Normotensive patients with acute pulmonary embolism (PE) who have increased troponin levels and right ventricular (RV) dysfunction are thought to be at high risk of death, but the level of risk is unclear. We retrospectively evaluated outcome in 1,273 stable patients with PE who had echocardiographic evaluations of RV size and/or measurement of cardiac troponin I (cTnI). In-hospital all-cause mortality was higher in those with RV enlargement (8.0%, 19 of 237, vs 3.3%, 22 of 663, p = 0.003). With an increased cTnI, irrespective of RV enlargement, all-cause mortality was 8.0% (28 of 330) versus 1.9% (15 of 835) in patients with a normal cTnI (p <0.0001). In patients with an increased cTnI combined with an enlarged right ventricle, all-cause mortality was 10.2% (12 of 118) compared to 1.9% (8 of 421) in patients who had neither (p <0.0001). These data show that increased levels of cTnI and RV enlargement are associated with an adverse outcome in stable patients with acute PE. In conclusion, increased levels of cTnI in combination with RV enlargement might indicate a group who would benefit from intense monitoring and aggressive treatment if subsequently indicated. The outcomes, however, were not extreme enough to warrant routine thrombolytic therapy.
Cardiac biomarkers, especially troponin levels, have emerged as a promising tool for risk stratification of patients with acute pulmonary embolism (PE). Risk assessment of PE with cardiac troponin I (cTnI) has shown a slight superiority compared to cardiac troponin T (cTnT). Right ventricular (RV) dysfunction alone in a patient with PE and normal systolic blood pressure may indicate “impending hemodynamic instability.” It has been suggested that normotensive patients with an increased troponin level should undergo testing of RV function by echocardiography. If echocardiogram shows RV dysfunction in the presence of an increased troponin level, this may portend a lethal combination. Such patients should be assessed to determine whether thrombolysis or embolectomy is a clinically appropriate strategy. To our knowledge, however, there are no data on the outcome of patients who are stable with RV enlargement and an increased cTnI, although outcome with cTnT has been evaluated. Even outcome in case series that have included unstable and stable patients with increased levels of cTnI and RV enlargement is limited. Outcome of stable patients with an increased cTnI, irrespective of RV enlargement, is sparse. Therefore, we undertook this investigation to further assess in-hospital mortality of stable patients with PE who have RV enlargement and/or an increase of cTnI.
Methods
This was a retrospective study of patients hospitalized with acute PE who had an evaluation of RV size by echocardiogram or measurement of a cTnI level. Patients were studied from March 2007 through December 2008 at St. Joseph Mercy Oakland Hospital, Pontiac, Michigan, and from January 2004 through June 2008 at William Beaumont Hospital, Royal Oak, Michigan and William Beaumont Hospital, Troy, Michigan. The investigation was approved by the institutional review boards of each hospital. Hospitalized patients with PE were identified by computer listings of International Classification of Disease, Ninth Revision discharge codes (415.11, 415.19 at St. Joseph Mercy Oakland Hospital, and 415.19 at William Beaumont Hospital, Troy and Royal Oak). Medical records, reports of computed tomographic angiograms, ventilation/perfusion lung scans, laboratory data, and reports of echocardiograms were manually reviewed in all patients.
Patients were excluded if in shock (systolic blood pressure <90 mm Hg), were on ventilatory support, or received thrombolytic therapy within 24 hours of hospitalization. Patients were also excluded if they had a possible cause of RV enlargement from an illness other than PE, namely chronic obstructive pulmonary disease or left ventricular (LV) failure, defined as an ejection fraction <40%. Such patients also may have increased levels of cTnI.
PE was diagnosed by computed tomographic angiography in 1,213 patients (95%) and by a high probability interpretation of the ventilation/perfusion lung scan in 60 patients (5%).
Whether the right ventricle was enlarged by echocardiography was determined by a qualitative impression in 92% of patients (832 of 900) who had echocardiograms. RV/LV ratios were measured in 8% (68 of 900). An RV/LV ratio >1 was defied as RV enlargement. Data were obtained from echocardiographic reports. Echocardiograms were not reinterpreted for this investigation.
cTnI was measured by a chemiluminescent assay (Access Immunoassay System, Beckman Coulter, Fullerton, California, at St. Joseph Mercy Oakland Hospital; ADVIA Centaur TnI-Ultra, Deerfield, Illinois, at the William Beaumont Hospitals). At St. Joseph Mercy Oakland Hospital, cTnI was defined as normal if <0.05 ng/ml, intermediate if 0.05 to 0.49 ng/ml, and increased if ≥0.5 ng/ml. At the William Beaumont Hospitals, cTnI was defined as normal if ≤0.05 ng/ml, intermediate if 0.06 to 1.2 ng/ml, and abnormal if >1.2 ng/ml. Before October 2006, at the William Beaumont Hospitals, cTnI was defined as normal if ≤0.3 ng/ml, intermediate if 0.4 to 1.4 ng/ml, and abnormal if ≥1.5 ng/ml. For clarity, we describe “increased” laboratory values reported at St. Joseph Mercy Oakland Hospital and “abnormal” values reported at the William Beaumont Hospitals as “high concentrations.” We refer to any values above normal as increased unless specified as high concentrations.
