Fig. 17.1
Sample images of the ascending aorta. (a) is a simple CT image, (b) shows contrast-enhanced CT, and (c) shows epiaortic ultrasound echography image
Aortic side clamping has been routinely used for proximal anastomosis, even for SVG, radial artery, or free arterial graft. The aortic side clamp deforms, distorts, and compresses the ascending aorta, which might crush the plaque and result in embolization, depending on the characteristics of the aorta. Lev-Ran et al. reported the usage of partial clamping as a risk factor for postoperative cerebral infarction [7]. Edelman et al. reported that postoperative cerebral infarction was observed significantly more often in a clamp group than in a clampless group [8]. On the other hand, Yamaguchi reported that if intraoperative ultrasonography showed no plaque on the ascending aorta, no significant difference in risk of postoperative cerebral infarction existed between clamp and clampless groups [9]. In Japan, intraoperative epiaortic ultrasonography is recommended and used by many surgeons.
The ascending aorta is usually used as the site of proximal anastomosis. Brachiocephalic artery and ITA graft for Y-shaped or I-shaped grafts or aortocoronary bypass graft (SVG or RA) as Y-shaped graft are other options. An I-shaped graft might sacrifice the capacity for long-term patency of the ITA graft, while a Y-shaped graft requires careful consideration about the blood contributions of each branch to avoid steal phenomenon or string sign [10].
17.2 Simple Aortic Side Clamp
The aortic side partial clamp is usually placed after finishing the distal coronary artery anastomosis and aortic declamping with heart beating. The partial clamp is placed on the anterior face of the ascending aorta, and a hole is made with a puncher following a small cut with a spit knife on the ridge of the partially clamped aorta to avoid aorta injury. Anastomosis for the circumflex artery should be made slightly toward the left side of the wall to create proximal anastomosis rising from the ascending aorta. Proximal anastomosis can be set on the anterior aspect, making the graft run parallel to the aorta, or it can pass down toward the right-sided space of the right atrium. The size of the puncher is usually 4.5 mm for vein grafts and 3.5 mm for free ITA graft or radial artery graft. A hole that is too big for the graft risks stenosis at the heel side and excessive tension on the graft on the toe side. Blood pressure should be kept low by lowering the perfusion flow when using a heart-lung machine or by administration of vasodilator to avoid aortic injury or dissection. At the same time, compression on the carotid arteries by the anesthesiologist might help debris from the clamp side escape to proceed into the arch branches.
17.3 Selection of Proximal Anastomosis Techniques
The aorta no-touch technique might carry a low risk of cerebral embolization for patients with some degree of atherosclerosis on the aorta. Some surgeons have recommended the usage of anastomosis devices [11–13, 17–19, 22–25]. However, should these aorta no-touch techniques or anastomosis devices be used in all patients? Is there any evidence that these techniques make any difference regarding cerebral infarction in patients with a normal aorta? Yamaguchi reported that when intraoperative epiaortic ultrasonography showed no atherosclerotic change on the ascending aorta, simple aortic side clamping was not associated with any significant increase in cerebral infarctions [9]. However, presence of some degree of atherosclerotic change, fragile plaque, thickening, or debris should be taken into consideration and other techniques applied to avoid manipulation of the aorta.
17.4 Symmetry Aortic Connector (St. Jude Medical, Minneapolis, MN)
As the first device for proximal anastomosis available in Japan, the aortic connector was introduced in 2002. Results of short- and long-term studies on patency rates for this device are ambiguous [11–13]. Farhat reported histological damage to saphenous vein grafts with this device [14], which was withdrawn from use in Japan in 2006.
17.5 PAS-Port System (Cardiac, Menlo Park, CA)
The PAS-Port system was introduced in 2004 in Japan and has been used under specific conditions. It can be used for cases showing severe atherosclerosis on the ascending aorta with one spot where the aortic wall is suitably thin and smooth. The stent anchoring the vein graft to the aorta is placed external to graft, whereas the stent was inside the vein graft in the symmetry aortic connector. Although Izutani reported one case of ostial stenosis at 4 months postoperatively [15], this structure may decrease the possibility of thrombosis inside the graft and is morphologically acceptable according to Kawasaki [16]. Many groups have reported better results after clampless OPCAB using the PAS-Port system compared with conventional CABG [17–19] (Fig. 17.2).
These two anastomosis devices allowed automatic connection of the grafts on the aorta. However, some concerns have been raised regarding the quality of anastomosis, due to the need for metal stents for anchoring. The following are two new anastomosis devices that enable hand-sewn anastomosis:
17.6 Heartstring System (MAQUET, San Jose, CA)
The Heartstring was introduced to Japan in 2003. A hole is made with the original punch, then pressure is placed over the hole with a finger to stop the bleeding, and the sealing umbrella is inserted into the aorta. Hemostasis is achieved by blood pressure pushing the umbrella against the aorta wall [20]. Once hemostasis is obtained, anastomosis can be completed with a standard hand-sewn technique not only for the saphenous vein but also for radial artery grafts. After completing hand-sewn sutures, the sealing string comes out of the suture line as a single string. Sometimes bleeding cannot be completely controlled, but in such cases, use of the blower helps to make the hole bloodless. Thourani reported the Heartstring proximal anastomotic device could be safely used with all grades of aortic atherosclerosis, especially with moderately diseased aorta [21]. Stroke has been reported to occur with usage of this device in OPCAB [22–25] (Fig. 17.3).


Fig. 17.3
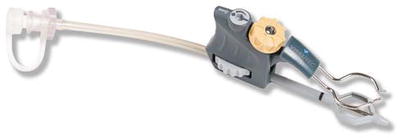
17.7 Enclose II System (Novare Surgical Systems, Cupertino, CA)
This is another manual proximal anastomosis device that enables the surgeon to perform proximal hand-sewn anastomosis without side clamping. The lower jaw of the device is inserted into the aorta through a small hole made by a 14-G needle 2 cm above the anastomosis point. The jaw is advanced toward the point of anastomosis. The membrane of the lower jaw is opened, and the upper jaw is lowered toward the aortic wall to compress the lower jaw onto the inside of the aorta. A small incision is made in the aorta and excess aortic tissue is removed using the 3.5-mm aortic punch. Proximal anastomosis can be performed in the usual fashion. An overly deep bite might tear the membrane. After the first anastomosis is finished, the device can be repositioned for the next. This technique is not a real aorta no-touch technique. Care should be taken to avoid atherosclerotic sites for the needle hole or anastomosis position using epiaortic ultrasonography. Many reports have shown good results using this device, which is popular in Japan [25–28] (Fig. 17.4).