Operations on the Supraortic Trunks
The supraaortic trunks may be repaired directly through a trans-sternal approach and remotely through cervical incisions.
TRANS-THORACIC REPAIRS: THE UPPER MIDSTERNOTOMY
The advantages of the upper midsternotomyi over the conventional full sternotomy are straightforward: the lower half of the thorax remains splinted by the intact lower sternum and this decreases postoperative pain (smaller sternal incision and immobility of the sternal edges) and facilitates the mechanics of respiration.
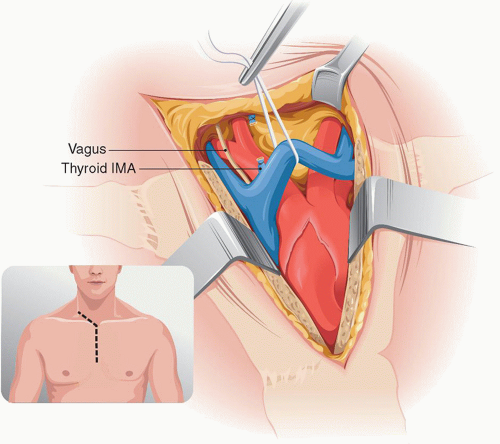
The incision starts with a 1 inch cut along the anterior tendon of the sternomastoid to the suprasternal notch and, from there, it follows the midline of the sternum for three segments (Fig. 4.1). The fibrous ligaments behind the notch are cut. The upper sternum is split with the oscillating saw to the level of T3-T4, at which level the saw is rotated to make a notch on the right half of the sternum without fully dividing it. This notch will result in a subperiosteal fracture when the sternal edges are spread in small steps with a Touffier or a pediatric Finochietto retractor.
The two lightly overlapping lobes of the thymus are separated and the thymic and thyroid ima veins draining into the brachiocephalic vein are divided. The brachiocephalic vein is dissected for 4 cm on both sides of the midline.
As the retractor is gently opened the amount of stretching that is being imposed on the brachiocephalic vein is checked visually and by palpation of the vein. Failure to do so may result in a tear of the junction of the brachiocephalic vein with the superior vena cava, a situation that is awkward to control and repair.
Below the thymus the pericardium is tented upward and opened exposing the ascending aorta. Individual sutures slung over the sternal retractor keep the pericardial edges open. Some of the fat surrounding the ascending aorta is excised to provide a better grip for the partial exclusion clamp later. The intended site for
exclusion clamping is inspected and palpated for the presence of atheroma or calcification (the preoperative CTA should have established the presence of calcification or thrombus at this site).
exclusion clamping is inspected and palpated for the presence of atheroma or calcification (the preoperative CTA should have established the presence of calcification or thrombus at this site).
The dissection proceeds over the trunk of the IA up to its bifurcation into the Rt CCA and SA. In order to expose the full length of the IA, it is necessary to divide the sternothyroid and the sternohyoid muscles. When dissecting the bifurcation of the IA, care is taken to protect the recurrent nerve in two locations: where it hugs the lower wall of the SA origin and where the nerve is close to the posterior wall of the origin of the CCA as it crosses behind it on its medial course toward the thyroid. At this latter, and less publicized, site the recurrent nerve may be injured while circling the origin of the CCA with a right angle clamp.
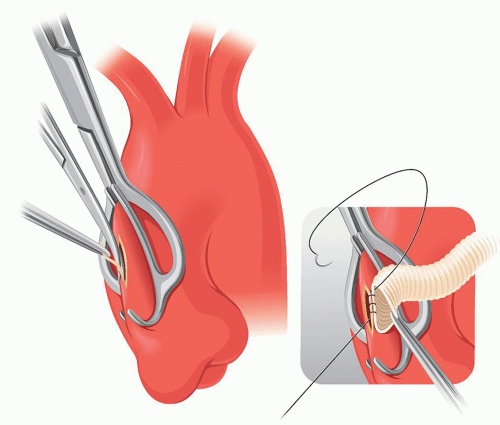
Once the origins of the Rt CCA and Rt SA are isolated one can proceed with partial-exclusion clamping of the ascending aorta1 for the proximal anastomosis of the bypass (Fig. 4.2). Clamping of the ascending aorta is done without heparinizing the patient and having reduced the mean aortic pressure to 80 mmHg. The clamp is a Lemole-Strong, designed in a way that protects the jaws from slipping away from the aorta. The clamp excludes only an edge of aorta large enough to make a safe anastomosis. When the clamp is closed on the aorta attention should be paid to any qualitative or quantitative change in the radial artery waveform signaling a ventricular outflow obstruction caused by too large a bite on the ascending aorta.
