INDICATIONS/CONTRAINDICATIONS
Indications
Middle lobectomy is indicated for pathologic changes involving the middle lobe. This includes mainly malignancies of the lung like primary lung cancer or lung metastases from extrapulmonary tumors. Bronchiectasis, middle lobe syndrome, and bullous changes of the middle lobe or large hamartochondroma are benign changes that justify middle lobe resection. Removal of the middle lobe is the least common resection of all pulmonary lobes. Only approximately 6% of lung cancer originates from the middle lobe.
Complete resection of the middle lobe with additional systematic lymphadenectomy is the treatment of choice for lung cancer limited to segment 4 and 5. However, in the presence of central tumor growth or tumor invasion of the upper vein, upper bilobectomy becomes necessary. Mostly, the middle lobe vein originates from the upper vein; therefore, separation of these two veins is often difficult or even impossible when attempting R0 resection in malignant disease.
Sometimes tumors in the upper or the lower lobe invade the interlobium thereby infiltrating the middle lobe. In these cases an upper or lower bilobectomy (upper or lower lobe as well as the middle lobe) is indicated. The same holds true in case of infiltration of the interlobar artery in lower lobe tumors or lesions at the origin of the lower lobe bronchus, because the middle lobe bronchus is often located just opposite of the bronchus of segment 6 (apical segment of lower lobe).
Neoadjuvant therapy may decrease the size of a tumor which then can be removed as middle lobectomy instead of more extensive resection. Neoadjuvant therapy is also indicated in case of operable patients if lymph node involvement is proven (N2 disease).
Besides surgical management of middle lobe malignancies, radio- or chemotherapy are nowadays accepted alternative treatment strategies in evidence-based medicine.
Placement of stents in an occluding tumor is rarely indicated as the middle lobe bronchus is very small and difficult to be stented.
The so-called “middle lobe syndrome” is a problem of recurrent infection of the middle lobe resulting in local lymph node swelling (around the middle lobe bronchus) that leads to further occlusion of the middle lobe and subsequent retention of secretions. The aetiology of the middle lobe syndrome could be infectious disease (i.e., granulomatous, tuberculosis) but often it remains unclear; sometimes a long and small middle lobe bronchus may be the cause of this syndrome.
Contraindications
As the middle lobe is the smallest lobe, resection seldom results in severely impaired lung function. However, because the risk of pneumonectomy is relevant (see Complications), an alternative treatment to surgery should be chosen if the patient is potentially inoperable in view of lung function or general condition.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
In case of pulmonary nodules, suspicious for malignancy (size, margins, radiologic pattern, growth), an attempt should be made to achieve histology prior to surgery.
Bronchoscopy with transbronchial biopsies is the least invasive procedure to gain samples for histologic examination. Furthermore, the investigation discloses endobronchial tumor growth and defines resection margins. Extensive resections like sleeve resections or bilobectomy are indicated in cases of endobronchial tumor growth in the intermediate bronchus.
In addition, bronchoscopy offers the option to achieve microbiologic specimen, especially if infection is part of the tumor problem or if the lesion is thought to be rather of infectious than malignant origin. Accordingly, antibiotic treatment and inhalation therapy should be initiated and hence the patient’s condition optimized for surgery.
If bronchoscopy does not reveal the etiology of the lesion, CT-guided needle biopsy is recommended.
Prior to surgery examination of the functional status, that is, lung function tests, diffusion capacity testing, blood gas analysis, ECG, etc. according to guidelines should be performed.
Nowadays all patients have CT scans prior to surgery; this should be done with contrast agent to allow separation of pulmonary vessels from lymph nodes on CT scans. In case of malignancy most patients will receive FDG-PET/CT as well.
It is important that the surgeon studies the CT scan and is familiar with the specific anatomy of the patient prior to surgery.
Positioning
Middle lobectomy can be performed as open (thoracotomy) or as thoracoscopic procedure (video-assisted thoracoscopic surgery [VATS]). For anterolateral thoracotomy, the patient is placed in the lateral position with the operated side upward and the table slightly turned backward. The arms are positioned in forward elevation. The surgeon stands anteriorly and the assistant posteriorly to the patient. For posterolateral thoracotomy, the patient is slightly turned forward exposing scapula and spine. The surgeon stands posteriorly and the assistant anteriorly to the patient. In VATS we prefer the anterior approach as the intercostal spaces are wider in the anterior than in the posterior part and less musculature overlaps the ribs. Both, surgeon and assistant, stand anteriorly with the video monitor placed opposite of them. The patient is intubated which allows single-lung ventilation of the nonoperated side.
The patient is secured to the operative table with one safety strap over the hips and pads posteriorly at the lower spine and the upper thoracic spine and anteriorly to the pubic bone. The upper part of the body is stabilized anteriorly by placing the arms on well-padded boards in forward position. From the spine to the sternum the whole thorax is prepped with a chlorhexidine–alcohol solution including also the axilla and upper part of the upper arm.
 SURGERY
SURGERY
Technique
The following description will be detailed for the open approach but it is basically true for the thoracoscopic approach as well. When performing the procedure by VATS one should have a low threshold to convert to the open technique in cases of impaired visualization or complications. Because the vessels to the middle lobe come from the interlobar artery and drain into the upper pulmonary vein respectively, insufficient visualization may lead to accidental transection or disrupture of vessels of the upper or lower lobe. This would result in additional lobectomy, in the worst case even in right-sided pneumonectomy.
We prefer anterolateral approach for thoracotomy as all important structures are located ventrally. The incision is carried out through the subcutaneous tissue and the musculature of the thoracic wall (M. serratus ant.) is spread. The latissimus dorsi muscle as well as the pectoralis major muscle is kept intact. Along the upper rim of the fourth or fifth rib the intercostal muscles are divided until the thoracic cavity is entered. A self-retaining retractor is inserted. Inspection for adhesions (often encountered in patients with bronchiectasis) or any intrapleural pathology is performed and the lobes are explored. The major fissure often is well developed allowing separation of the lower and middle lobe whereas the minor fissure (between the upper and middle lobe) shows broad parenchymal bridging in many cases. Inspection also includes the lymph node stations before it can be determined whether pathology is resectable.
Hilar Dissection
Dissection starts at the anterior hilum by incision of the mediastinal pleura. To do so, the lung is pushed dorsally and held in this position either with a sponge stick or a parenchymal clamp (i.e., Duval lung forceps). This maneuvre exposes the anterior hilum with the vessels, fatty tissue, lymph nodes (station 10), and phrenic nerve. Care has to be taken to prevent harm to the phrenic nerve which lies close to the hilar vessels and may be buried in fatty tissue. There are always small vessels accompanying the nerve longitudinally which are better visible than the nerve itself (Fig. 11.1). The pleura overlying the pulmonary vessels is grasped with DeBakey forceps and incised perpendicular to the axis of the vein with electrocautery or Metzenbaum scissors (Fig. 11.2). Preparation of vessels is performed until the vessel wall is bare. The upper pulmonary vein is the first vessel encountered as it partially overlaps the mainstem of the pulmonary artery (Fig. 11.3).
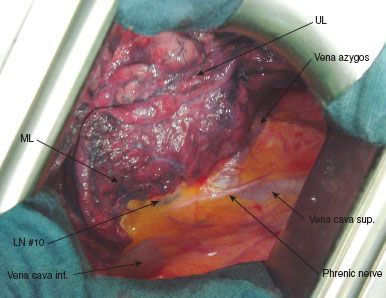
Figure 11.1 Situs with anterior hilum: Mediastinal pleura overlying the vascular structures. Phrenic nerve, vena cava, and azygos vein clearly visible.
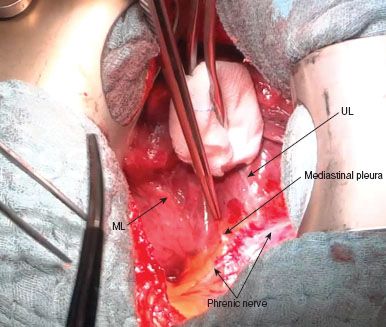
Figure 11.2 Grasping of the mediastinal pleura for incision. Upper lobe is pushed dorsally.
Dissection of Veins
Dissection is started at the upper pulmonary vein with exposure of the branches to the middle lobe and those to the upper lobe. A small sponge stick is used for blunt dissection of surrounding tissue from the vessel wall. Mobilization of the different veins is facilitated by pushing toward the lung parenchyma. The branching of the pulmonary vein becomes visible, allowing identification of the parts to the middle and upper lobe (Fig. 11.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