We attempted to identify all published articles in all languages that reported mortality in stable patients with PE and RV enlargement or increased levels of cTnI. Investigations were identified by searching PubMed through February 2010. Search terms combined with “pulmonary embolism” were “troponin,” “right ventricular hypokinesia,” “dyskinesia,” “right ventricular dyskinesia,” and “right ventricular enlargement.” Manual reference checks of reviews and all original investigations were performed to supplement electronic searches.
Chi-square test was used to assess differences of proportions (InStat 3.0 GraphPad Software, San Diego, California). Odd ratios and 95% confidence intervals (CIs) were calculated using a calculator for CIs of relative risk ( http://www.sign.ac.uk/methodology/risk.xls ).
Results
Data were obtained in 1,273 patients with acute PE treated with anticoagulants. Age was 65 ± 17 years (mean ± SD) and 578 patients (45%) were men.
Echocardiograms were obtained in 900 patients with acute PE. RV enlargement was identified in 26% (237 of 900). In-hospital mortality from acute PE was higher in those with RV enlargement than in those with a normal right ventricle (4.6%, 11 of 237, vs 0.9%, 6 of 663, p = 0.0003; Table 1 ). All-cause mortality was also higher in those with RV enlargement (8.0%, 19 of 237, vs 3.3%, 22 of 663, p = 0.003; Table 2 ). Odds ratio for PE mortality comparing RV enlargement to no RV enlargement was 5.33 (95% CI 1.95 to 14.58) and odds ratio for all-cause mortality was 2.54 (95% CI 1.34 to 4.78).
| PE Death | High Concentrations of cTnI | Intermediate Concentrations of cTnI | Normal Concentrations of cTnI | cTnI Not Done | Total |
|---|---|---|---|---|---|
| Enlarged right ventricle | 1/12 (8.3%) | 6/106 (5.7%) | 2/93 (2.1%) | 2/26 (7.7%) | 11/237 (4.6%) |
| Normal right ventricle | 1/22 (4.5%) | 2/138 (1.4%) | 3/421 (0.7%) | 0/82 | 6/663 (0.9%) |
| Echocardiography not done | 0/6 | 3/46 (6.5%) | 1/321 (0.3%) | 0 | 4/373 (1.1%) |
| Total | 2/40 (5.0%) | 11/290 (3.8%) | 6/835 (0.7%) | 2/108 (1.9%) | 21/1,273 (1.6%) |
| All-Cause Mortality | High Concentrations of cTnI | Intermediate Concentrations of cTnI | Normal Concentrations of cTnI | cTnI Not Done | Total |
|---|---|---|---|---|---|
| Enlarged right ventricle | 2/12 (17%) | 10/106 (9.4%) | 5/93 (5.4%) | 2/26 (7.7%) | 19/237 (8.0%) |
| Normal right ventricle | 2/22 (9.1%) | 10/138 (7.2%) | 8/421 (1.9%) | 2/82 (2.4%) | 22/663 (3.3%) |
| Echocardiography not done | 1/6 (17%) | 3/46 (6.5%) | 2/321 (0.6%) | 0 | 6/373 (1.6%) |
| Total | 5/40 (13%) | 23/290 (7.9%) | 15/835 (1.8%) | 4/108 (3.7%) | 47/1,273 (3.7%) |
Levels of cTnI were obtained in 1,165 patients with acute PE, and increased levels (high concentrations or intermediate) were found in 28% (330). With any increased level of cTnI (high concentrations or intermediate), irrespective of RV enlargement, death from PE occurred in 3.9% (13 of 330) versus 0.7% (6 of 835) of patients with a normal cTnI (p <0.0001; Table 1 ). All-cause mortality with any increased level of cTnI was 8.0% (28 of 330) versus 1.8% (15 of 835) in patients with a normal cTnI (p <0.0001; Table 2 ). In patients with high concentrations of cTnI, death from PE occurred in 5.0% (2 of 40). Of those with an intermediate cTnI, death from PE occurred in 3.8% (11 of 290). All-cause mortality with high concentrations of cTnI was 13% (5 of 40), and with an intermediate cTnI all-cause mortality was 7.9% (23 of 295). Odds ratio for mortality from PE comparing any increased level of cTnI to a normal cTnI was 4.49 (95% CI 1.69 to 11.92) and odds ratio for all cause mortality was 5.09 (95% CI 2.67 to 9.62).
In patients with any increased level of cTnI combined with an enlarged right ventricle, death from PE occurred in 5.9% (7 of 118) compared to 0.7% (3 of 421) with a normal cTnI and normal RV size (p = 0.0009; Table 1 ). All-cause mortality in patients with any increased level of cTnI combined with an enlarged right ventricle was 10% (12 of 118) compared to 1.9% (8 of 421) in patients who had neither (p <0.0001; Table 2 ).
In patients with any increased level of cTnI, death from PE occurred in 5.9% (7 of 118) in those with RV enlargement and 1.9% (3 of 160) in those in whom the right ventricle was not enlarged (p = NS; Figure 1 ). All-cause mortality in those with any increased level of cTnI was 10% (12 of 118) with RV enlargement and 7.5% (12 of 160) without RV enlargement (p = NS; Figure 2 ).
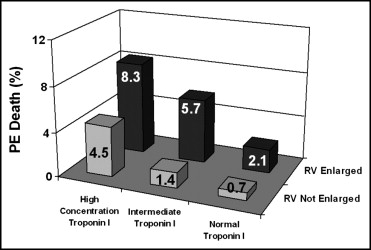
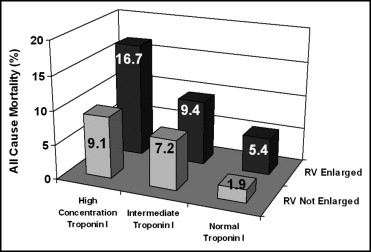
In patients with a normal cTnI, death from PE occurred in 2.1% (2 of 93) of those with RV enlargement and 0.7% (3 of 421) of those in whom the right ventricle was not enlarged (p = NS; Figure 1 ). All-cause mortality in those with a normal cTnI was 5.4% (5 of 93) with RV enlargement and 1.9% (8 of 421) without RV enlargement (p = NS; Figure 2 ).
In patients with an enlarged right ventricle, death from PE occurred in 8.3% (1 of 12) with high concentrations of cTnI, 5.7% (6 of 106) with an intermediate cTnI, and 2.1% (2 of 93) with a normal cTnI (differences between groups not significant; Figure 1 ). All-cause mortality in patients with an enlarged right ventricle occurred in 17% (2 of 12) with high concentrations of cTnI, 9.4% (10 of 106) with an intermediate cTnI, and 5.4% (5 of 93) with a normal cTnI (differences between groups not significant; Figure 2 ).
In patients with a normal RV size, death from PE occurred in 4.5% (1 of 22) with high concentrations of cTnI, 1.4% (2 of 138) with an intermediate concentration of cTnI, and 0.7% (3 of 421) with a normal cTnI (differences between groups not significant; Figure 1 ). All-cause mortality in patients with a normal RV size occurred in 9.1% (2 of 22) with high concentrations of cTnI, 7.2% (10 of 138) with an intermediate cTnI, and 1.9% (8 of 421) with a normal cTnI (high concentrations vs normal, p = 0.03; intermediate vs normal, p = 0.002; Figure 2 ).
Delayed thrombolytic therapy (>24 hours) was administered to 12 patients who survived. Of these 6 had RV enlargement with an intermediate cTnI, 4 had RV enlargement with a normal cTnI, and 2 had a normal cTnI and a normal RV size. Delayed ventilatory support in patients who survived and did not have RV enlargement was administered to 1 patient with high concentrations of cTnI, 3 with an intermediate cTnI, and 3 with a normal cTnI. In addition, delayed ventilatory support in patients in whom RV size was not known was administered to 1 patient with high concentrations of cTnI, 3 with an intermediate cTnI, and 1 with a normal cTnI.
Results
Data were obtained in 1,273 patients with acute PE treated with anticoagulants. Age was 65 ± 17 years (mean ± SD) and 578 patients (45%) were men.
Echocardiograms were obtained in 900 patients with acute PE. RV enlargement was identified in 26% (237 of 900). In-hospital mortality from acute PE was higher in those with RV enlargement than in those with a normal right ventricle (4.6%, 11 of 237, vs 0.9%, 6 of 663, p = 0.0003; Table 1 ). All-cause mortality was also higher in those with RV enlargement (8.0%, 19 of 237, vs 3.3%, 22 of 663, p = 0.003; Table 2 ). Odds ratio for PE mortality comparing RV enlargement to no RV enlargement was 5.33 (95% CI 1.95 to 14.58) and odds ratio for all-cause mortality was 2.54 (95% CI 1.34 to 4.78).



