Adequate health care is increasingly dependent on prehospital systems and cardiovascular (CV) disease remains the most common cause for hospital admission. However the prevalence of CV dispatches of emergency medical services (EMS) is not well reported and survival data described in clinical trials and registries are subject to selection biases. We aimed to describe the prevalence and prognosis of acute CV disease and the effect of invasive treatment, in an unselected and consecutive prehospital cohort of 3,410 patients calling the national emergency telephone number from 2005 to 2008 with follow-up in 2013. Individual-level data from national registries were linked to the dedicated EMS database of primary ambulance dispatches supported by physician-manned emergency units. Outcome data were obtained from the Central Population Registry, the National Patient Registry, and the National Registry of Causes of Death. In patients calling the national emergency telephone number, a CV related ambulance alarm code was given in 2,541 patients of 3,410 patients (74.5%) resulting in 2,056 of 3,410 primary CV discharge diagnoses (60.3%) with a 30-day and 5-year all-cause mortality of 24.5% and 46.4%, respectively. Stroke, acute heart failure, and ST-segment elevation myocardial infarction (STEMI) carried a 25- to 50-fold adjusted mortality hazard during the first 4 days. In patients with suspected STEMI, 90.5% had an acute angiography performed. Nontransferred, nonreperfused patients with STEMI (9.1%) carried 80% short-term mortality. Noninvasive management of non–ST-segment elevation myocardial infarction was common (37.9%) and associated with an increased adjusted long-term mortality hazard (hazard ratio 4.17 [2.51 to 8.08], p <0.001). Survival in 447 out-of-hospital cardiac arrest patients (13.1%) was 11.6% at 30 days. In conclusion, patients with a CV ambulance alarm call code and a final CV discharge diagnosis constitute most patients handled by EMS with an extremely elevated short-term mortality hazard and a poor long-term prognosis. Although co-morbidities and frailty may influence triage, this study emphasizes the need for an efficient prehospital phase with focus on CV disease and proper triage of patients suitable for invasive evaluation if the outcomes of acute heart disease are to be improved further in the current international context of hospitals merging into highly specialized entities resulting in longer patient transfers.
An uncovered need remains for investigating the true underlying mortality rates in acute cardiovascular (CV) disease. Recently, a national Danish survey based on the National Patient Registry, in which all hospitalized patients are coded according to the International Classification of Diseases (ICD-10), showed a 14.8% (confidence interval 14.5% to 15.2%) 30-day mortality rate from 2004 to 2008 for all myocardial infarctions diagnoses (ICD I21 diagnoses: ST-segment elevation myocardial infarction [STEMI], non–ST-segment elevation myocardial infarction [NSTEMI], and unspecified myocardial infarction [MI]), an incidence that is considerably higher than those reported in randomized clinical trials and registries. Because of this mortality discrepancy between randomized clinical trials, registries, and national data, we relied on a prehospital register of patients with a potential upstream acute CV diagnosis, enabling us to follow primary discharge diagnoses of patients calling emergency medical services (EMS) for suspected CV disease, rather than relying on acute coronary syndrome (ACS) discharge diagnoses obtained after admission at the invasive center in a consequently selected patient population. To describe the burden of CV disease in an EMS setting is important, as adequate health care is increasingly dependent on elaborate prehospital systems because hospitals condensate into fewer and highly specialized entities, conjoining smaller or rural hospitals and thereby enhancing catchment areas and transfer distances. We aimed to describe the prevalence and prognosis of CV disease in an upstream unselected prehospital cohort of patients calling the national emergency telephone number, for example 112 or 911.
Methods
We investigated a consecutive Danish cohort of 4,083 patient contacts with EMS in Storstrøm County in the southern part of Zealand (262,781 inhabitants and 3,398 km 2 ). The former Storstrøm county is a nonurban region of small cities with <45,000 inhabitants and confluent suburban areas, as well as large areas of rural character. The rate of elderly citizens >75 years of age is higher than the national average. Population increase, educational level, employment rate, and self-assessed health are lower than the national average, whereas the average alcohol and cigarette consumption and the incidence of long-term sick leave are above national average.
