-diastolic) or with atrial contraction (late diastolic). These murmurs are low pitched and are heard best with the bell of the stethoscope.
Mitral valve regurgitation results in a high-pitched holosystolic murmur at the apex with radiation to the back, left axilla or clavicular area.
41. ANSWER: C. The 12-lead ECG is practical and cost-effective when used to further evaluate an athlete with a suspected cardiovascular abnormality. Other common noninvasive testing modalities include echocardiography, Holter ECG, and exercise test. However, due to the cost and lesser practicality of these studies, the 12-lead ECG is the preferred first test when evaluating athletes with suspected cardiovascular abnormality.
42. ANSWER: E. Cardiac involvement in ARF has been considered a pancarditis. The most important clinical abnormalities in ARF are related to valvular pathology and regurgitation rather than myocarditis or myocardial dysfunction. Endomyocardial biopsy in ARF does not show myocyte necrosis associated with lymphocytic infiltration. Troponin I levels are not elevated and several studies have demonstrated that left ventricular shortening and ejection fraction remain normal. Valvular dysfunction is the main determinant of clinical outcome in rheumatic carditis. Heart failure does not occur in either acute or chronic rheumatic carditis in the absence of significant valvular dysfunction.
43. ANSWER: E. All these entities have been implicated as a cause of sudden cardiac death in the young. Many studies have described hypertrophic cardiomyopathy as the most common cause of sudden cardiac death in young athletes.
44. ANSWER: B. After birth, as pulmonary artery pressures fall below systemic pressures and the pulmonary artery contains desaturated blood, left ventricular perfusion is compromised. Collateral flow is initially low, as collaterals do not form in fetal life when the pressures in the aorta and pulmonary arteries are essentially equal. As the left ventricle’s demand for oxygen is not met, the left ventricular myocardial vessels dilate to reduce resistance and increase flow. When coronary vascular reserve is exhausted, the result is myocardial ischemia. In response to ischemic stimuli, collateral vessels form and enlarge between the normal right and the abnormal left coronary arteries. However, with the left coronary artery connected to the low-pressure pulmonary artery, there is pulmonary–coronary steal as blood tends to flow into the pulmonary artery rather than into the high-resistance myocardial vessels. This results in a left-to-right shunt, which is not significant in terms of cardiac output but which can be critical in terms of coronary flow and creating a “steal” phenomenon and resultant myocardial ischemia.
Any lesion that increases pressure in the pulmonary artery will help to decrease the pulmonary–coronary steal. If there is pulmonary hypertension, as may result with a large VSD or PDA, there may be adequate pulmonary artery pressure to drive left ventricular perfusion and to prevent left ventricular ischemia. In these cases, closure of the VSD or PDA results in a decrease in pulmonary arterial pressure, an effect that may decrease perfusion of the anomalous left coronary artery.
45. ANSWER: A. There are several metabolic disorders resulting from specific enzyme deficiencies that cause RCM. These include Hurler syndrome, Gaucher disease, Fabry disease, and glycogen-storage diseases that can be lysosomal disorders or cytoplasmic enzyme deficiencies. Amyloidosis does result in RCM; however, this disease is seen almost exclusively in the adult population, with only one reported case to date in the pediatric literature. Thiamin deficiency, muscular dystrophy, and collagen vascular diseases all cause dilated cardiomyopathy, not RCM.
46. ANSWER: B. Cardiovascular manifestations are common in SLE. 50% to 80% of patients report some cardiovascular complication in their lifetime. The most frequent clinically apparent cardiovascular complication is pericarditis with a frequency of ~25% and a pericardial effusion may be detected in as many as 50% of patients.
While necropsy studies have found evidence of myocarditis in as many as 40% of SLE cases, the rate of clinically evident myocarditis has been reported in <25% of patients. While less common, lupus myocarditis is an important cardiovascular complication because it has the potential to precipitate heart failure and arrhythmia and may contribute to the insidious development of cardiomyopathy. Angina is a complication of SLE, especially in the adult population, though not as common as pericarditis. Angina results from extramural and intramural coronary arteritis, accelerated atherosclerosis, embolism, thrombosis, spasm, or any combination thereof. These complications may be secondary to prolonged corticosteroid therapy and/or related to other lupus non-steroid-related mechanisms such as lupus-induced lipid disturbances, lupus-related antiphospholipid antibodies, and lupus-related intimal damage. Aortic dissection is not a common cardiac manifestation of SLE.
47. ANSWER: B. The most important factor in determining prognosis and natural history of rheumatic carditis and RHD is the severity of the initial carditis and rheumatic fever recurrence. Severe initial carditis and/or patients with recurrent episodes of rheumatic fever are more likely to develop persistent RHD than those with mild carditis and no recurrence.
Of those patients with acute valvular involvement, the prognosis for resolution is more favorable for acute mitral regurgitation than it is for acute aortic regurgitation. This is in part because aortic regurgitation usually occurs in combination with mitral regurgitation. Isolated aortic regurgitation only occurs in ~5% of patients with acute rheumatic carditis. Aortic regurgitation with mitral regurgitation occurs in ~15% to 20%.
Age and gender also play a role in the natural history of rheumatic carditis and RHD. Acute rheumatic carditis resolves more frequently in boys. More severe cardiac involvement and RHD are seen in patients who present before the age of 5 years.
48. ANSWER: D. The ECG demonstrates deep q waves in leads I, aVL, and leads V4–V6. There is T wave inversion, in leads I and aVL and the precordial leads. These findings strongly suggest ALCAPA. Furthermore, the clinical history is also suggestive with increased work of breathing and sweating and crying with feeds. Echocardiography with color Doppler flow imaging is the standard of diagnosis. Alternative imaging may be considered if the diagnosis is unclear after detailed transthoracic echocardiography is performed.
49. ANSWER: C. If an anomalous coronary arises from the opposite sinus of Valsalva, it is very unlikely to pass between the aorta and the right ventricular infundibulum, which is when it is at most risk for myocardial ischemia. Therefore, most people with this anomaly are completely asymptomatic. There is, however, a risk of sudden death with this anomaly, although the exact incidence is unknown. Basso et al. reported 27 deaths in young athletes whose autopsies showed anomalous origin of a coronary artery from the wrong sinus. Fifteen athletes had no prior cardiovascular symptoms. Of the remaining 12 patients, 10 had symptoms including 4 with syncope, 5 with chest pain, 2 with palpitations, and 1 with dizziness.
50. ANSWER: A. See explanation to question 26.
51. ANSWER: C. See guideline statement and explanation to question 26.
SUGGESTED READINGS
Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adam’s Heart Disease in Infants, Children and Adolescents. 7th ed. Philadelphia, PA: Lippincott Williams, and Wilkins; 706–709.
Allen HD, Mendell JR, Hoffman TM. The heart in muscular dystrophies. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents. Philadelphia, PA: Lippincott, Williams and Wilkins, 2008:1514–1524.
American Heart Association. Dietary recommendations for children and adolescents. Circulation. 2005;112:2061–2075.
Barst RJ, Ertel SI, Beghetti M, et al. Pulmonary arterial hypertension: a comparison between children and adults. Eur Res J. 2011;37(3):665–677.
Basso C, Maron BJ, Corrado D, et al. Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J Am Coll Cardiol. 2000;35(6):1493–1501.
Congenital Contractural Arachnodactyly. 2011. NCBI.
Corrigan JJ. Hematologic aspects of pediatric cardiology. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents. Philadelphia, PA: Lippincott, Williams and Wilkins, 2008:1514–1524.
Daniels SR, Greer FR; Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122:198–208.
Gerber MA, Baltimore RS, Eaton CB, et al. Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis. Circulation. 2009;119(11):1541.
http://www.bcm.edu/cnrc/consumer/archives/percentDV.htm
Lipshultz SE, Colan SD, Gelber RD, et al. Late cardiac effects of doxorubicin therapy for acute lymphoblastic leukemia in childhood. N Engl J Med. 1991;324(12):808.
Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010;47:476–
485.
Magnani JW, William G. Myocarditis: current trends in diagnosis and treatment. Circulation. 2006;113:876–890.
McDaniel NL, Gutgesell HP. Ventricular Septal Defects, Moss and Adams Heart Disease in Infants, Children, and Adolescents. Philadelphia, PA: Lippincott Williams, and Wilkins, 2008:667–672.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555.
Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment and long-term management of Kawasaki disease…. Pediatrics. 2004;114:1708–1733.
O’Brien ET, O’Malley K. ABC of blood pressure measurement: technique. Br Med J. 1979;2(6196):982–984.
Ogedegbe G, Pickering T. Principles and techniques of blood pressure measurement. Cardiol Clin. 2010;28(4):571–586.
Porter CJ, Edwards WD. Atrial septal defects. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents. Philadelphia, PA: Lippincott, Williams and Wilkins, 2008:632–634.
Rocchini AP. Sports screening and participation. In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents. Philadelphia, PA: Lippincott, Williams and Wilkins, 2008:66–80.
Ruggiero A, Ridola V, Puma N, et al. Anthracycline cardiotoxicity in childhood. Pediatr Hematol Oncol. 2008;25(4):261–
281.
Smith LA, Cornelius VR, Plummer CJ, et al. Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomized controlled trials. BMC Cancer. 2010;10:337.
The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology, et al. Guidelines for the
diagnosis and management of syncope (version 2009). Eur Heart J. 2009;30(21):2631–2671.
Wilson W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association…. Circulation.2007;116:1736–1754.
Zipes DP, Ackerman MJ, Estes NA III, et al. Task Force 7: arrhythmias. JACC. 2005;45:1354–1363.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


