Purpose
Although sleep deprivation (SD) affects cardiovascular system in many ways, physio-pathological changes in cardiac chamber volume and function have not been well described. Three-dimensional (3D) echocardiography has major advantages in evaluation of volumes and phasic changes independent from any geometrical assumption. The aim our study was to investigate the effect of SD on left atrial (LA) and ventricular function by 3D echocardiography.
Methods
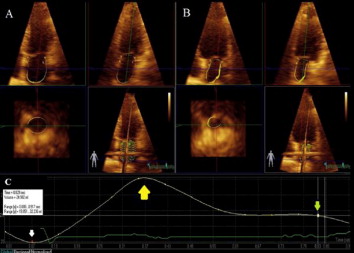
Thirty-two healthy individuals (12 female, mean age 33.25 ± 8.18) were evaluated. Echocardiographic examination performed once after a night of regular sleep and a night of sleep debt. Beside conventional parameters, 3D phasic volumes and function measured using a commercially available 3D echocardiography system and off-line analysis software.
Methods
Thirty-two healthy individuals (12 female, mean age 33.25 ± 8.18) were evaluated. Echocardiographic examination performed once after a night of regular sleep and a night of sleep debt. Beside conventional parameters, 3D phasic volumes and function measured using a commercially available 3D echocardiography system and off-line analysis software.
Results
Mean daily sleep duration of the study group was 8.15 ± 2.19 hours in the day of regular sleep and 2.56 ± 2.25 hours in the day of sleep deprivation. Among the conventional Doppler parameters, mitral early diastolic inflow’s (E) deceleration time (166.44 ± 26.12 vs 180.83; %95CI 0.41-28.36; p= 0.044) and proportion to early diastolic anular velocity (E’) (6.38 ± 0.85 vs 6.95 ± 1.26; %95 CI (-1.06) – (-0.04)); p=0.005) derived by Doppler tissue imaging were significantly increased after night shift. Among 3D measurements, the difference in left ventricular (LV) ejection fraction (EF), LA EF, LA reservoir function and LA active EF were not significant. Left atrial passive EF of the individuals after night shift was significantly lower (31.49 ± 7.75 vs 24.10 ± 7.66; %95CI 2.35 – 12.43; p= 0.006).
Conclusion
Acute SD is associated with a reduction in LA passive emptying function in healthy adults. Although entire conventional indices of diastolic function did not support, 3D derived indices were sufficient to show subclinical diastolic dysfunction according to impairment in passive phase of left atrial ejection. Prospective large scale studies needed to enlight this issue.