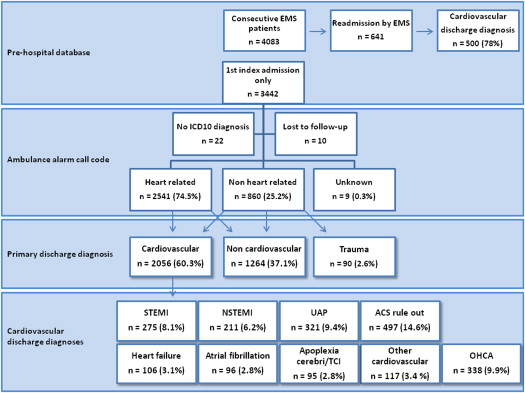
The prehospital organization in this study has been previously described. Usually the first EMS to arrive at scene is the primary ambulance staffed by emergency medical technicians or paramedics. These primary ambulances are supported by emergency medical units manned with physicians. A patient contact was registered every time a patient called the national emergency telephone number, activating a primary ambulance and physician-manned unit. Calls that did not result in an ambulance dispatch were not registered. Patients were entered, regardless of vital status at the arrival of EMS and regardless of being permanent residents in Storstrøm county. We only considered the first admission of every patient and excluded 641 (15.7%) register entries of patients repeatedly admitted by EMS ( Figure 1 ).
The physician-manned units are fast vehicles without the space to transport patients, but are dispatched simultaneously with the primary ambulance to the injury site for a so-called “rendezvous” with the primary ambulance at the injury site or on the way, to triage and initiate advanced treatment for stabilization before transport. Patients were transferred to 2 around the clock invasive centers in Copenhagen and 4 noninvasive hospitals within the county.
We linked individual-level data from national registries to the dedicated prehospital EMS database, using the personal registration number provided to all Danish residents. The inclusion period was May 1, 2005, to January 31, 2008, with follow-up from May 6, 2013, to May 14, 2013. The EMS database contained data entries based on ambulance charts reporting time information on alarm call, arrival at scene, departure from scene and hospital arrival, vital parameters, and the tentative prehospital diagnosis. Outcome data were obtained from the Central Population Registry, the National Patient Registry, and the National Registry of Causes of Death, enabling follow-up of all patients who had not emigrated. Long-term follow-up was at least 5 years in all patients, maximum follow-up was 8 years, and median follow-up was 5 years and 6 months.
Patients were categorized according to their primary discharge diagnosis based on the ICD-10 codes. STEMI was defined by the ICD-10 codes I210B, I211B, and I213, and NSTEMI was defined by the codes I210A, I211A, and I214. The diagnosis of MI has been validated in the National Patient Registry. Patients treated invasively with diagnostic coronary angiography, percutaneous coronary intervention (PCI), or coronary artery bypass grafting (CABG) were also registered in the eastern Denmark PCI database. Non specified MI was defined by I219. In these patients, we applied all available data from the registries, as well as the eastern Denmark PCI database and individual discharge letter reviews, to allocate I219 to either the STEMI or NSTEMI group. Unstable angina pectoris (UAP) was defined by I200 and also by I208, I209 and I259, as patients in this population called 112 for chest pain due to acute onset or aggravation of known angina pectoris. ACS rule-out diagnosis was defined by a discharge diagnosis Z034, Z035, and R072-74. Heart failure was defined by I420, I500-509, and R570; atrial fibrillation by I48-I489; and out-of-hospital cardiac arrest (OHCA) by ambulance charts and I46-I469 at emergency room arrival. The term OHCA covers both patients with community cardiac arrest and cardiac arrest during ambulance transfer. Chronic kidney disease was defined by N17-19. The study was approved by the Danish Data Protection Agency (2011-41-5849) and the National Board of Health (7-505-29-1710/1/FSE).
Continuous variables are presented as mean ± SD. The independent samples t test was used for comparison. Discrete data are presented as frequencies and percentages. The chi-square test, Fisher’s exact test, Mann-Whitney test, and Kruskal-Wallis test were used for comparison of categorical and continuous variables as appropriate. Mortality hazards were adjusted for age and gender in multivariate Cox regression analysis. Hazard ratios are presented according to time interval after admission by EMS with patients discharged with an ACS rule-out diagnosis as the reference group. Independent predictors of all-cause 30-day to 5-year mortality in non–ST-segment elevation (NSTE)-ACS were identified using Cox proportional hazard regression analysis. We excluded patients with STEMI from the prediction analysis of invasive management, as patients with STEMI per definition are invasively managed because of the Danish national reperfusion strategy with primary percutaneous coronary intervention (pPCI). Also the survival benefit of invasive management in patients with STEMI is well established. The statistical significance level was p <0.05 (2-sided test). Data were analyzed using the PASW Statistics 18 software package (SPSS Inc., Chicago, Illinois).
Results
In 3,442 consecutive patient contacts calling the national emergency telephone number, follow-up was 99.2% complete; thus, we included 3,410 patients. A CV related diagnosis by ambulance call alarm code was given in 2,541 (74.5%) of patients and a CV related final primary discharge diagnosis in 2,056 (60.3%) of patients ( Figure 1 ). Of these, 1,294 (38%) patients were discharged with an ischemic heart disease–related diagnosis. Baseline characteristics and crude mortality rates according to discharge diagnosis are listed in Tables 1 and 2 , respectively.
| STEMI | NSTEMI | UAP | ACS rule out | |
|---|---|---|---|---|
| Variable | (n=275) | (n=211) | (n=321) | (n=497) |
| Men | 198 (72%) | 133 (63%) | 216 (67.3%) | 290 (58.4%) |
| Age (years) | 65.0 ± 13.1 | 71.2 ± 13.1 | 68.5± 13.3 | 62.9 ± 15.7 |
| Diabetes mellitus | 41 (14.9%) | 37 (17.5%) | 63 (19.6%) | 72 (14.5%) |
| Chronic kidney disease | 9 (3.3%) | 21 (10%) | 20 (6.2%) | 15 (3%) |
| Prior myocardial infarction | 35 (12.7%) | 58 (27.5%) | 98 (30.5%) | 50 (10.1%) |
| Prior percutaneous coronary intervention | 19 (6.9%) | 25 (11.8%) | 78 (24.3%) | 33 (6.6%) |
| Prior coronary artery bypass | 3 (1.1%) | 9 (4.3%) | 41 (12.8%) | 9 (1.8%) |
| Prior stroke | 9 (3.3%) | 17 (8.1%) | 24 (7.5%) | 33 (6.6%) |
| Invasive management (Total of CAG without PCI, PCI, CABG) | 249 (90.5%) | 131 (62.1%) | 56 (17.4%) | 0 (0%) |
| N | 30 day | 1 year | 3 year | 5 year | |
|---|---|---|---|---|---|
| STEMI | 275 | 40 (14.5%) | 49 (17.8%) | 63 (22.9%) | 82 (29.8%) |
| NSTEMI | 211 | 21 (10%) | 52 (24.6%) | 75 (35.5%) | 94 (44.5%) |
| UAP | 321 | 12 (3.7%) | 34 (10.6%) | 72 (22.4%) | 105 (32.7%) |
| ACS rule out | 497 | 7 (1.4%) | 45 (9.1%) | 86 (17.3%) | 114 (22.9%) |
| Heart failure | 106 | 34 (32.1%) | 54 (50.9%) | 71 (67%) | 78 (73.6%) |
| Atrial fibrillation | 96 | 4 (4.2%) | 18 (18.8%) | 34 (35.5%) | 41 (42.7%) |
| Stroke | 95 | 33 (34.7%) | 41 (43.2%) | 54 (56.8%) | 62 (65.3%) |
| Other Cardiovascular | 117 | 16 (13.7%) | 26 (22.2%) | 33 (28.2%) | 39 (33.3%) |
| Total Cardiovascular | 2056 | 503 (24.5%) | 656 (31.9%) | 826 (40.2%) | 953 (46.4%) |
| Non Cardiovascular | 1264 | 138 (10.9%) | 261 (20.6%) | 417 (33%) | 521 (41.2%) |
| Trauma | 90 | 6 (6.7%) | 11 (12.2%) | 19 (21.1%) | 22 (24.4%) |
| Total emergency medical services population | 647 (19%) | 928 (27.2%) | 1250(36.7%) | 1496(43.9%) |
Patients with a primary STEMI discharge diagnosis were invasively investigated in 90.5% of cases. Those treated with pPCI within 12 hours had a 30-day mortality of 6.3%, whereas patients who did not undergo any attempt of reperfusion had a 30-day mortality rate of 80% ( Table 3 ). The reasons for nonreperfusion were death at the local hospital before transfer in 17 cases (68%) and 4 patients (16%) were judged too frail. Three patients (12%) were not accepted by the attending cardiologist at the pPCI center, and 1 patient (4%) refused transfer. Nonreperfused patients were significantly older (median 81 years [interquartile range 70 to 87] vs 64 [interquartile range 55 to 73], p <0.001), more often women (48% vs 26%, p = 0.019), had higher incidence of previous stroke (16% vs 2%, p <0.001) and diabetes (32% vs 13.2%, p = 0.012), presented more often with prehospital hypotension (35.1% vs 15%, p = 0.022) and tachycardia (57.1% vs 25.4%, p = 0.002), and more frequently had OHCA before admission at the non-pPCI center (24% vs 10.8%, p = 0.053).
