Other Diastolic and Systolic Sounds
1. What causes an opening snap?
2. How can you differentiate an opening snap from a second or a third heart sound (S2 or S3)?
3. What is the difference between a pulmonic ejection sound and an aortic ejection sound?
4. What is a midsystolic click (MSC)?
5. How can you differentiate an MSC from other heart sounds?
OPENING SNAPS
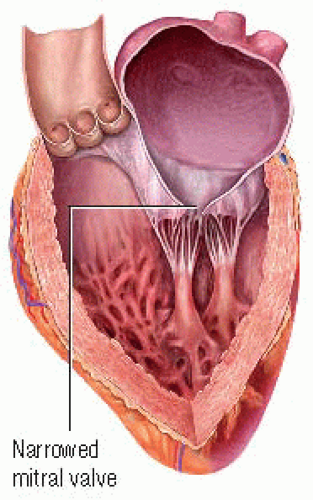
At the end of ventricular systole, the aortic and pulmonic valves close, generating the second heart sound, S2. S2 is followed by a brief period of isovolumic relaxation; during this time, ventricular pressures fall. When ventricular pressures are less than atrial pressures, the mitral and tricuspid valves open. Normally, the opening of these heart valves is inaudible. However, if the mitral valve leaflets become stenotic or abnormally narrowed while remaining somewhat mobile, they create an opening snap (OS). (♦Sound 23) The OS sound is generated by the maximum, but limited, opening of the stenotic leaflets and usually indicates the beginning of the diastolic murmur associated with mitral stenosis. If the mitral valve becomes severely calcified and inflexible, the OS disappears. If the tricuspid valve leaflets become stenotic or abnormally narrowed, an OS can be produced.
Auscultatory area and relationship to ECG
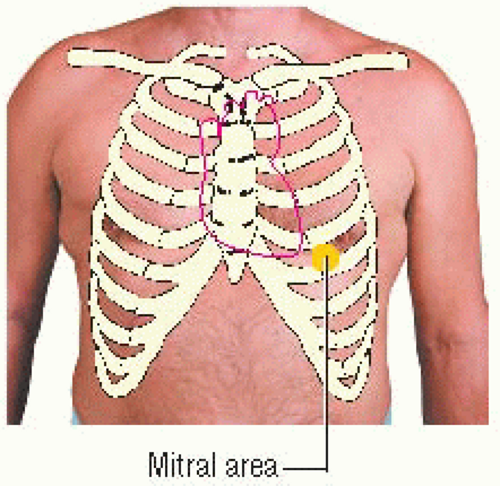
An OS is heard best with the diaphragm of the stethoscope near the heart’s apex over the mitral area or just medial to it, with the patient in the left lateral decubitus position. It’s transmitted widely across the precordium and can typically be heard over the aortic, pulmonic, and tricuspid areas as well. An OS is higher in pitch than S2; it may be as loud as or louder than S2.
An OS occurs early in ventricular diastole; thus, it’s heard just after the T wave in the electrocardiogram (ECG) waveform.
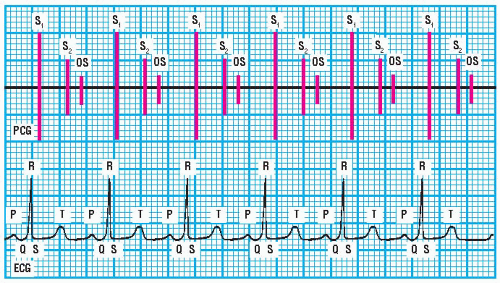 PCG and ECG showing opening snap |
Sound characteristics
The intensity of an OS varies among patients, and it’s usually easy to hear during auscultation. An OS has a short duration. It has a high pitch that’s heard best with the diaphragm of the stethoscope, and a sharp, snaplike quality. Its timing is closely related to S2; an OS occurs early in ventricular diastole, just after the stenotic mitral valve opens. (♦Sound 23)
Differentiating an OS from S2
An OS occurs early in diastole and consequently may be confused with P2 or S3. One characteristic of an OS that helps distinguish it from P2 is its timing: the A2-P2 interval is normally shorter than the A2-OS interval. Also, when the patient stands, the A2-P2 interval narrows, whereas the A2-OS interval widens.
