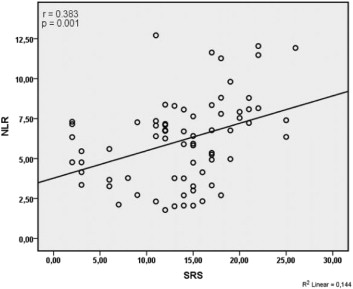
The neutrophil–lymphocyte ratio (NLR) is an inflammatory marker of adverse cardiac events in STEMI. Whether admission NLRs before a successful primary percutaneous coronary intervention (PCI) directly reflect a larger myocardial infarct size and left ventricular impairment is not enough known. The aim of this study was to assess the relationship between NLR levels and myocardial infarct size, left ventricular function and clinical outcomes after PCI in STEMI patients. The 72 patients recruited for the present study were admitted in the period between 01 September, 2012 and 01 May, 2013 at Atatürk University Cardiology Department, Erzurum, Turkey). The patients, who had first anterior STEMI within 6 hours after the onset of symptoms, were successfully reperfused with primary PCI; were evaluated according to the thrombolysis in myocardial ınfarction classification (21), with the infarct-related vessel as the only proximal left anterior descending artery; and were then referred to a nuclear medicine laboratory for the assessment of myocardial perfusion defects before hospital discharge, using the resting gated SPECT MPI with technetium Tc 99m sestamibi. The related analyzes were carried out by virtue of SPSS software (Version 18.0, SPSS Chicago, USA). For the continuous data, the differences between normally distributed numeric variables were evaluated using Student-t test analysis of variance, while non-normally distributed variables were analyzed using Mann-Whitney U test analysis of variance as appropriate. The relationship of infarct size and the NLR levels is presented graphically using Pearson’s correlation. Patients were divided into equal tertiles according to admission NLR levels. The summed rest scores, number of infarcted segments and infarct size ratio were significantly increased in the higher NLR group (15.6 ± 5.6 vs. 11.9 ± 5.7, p= 0.006; 6.4 ± 1.4 vs. 5.36 ± 1.9, p= 0.016; 33.9 ± 16.0 vs. 23.4 ± 10.2; p=0.001, respectively). The higher NLR group has lower LVEF (46.0 ± 7.9 vs. 40.8 ± 10.9; p= 0.024). The higher NLRs were associated with the adverse clinical outcomes [10 (28%) vs. 2 (5%); p= 0.012]. In conclusion, the NLR can be measured upon admission of patients with STEMI to identify patients with increased risk of developing a larger myocardial infarction and increased heart failure. Therefore, the NLR is useful biomarker for determining which patients may show poor prognosis after successful revascularization. We believe that this information will be useful in the risk evaluation of STEMI patients treated with primary PCI.