| N | 30 day | 1 year | 3 year | 5 year | |
|---|---|---|---|---|---|
| Primary percutaneous coronary intervention | 222 (80.7%) | 14 (6.3%) | 19 (8.6%) | 30 (13.5%) | 45 (20.3%) |
| Percutaneous coronary intervention >12 hours | 11 (4%) | 1 (9.1%) | 3 (27.6%) | 3 (27.6%) | 7 (63.6%) |
| Acute coronary artery bypass graft | 8 (2.9%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Acute coronary angiography, no percutaneous coronary intervention | 8 (2.9%) | 4 (50%) | 4 (50%) | 7 (87.5%) | 7 (87.5%) |
| Transferred, no coronary angiography | 1 (0.4%) | 1 (100%) | 1 (100%) | 1 (100%) | 1 (100%) |
| Not transferred | 25 (9.1%) | 20 (80%) | 22 (88%) | 22 (88%) | 22 (88%) |
In patients with NSTEMI, an angiography was performed in 62.1% of the cases. Of these, 34.6% were treated by PCI within 30 days and 9% by CABG within 90 days, and 37.9% were noninvasively managed. In patients with UAP, 17.4% of patients had an angiography performed, whereas 4.7% were treated by PCI within 30 days and 3.4% by CABG within 90 days, and 82.6% were noninvasively managed. The mortality rates according to treatment for patients with NSTE-ACS are listed in Table 4 . Noninvasively treated patients with NSTE-ACS had higher all-cause mortality in the period from 30 days to 5 years (41.5% vs 18.6%, p <0.001) compared with invasively handled patients with a coronary angiography (CAG) <30 days. Patients without invasive management were older (71.6 ± 13.1 vs 65.7 ± 12.8, p <0.001) and had a higher burden of CV disease in terms of more known ischemic heart disease (51.8 vs 39.7%, p = 0.008) and CABG (12.2% vs 3.9% p = 0.002). In patients with NSTEMI, prehospital tachycardia (Heart rate >100; 54.3% vs 28.4%. p <0.001) was more frequent in patients without invasive management. There were no differences for gender, known chronic kidney disease, previous stroke, and diabetes.
| N | 30 day | 1 year | 3 year | 5 year | |
|---|---|---|---|---|---|
| Percutaneous coronary intervention | 88 (16.5%) | 1 (1.1%) | 2 (2.3%) | 6 (6.8%) | 13 (14.8%) |
| Coronary artery bypass graft | 30 (5.6%) | 2 (6.7%) | 5 (16.7%) | 6 (20%) | 9 (30%) |
| Coronary angiography, no revasc. | 69 (13%) | 1 (1.4%) | 10 (14.5%) | 11 (15.9%) | 16 (23.2%) |
| Non-invasive treatment | 345 (64.8%) | 29 (8.4%) | 69 (20%) | 124 (35.9%) | 161(46.7%) |
Medical management without subacute CAG performed within 30 days was independently associated with 30-day and 5-year all-cause mortality. Other independent long-term predictors were age, gender, diabetes, chronic kidney disease, prehospital tachycardia, and an NSTEMI diagnosis ( Table 5 ). Age and gender adjusted hazard ratios are shown in Figure 2 . All CV diagnoses had substantially elevated risk of all-cause mortality during the first 4 days after admission, which mitigated to nonsignificant hazard levels after 30 days from EMS admission, except for patients with NSTEMI, heart failure and stroke, where mortality risk remained significantly elevated during the 5-year follow-up.
| Univariable | Multivariable | |||
|---|---|---|---|---|
| HR (95 % CI) | P | HR (95 % CI) | P | |
| Age | 1.08 (1.06 – 1.09) | <0.001 | 1.08 (1.06 – 1.10) | <0.001 |
| Female | 1.36 (0.99 – 1.85) | 0.054 | 0.65 (0.45 – 0.93) | 0.020 |
| Diabetes | 1.53 (1.07 – 2.19) | 0.019 | 1.61 (1.07 – 2.41) | 0.030 |
| Prehospital HR >100 | 2.62 (1.88 – 3.64) | <0.001 | 2.05 (1.43 – 2.94) | <0.001 |
| Prehospital SBP <100 | 1.69 (0.99 – 2.88) | 0.054 | ||
| Prior Stroke | 1.53 (0.92 – 2.52) | 0.099 | 1.68 (0.95 – 2.98) | 0.075 |
| Chronic Kidney Disease | 3.47 (2.28 – 5.28) | <0.001 | 1.99 (1.21 – 3.27) | 0.007 |
| Non-invasively managed ∗ | 3.69 (2.04 – 6.67) | <0.001 | 4.17 (2.51- 8.08) | <0.001 |
| NSTEMI vs. UAP | 1.39 (1.01 – 1.87) | 0.041 | 1.87 (1.28 – 2.73) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