The excluded aorta is aspirated with a 19-gauge needle till it puckers to prove the closure of the clamp is complete. The aorta is then opened longitudinally and a small
sliver of wall is removed from one side. The graft selected to replace the IA artery is a #10 tube with its proximal end cut slanted to result in an anastomosis that is tangent to the ascending aorta. It is sutured with 4-0 polypropylene. Prior to tying it, any slack in its loops is corrected tenting them with a fine nerve hook. Before testing the anastomosis, the head of the patient is placed in 15 degrees of Trendelenburg to ensure that any air that could be trapped in the excluded aorta is bled out through the graft and will not escape to the more distal portion of the aortic arch.
sliver of wall is removed from one side. The graft selected to replace the IA artery is a #10 tube with its proximal end cut slanted to result in an anastomosis that is tangent to the ascending aorta. It is sutured with 4-0 polypropylene. Prior to tying it, any slack in its loops is corrected tenting them with a fine nerve hook. Before testing the anastomosis, the head of the patient is placed in 15 degrees of Trendelenburg to ensure that any air that could be trapped in the excluded aorta is bled out through the graft and will not escape to the more distal portion of the aortic arch.
The bypass graft is tended over the brachiocephalic vein into the proximity of the exposed bifurcation of the IA artery. Some descriptions of this technique have placed the IA bypass behind the brachiocephalic vein. That would be acceptable if the bypass had taken origin from the same site as the native IA. But the origin of the bypass is 6 to 7 cm proximal, and anterior to, to that of the IA (Fig. 4.3). A bypass placed under the brachiocephalic vein may compress the latter and itself kink at that level.
For the distal anastomosis, the patient is heparinized and the Rt CCA and the Rt SA are clamped. The IA is clamped in a portion devoid of calcified plaque. The artery is divided 10 mm below its bifurcation where the end of the prosthetic bypass is anastomosed to the distal rim of IA before its bifurcation (Figs. 4.4 and 4.5).
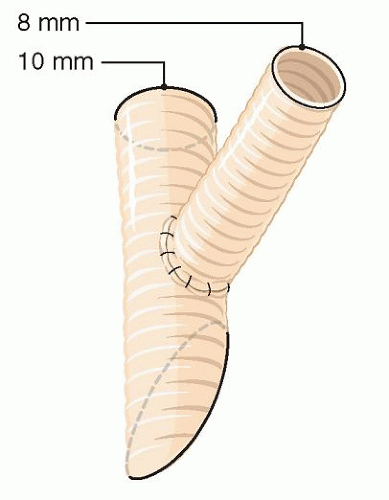
The most common supraaortic reconstruction is an aorto-distal IA bypass with a Lt CCA branch (Fig. 4.6). When a branch is needed to revascularize the left common carotid, a #8 straight graft would have been attached to the left wall of the #10 main graft beforehand. Occasionally, the bypass arising from the ascending aorta needs to reach the carotid bifurcation in one or both sides.
The choice of a #10 prosthesis for the ascending aorta-IA bypass with a #8 side branch to the Lt CCA (Fig. 4.7) is better than to use a commercial bifurcation graft,
as some have recommended. If a standard bifurcation graft were to be used, it would have a #16 trunk with limbs of 8 mm in diameter in order to match the diameter of the CCA. The slanted shape to which the proximal end of the #16 mm graft must be shaped to achieve a tangential anastomosis with the ascending aorta would result in a large perimeter anastomosis that requires a considerably larger opening in the aorta,
hence, a greater exclusion clamping of the ascending aorta. Furthermore, the bulk of the pressurized trunk of a #16 mm graft in the anterior mediastinum may actually either compress the brachiocephalic vein or be compressed itself by the sternum.
as some have recommended. If a standard bifurcation graft were to be used, it would have a #16 trunk with limbs of 8 mm in diameter in order to match the diameter of the CCA. The slanted shape to which the proximal end of the #16 mm graft must be shaped to achieve a tangential anastomosis with the ascending aorta would result in a large perimeter anastomosis that requires a considerably larger opening in the aorta,
hence, a greater exclusion clamping of the ascending aorta. Furthermore, the bulk of the pressurized trunk of a #16 mm graft in the anterior mediastinum may actually either compress the brachiocephalic vein or be compressed itself by the sternum.
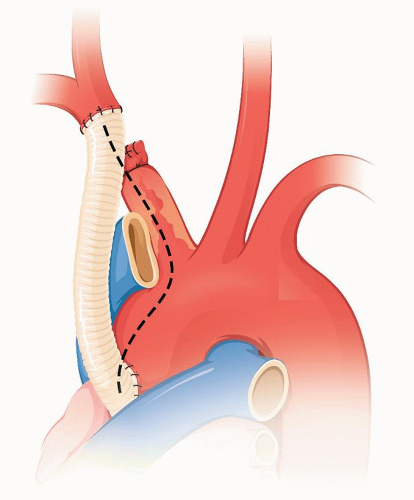 FIGURE 4.3. Schematic showing that for the bypass graft to have a straight and unimpeded course it must be placed in front of the brachiocephalic vein. |
 FIGURE 4.4. A completed aorto-distal IA bypass. |
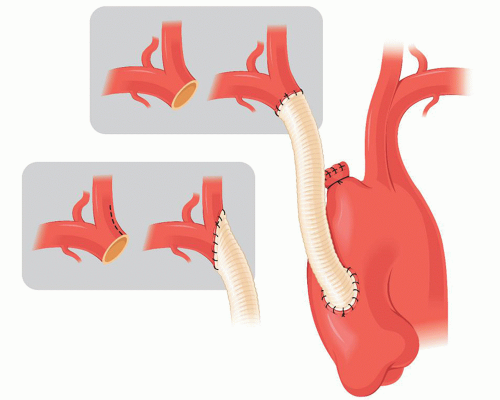 FIGURE 4.5. The distal anastomosis is fashioned extending it to the artery that bears the heaviest burden of plaque. |
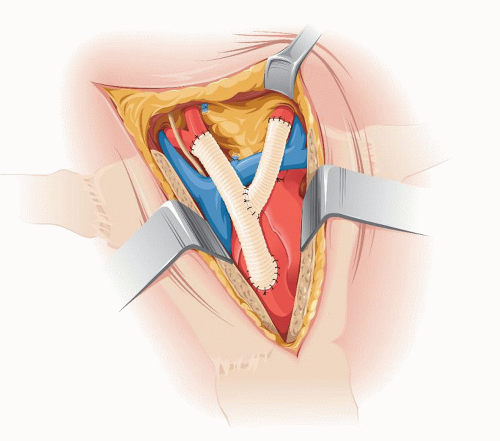 FIGURE 4.6. The most frequent arrangement: aorto-IA-Lt CCA bypass through an upper sternotomy. |
Another reason to prefer the #10/#8 configuration is better conditions for flow and more physical similarity with human geometry. From a mechanics point of view, the ideal area ratio for an arterial bifurcation is 1.16. The area ratio of a #10 tube with a #8 side branch is 1.64. In contrast a #16 × 8 commercial bifurcated graft has an area ratio of 4.61. This will result in a pressure drop at the bifurcation of the prosthesis and will cause a high percentage of wave reflection. I do not know if these disturbed flow circumstances have any impact on outcomes but I suspect they will not be better than those obtained with the smaller and more physiologic configuration of 10 + 8, described above.
If the distal anastomosis of either branch is to be made at the carotid bifurcation, the most efficient way is to divide the CCA 3 mm below the flow divider. If a concomitant endarterectomy is indicated a Type 2 eversion is done and the graft is anastomosed end-to-end to the bifurcation (Fig. 4.8). The stump of the IA is closed with a continuous 4-0 suture between pledgets.