Fig. 28.1
A 45-year-old woman with celiac compression identified on CTA and a 25-lb weight loss with abdominal and back pain. (a) The crus of the diaphragm (arrow) is dissected and the ganglion fibers isolated with a right-angle clamp. (b) The ganglion fibers are divided with electrocautery. (c) The ganglion fibers retract and are excised along with the diaphragmatic fibers. (d) The origin of the celiac artery is freed of all surrounding tissue (arrow) and assessed by palpation and ultrasound exam
Most authors agree that after the celiac artery is inspected and patency assessed, ideally with palpation, Doppler exam, and ultrasound, a decision is made whether celiac artery reconstruction is indicated. Reilly et al recommend celiac reconstruction for all patients with a visible celiac artery deformity, thrill, or pressure gradient [1]. At our institution, all patients undergo intraoperative ultrasound (Fig. 28.2a–c) after open MAL resection, with ~40 % demonstrating residual celiac stenosis despite adequate MAL release [2]. Depending on the length of the stenotic lesion and the proximity to the aorta, either patch angioplasty (bovine pericardium or polyester graft patch) or aortoceliac bypass is recommended. In our early series, patients also had intraluminal dilation but this technique was abandoned due to less favorable success rates. In addition, because of the elongation of the celiac artery in some cases, primary reanastomoses has also been reported.
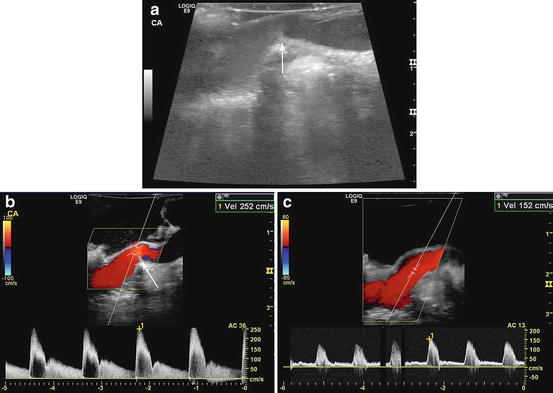
Fig. 28.2
After MAL release in a 37-year-old woman, intraoperative duplex identified a fixed stenosis (arrow) arising from the posterior wall of the celiac artery. (a) Gray-scale images identified the stenosis. (b) Color flow Doppler confirmed the site of stenosis (arrow) with a peak systolic velocity of 252 cm/s. (c) Because of a diminished pulse, the patient underwent a patch angioplasty with bovine pericardium resulting in improvement of the stenosis and improvement of the peak systolic velocity to 152 cm/s
Ganglion Resection
Many authors believe the celiac ganglion resection is the more critical component of the procedure. The ganglion can often be more easily visualized if the percutaneous ganglion injections have been done within 72 h. In our series of five patients with aortoceliac bypass, one had persistent symptoms with a widely patient graft, emphasizing the role of the ganglion in the pain of MALS. In addition, of the 32 patients, 4 had recurrent symptoms, but only 1 of the 4 had recurrent celiac artery stenosis.
Role of Endovascular Treatment
Percutaneous treatment of MALS was first described decades ago to treat recurrent stenosis after open MAL release [5]. However, primary treatment of celiac artery compression either by MAL or an occult malignancy with angioplasty has a high failure rate [6]. Several case reports [6–8] suggest that angioplasty alone, without the preceding removal of the MAL and ganglion fibers, will not be successful. In addition, stents used in a primary fashion are at risk of fracture due to external compression. However, angioplasty can be used to good effect for celiac artery restenosis after MAL release and/or celiac artery bypass or patch angioplasty [5, 9].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


