by the American Society of Anesthesiologists and the Society of Cardiovascular Anesthesiologists (SCA) recognized two levels of training in perioperative TEE: basic and advanced (4). Anesthesiologists with basic training “should be able to use TEE for indications which lie within the customary practice of anesthesiology,” which include assessment of ventricular function, hemodynamics, cardiovascular collapse, and others. Anesthesiologists with advanced training should be able to utilize the full diagnostic potential of TEE. Clinicians with basic training must recognize their limitations and obtain assistance from expert echocardiographers when needed. When presented with complex diagnostic decisions in the operating room, even anesthesiologists with advanced training may require the assistance of a cardiologist. More recently, these training objectives have been updated and modified to include specific cognitive and technical skills required for the basic and advanced levels (5) (Table 8.1). Most importantly, these training guidelines published jointly by the American Society of Echocardiography and the SCA recommend that 150 TEE examinations be completed under appropriate supervision with at least 50 of them personally performed, interpreted, and reported by the trainee as part of “basic” training. At the advanced level of training, 300 complete examinations under appropriate supervision are recommended with at least 150 of these performed, interpreted, and reported by the trainee.
and chemicals that are used for cleaning and sterilization can damage TEE probes (Table 8.2).
TABLE 8.1. Recommended Training Objectives for Basic and Advanced Perioperative Echocardiography | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 8.2. Procedures and Chemicals That Damage TEE Probes | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
examined in a case series of 7200 cardiac surgical patients (9). No deaths related to intraoperative TEE were reported in this retrospective study. Morbidity occurred in 14 patients (0.2%); severe odynophagia accounted for half of these complications. In two other large series, morbidity was reported in 0.47% of 1500 ambulatory adult patients and 0% of 5016 cardiac surgical patients (10,11). The safety of TEE appears comparable with upper gastrointestinal (UGI) endoscopy (12).
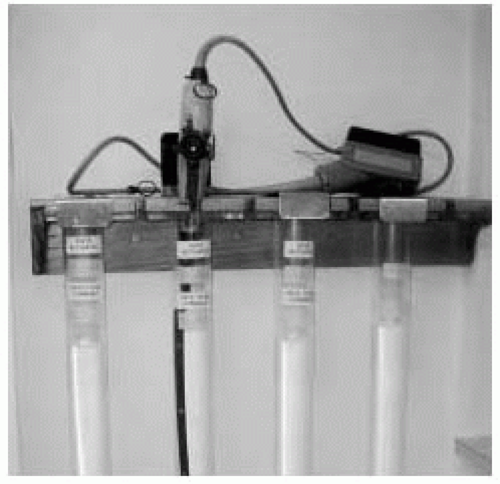 FIGURE 8.2. Example of a wall-mounted rack designed to protect transesophageal echocardiography probes during storage. |
TABLE 8.3. Complications of Intraoperative TEE | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree