Other Tests of Lung Mechanics: Resistance and Compliance
The tests described here are usually performed in fully equipped laboratories. In the outpatient setting, they add relatively little to the basic evaluations discussed in previous chapters (spirometry, lung volumes, diffusing capacity, and arterial blood gases). However, these tests might be encountered in either graduate training or in laboratory reports and therefore are considered briefly. In addition, understanding these concepts is important in the management of patients requiring mechanical ventilation.
7A. Resistance
Resistance is the pressure required to produce a flow of 1 L/s into or out of the lung. The units are centimeters of water per liter per second (cm H2O/L/s). This general concept is illustrated in Figure 7-1, in which the pertinent driving pressure (ΔP) is the pressure difference between the ends of the tubes. The pressure required to produce a flow of 1 L/s in a large tube is less than that in a small tube. Hence, the resistance (R) of the small tube is much higher than that of the large tube.
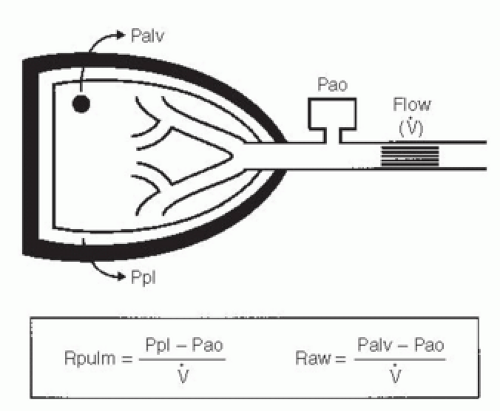
In the lung, measurement of the resistance of the entire system is of interest. Figure 7-2 illustrates how this can be obtained. Flow at the mouth can be measured with a flowmeter. The pressure driving the flow can be measured in either of two ways. Pleural pressure (Ppl) can be measured from a small balloon-catheter unit placed in the lower third of the esophagus and attached to a pressure transducer. Pressure changes in the esophagus have been shown to reflect those in the pleural cavity. The difference between Ppl and Pao (the pressure at the mouth) is the driving pressure, which divided by flow  is defined as the pulmonary resistance (Rpulm). Rpulm includes airway resistance plus a small component due to the resistance of the lung tissue.
is defined as the pulmonary resistance (Rpulm). Rpulm includes airway resistance plus a small component due to the resistance of the lung tissue.
 is defined as the pulmonary resistance (Rpulm). Rpulm includes airway resistance plus a small component due to the resistance of the lung tissue.
is defined as the pulmonary resistance (Rpulm). Rpulm includes airway resistance plus a small component due to the resistance of the lung tissue.The other and much more common resistance measurement is obtained by measuring alveolar pressure (Palv) and relating this to Pao. Palv can be measured in a body plethysmograph and does not require swallowing an esophageal balloon. In this method, the driving pressure is Palv — Pao. This result is divided by flow to determine the airway resistance, Raw. Raw is slightly lower than Rpulm because of the absence of tissue resistance. Both Rpulm and Raw can be measured during either inspiration or expiration, or as an average of both. Figure 7-3 describes how Raw is measured.
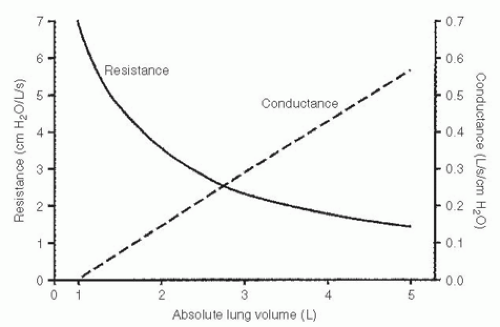
Average resistance in normal adults is 1 to 3 cm H2O/L/s. It is higher in the small lungs of children because the airways are smaller. Occasionally, the
term conductance is used. Conductance is a term borrowed from the electrical engineering field and is the reciprocal of resistance, its units being liters per second per centimeter of water, L/s/cm H2O. Thus, a high resistance means a low conductance—flow is not “conducted” well.
term conductance is used. Conductance is a term borrowed from the electrical engineering field and is the reciprocal of resistance, its units being liters per second per centimeter of water, L/s/cm H2O. Thus, a high resistance means a low conductance—flow is not “conducted” well.