Another characteristic is that the A2-OS interval remains constant throughout respiration, whereas the A2-P2 interval normally widens during inspiration and narrows during expiration. During inspiration, three distinct sounds can usually be heard over the pulmonic area; therefore, the sequence must be A2, P2, OS. In contrast, during expiration, the A2-P2 interval narrows or fuses, forming one sound. This creates an S2-OS interval.
Finally, P2 isn’t usually heard over the mitral area. Therefore, if you hear a split S2 over this area, it may be an S2 and an OS.
Differentiating an OS from S3
Distinguishing an OS from an S3 is difficult in some patients, especially in those with mild mitral stenosis when the A2-OS interval is wider than usual and the OS is somewhat softer. One characteristic of an OS that helps distinguish it from an S3 is its timing: the A2-S3 interval is usually longer than the A2-OS interval. Also, S3 is a low-frequency sound that’s heard best over the mitral area using the bell of the stethoscope. In contrast, an OS produces a high-frequency sound that’s more widely transmitted across the precordium and heard best using the diaphragm of the stethoscope.
Another characteristic of an OS is that its intensity usually isn’t affected by having the patient stand, whereas S2 intensity can be decreased by standing. If the OS is affected, it’s intensified. Finally, if the murmur typically heard in patients with mitral stenosis is present, you can confirm that the sound is an OS.
 AUSCULTATION TIP
AUSCULTATION TIPS3 is usually louder during expiration than during inspiration and is typically palpable; an OS doesn’t vary in intensity with respiration.
SYSTOLIC EJECTION SOUNDS
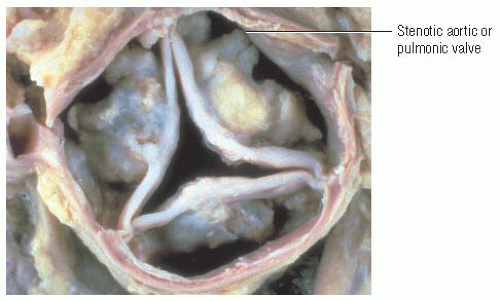
Just as an OS is caused by stenotic mitral valve leaflets, a systolic ejection sound (ES) is caused by the opening of a stenotic aortic or pulmonic valve.
A systolic ES usually occurs early in systole after S1 and isovolumic contraction. It’s commonly associated with ventricular ejection and the maximum opening of a stenotic, yet mobile, aortic or pulmonic valve. If the valve is severely stenotic because of calcification, a systolic ES—like an OS—won’t be produced.
A systolic ES is considered an abnormal condition, regardless of whether it originates on the heart’s right or left side. It may also be caused by the sudden distention of an already dilated aorta or pulmonary artery and by forceful ventricular ejection from pulmonary or systemic hypertension.
Auscultatory area and relationship to ECG
A systolic ES is usually a brief, high-frequency sound that’s heard best using the diaphragm of the stethoscope. It may be heard near the heart’s base over the aortic or pulmonic area, over Erb’s point, or near the apex over the mitral area. A systolic ES occurs just after the QRS complex on the ECG waveform.
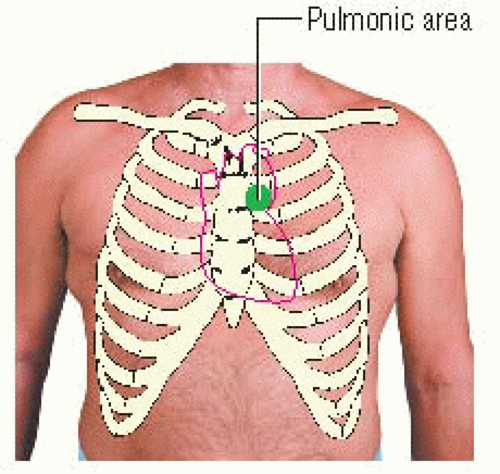
Pulmonic ejection sounds
A pulmonic ejection sound (PES), heard best over the pulmonic area, is the only right-sided heart sound that increases in intensity during expiration and diminishes or disappears during inspiration. (♦Sound 24) In a normal heart, inspiration increases the right ventricular volume, causing the pulmonic valve to dome toward the pulmonary artery, which decreases the sound’s intensity. During expiration, the right ventricular volume is decreased, the valve is less domed, and its opening produces a louder snap. In a patient with pulmonary artery dilation or pulmonary hypertension, a PES may not vary in intensity during respiration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree