Chapter 60 Obstructive Sleep Apnea
Epidemiology, Risk Factors, and Pathophysiology
Epidemiology
Although obstructive sleep apnea clearly is a common disorder within the general population, its incidence is hard to establish, because methodologic differences among the various epidemiologic studies have made comparisons difficult. First, different tests have been used to diagnose OSA. Overnight polysomnography (PSG) is considered the “gold standard” diagnostic modality, but assessments have been made using other tests instead, such as unattended in-home PSG or respiratory polygraphy, pulse oximetry, and even clinical questionnaires (see Chapter 61). Second, variability in the definitions of different respiratory events (especially hypopnea) and the apnea-hypopnea index (AHI) cutoff value that defines OSA, or clinically significant OSA, is well recognized. In this sense, the chosen oxyhemoglobin desaturation threshold, typically 3% or 4%, used to define hypopnea can lead to different AHI scores; accordingly, estimates of disease severity will vary. Third, differences in sampling of populations (for example, the percentages of elderly and female subjects included) have been noted. Fourth, disparities in signal processing and a lack of standardization in the quantification of airflow (including thermistor, inductance plethysmography, and nasal cannula–pressure transduction) are common. Finally, the quality of validation of equipment and the conclusions of some studies have been questioned because of methodologic limitations such as small sample sizes or inadequate controls for potential confounding variables.
Middle-Aged Population
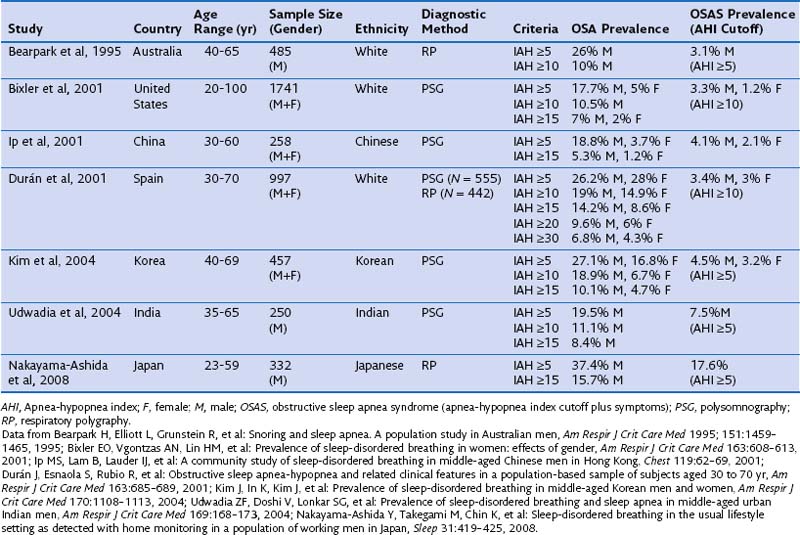
It is estimated that 24% of men and 9% of women have OSA, as defined by an AHI of 5 or greater, and that 15% of men and 5% of women between 30 and 60 years have an AHI of 10 or higher. With use of daytime sleepiness as a clinical syndrome, the prevalence ranges between 3% and 7% in men and 2% and 5% in women in the general population (Box 60-1). Until recently, population-based epidemiologic studies of OSA were available only for North America, Europe, and Australia. However, more recent studies undertaken in other countries, including China, India, and Korea, report similar prevalence rates. The overall incidence of moderate to severe OSA (defined by an AHI of 15 or higher) occurring over a 5-year period is 11% and 5% in men and in women, respectively, which persists even after adjustment for confounding variables. This means that, even in the absence of any weight change, approximately 20% of men and 10% of women will develop moderate to severe OSA in that period of time.
Box 60-1
Epidemiologic Features of Obstructive Sleep Apnea (OSA)
• 24% of men and 9% of women have OSA.
• 3% to 7% men and 2% to 5% women have OSA syndrome.
• 65% of older men and 56% of older women have OSA.
• 20% of older men and 15% of older women have OSA syndrome.
• In postmenopausal status, women reach similar incidence rates of OSA than men.
• The overall 5-year incidence of moderate to severe OSA ranges between 5% and 11%.
• Referral to sleep centers for further investigation is four- to eight times more frequent in men than in women.
Most population-based studies have found a two- to three-fold higher prevalence of OSA in males than in females. The ratio is even higher for men treated in sleep centers, with reported ratios between 4 : 1 and 8 : 1 or higher. This higher ratio may be the result of multiple factors: Women do not show the “classic” OSA symptomatology—they typically have more comorbid illnesses, use more psychoactive drugs in the absence of a correct diagnosis, and often present with vague, nonspecific symptoms, which widens the differential diagnosis and leads to a higher level of underdiagnosis or misdiagnosis of OSA. An important finding from epidemiologic studies is that gender disparities in prevalence seem to decrease with age, and when women reach postmenopausal status (and are not receiving hormonal replacement treatment), incidence rates for men and women become similar. Table 60-1 summarizes the most important sleep apnea prevalence studies in middle-aged populations.
Elderly Population
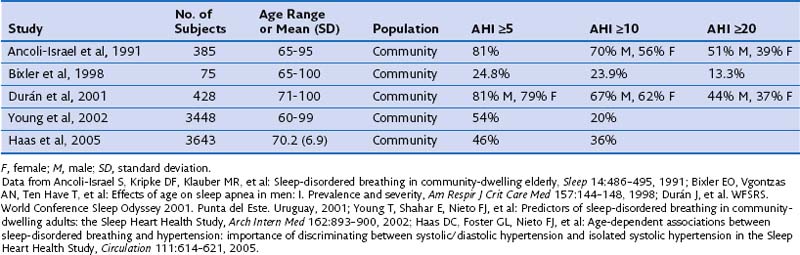
In any case, the two proposed types of OSA consist of (1) a pathologic form of OSA that appears in middle age in those patients who usually are diagnosed in sleep laboratories and (2) OSA that appears after the age of 60 years, with some overlap between the two, mainly caused by physiologic changes (increase in pharyngeal collapsibility) associated with aging, and of less clinical importance. Data also suggest that the interaction between body weight and OSA in elderly persons may be different from that in younger adults. Because of the population-wide increase in longevity, the proportion of elderly persons being treated at sleep units also is increasing; currently one in four sleep studies are performed in patients older than 65 years of age. This scenario will present a scientific challenge in the future, in view of the lack of scientific evidence available on OSA in the elderly. Table 60-2 summarizes the most important epidemiologic studies describing the prevalence of OSA in older people.