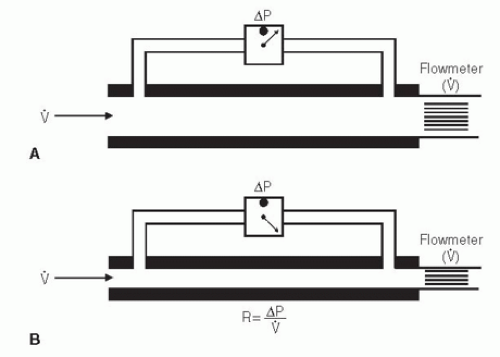 FIG. 7-1. Measurement of resistance (R) through a large tube (A) and small tube (B). Flow (  ) is measured by the flowmeter, and driving pressure (ΔP) is measured by a differential pressure transducer. To drive the same flow, the decrease in pressure is greater in tube (B) and hence the resistance (R) of tube (B) is higher than that of tube (A). ) is measured by the flowmeter, and driving pressure (ΔP) is measured by a differential pressure transducer. To drive the same flow, the decrease in pressure is greater in tube (B) and hence the resistance (R) of tube (B) is higher than that of tube (A). |
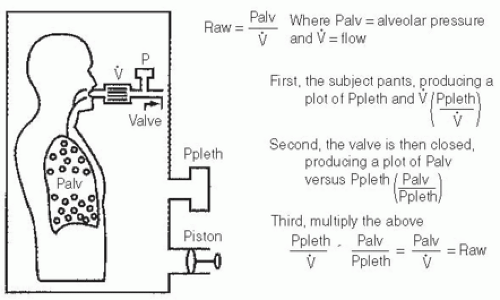 FIG. 7-3. The equipment used to measure lung volume by the body plethysmograph (see Fig. 3-6, page 28) has been modified by inserting a flowmeter between the patient’s mouth and the pressure gauge and valve. The flowmeter measures airflow (  ). The subject is instructed to pant shallowly through the system with the valve open. This provides a measure of plethsymographic pressure as a function of flow, that is, Ppleth/ ). The subject is instructed to pant shallowly through the system with the valve open. This provides a measure of plethsymographic pressure as a function of flow, that is, Ppleth/ . With the subject still panting, the valve is closed. This provides a measure of alveolar pressure as a function of plethysmographic pressure, that is, Palv/Ppleth. As shown, airway resistance (Raw) is obtained by multiplying these two ratios. . With the subject still panting, the valve is closed. This provides a measure of alveolar pressure as a function of plethysmographic pressure, that is, Palv/Ppleth. As shown, airway resistance (Raw) is obtained by multiplying these two ratios. |
Resistance varies inversely with lung volume (Fig. 7-4). At high lung volumes, the airways are wider and the resistance is lower. To standardize for this effect, resistance is typically measured during breathing at functional residual capacity.
Resistance is increased when the airways are narrowed. Narrowing may be due to bronchoconstriction of inflamed airways in asthma, mucus and thickened bronchi in chronic bronchitis, or floppy airways in emphysema.
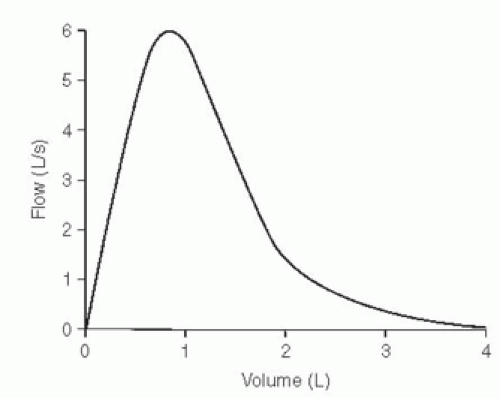
There is a strong negative correlation between resistance and maximal expiratory flow. A high resistance is associated with decreased flows, evidenced by decreases in the forced expiratory volume in 1 second (FEV1) and forced expiratory flow rate over the middle 50% of the forced vital capacity (FEF25-75). There are, however, a few exceptions to this relationship. One is illustrated in Figure 7-5. This type of maximal expiratory flow-volume curve is occasionally seen in the elderly. Resistance in this case is normal, but flow low in the vital capacity, such as the FEF25-75, is decreased. The converse also can occur, namely, normal forced flows and an increased resistance.
PEARL: A patient with a variable obstructing lesion in the extrathoracic trachea (see Fig. 2-7D, page 15) may have a considerable increase in airway resistance but normal maximal expiratory flow. The increased resistance reflects the markedly decreased inspiratory flows caused by the high inspiratory resistance.
7B. Pulmonary Compliance
Compliance is a measure of the lungs’ elasticity. Compliance of the lungs (CL) is defined as the change in lung volume resulting from a change of 1 cm H2O in the elastic pressure of the lungs. Figure 7-6 is similar to Figure 7-2, but a spirometer is added to measure volume (V). When the lung is not moving (that is, airflow is zero), the Ppl is negative (subatmospheric). The lungs are elastic and always tend to collapse. This is resisted by the chest wall, so the Ppl when volume is not changing reflects the static elastic pressure or recoil of the lung at
that volume. If lung volume is increased by a known amount (ΔV) and volume is again held constant, the new Ppl is more negative (the recoil of the lung is greater). This ΔV divided by the difference in the two static Ppl values (ΔPpl) defines the lung compliance, CL = ΔV/ΔPpl (L/cm H2O) at that volume. In addition, it is common practice to measure the elastic recoil pressure with the subject holding his or her breath at total lung capacity (TLC); this is termed the PTLC (recoil pressure at TLC). The measurement of lung compliance requires the introduction of an esophageal balloon (to measure Ppl).
that volume. If lung volume is increased by a known amount (ΔV) and volume is again held constant, the new Ppl is more negative (the recoil of the lung is greater). This ΔV divided by the difference in the two static Ppl values (ΔPpl) defines the lung compliance, CL = ΔV/ΔPpl (L/cm H2O) at that volume. In addition, it is common practice to measure the elastic recoil pressure with the subject holding his or her breath at total lung capacity (TLC); this is termed the PTLC (recoil pressure at TLC). The measurement of lung compliance requires the introduction of an esophageal balloon (to measure Ppl).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree