Obstructive disorders
Among chronic obstructive disorders of the lung, chronic obstructive pulmonary disease (COPD), also called chronic obstructive lung disorder, is the most common. It affects an estimated 30 million Americans and its numbers are rising.
Early COPD may not produce symptoms and may cause only minimal disability in many patients, but it tends to worsen with time.
Types of COPD include chronic bronchitis, cystic fibrosis, emphysema and, more commonly, a combination of these conditions (usually bronchitis and emphysema).
CHRONIC BRONCHITIS
Bronchitis is acute or chronic inflammation of the bronchi caused by irritants or infection. The distinguishing characteristic of bronchitis is obstruction of airflow. In chronic bronchitis, a form of chronic obstructive pulmonary disease, hypersecretion of mucus and chronic productive cough are present during 3 months of the year for at least 2 consecutive years.
Pathophysiology
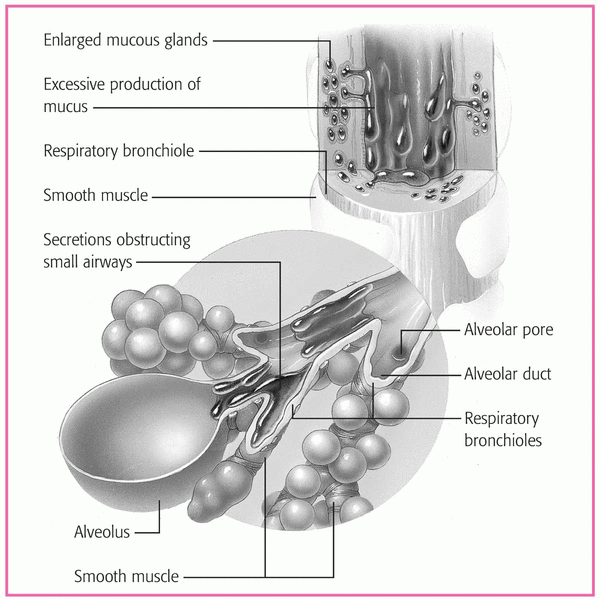
Chronic bronchitis develops when irritants are inhaled for a prolonged period. The irritants inflame the tracheobronchial tree, leading to increased mucus production and a narrowed or blocked airway. As the inflammation continues, changes in the cells lining the respiratory tract increase resistance in the small airways, and severe imbalance in the ventilation-perfusion ([V with dot above]/[Q with dot above]) ratio decreases arterial oxygenation.
Chronic bronchitis causes hypertrophy of airway smooth muscle and hyperplasia of the mucus glands, increased number of goblet cells, ciliary damage, squamous metaplasia of the columnar epithelium, and chronic leukocytic and lymphocytic infiltration of bronchial walls. Hypersecretion of the goblet cells blocks the free movement of the cilia, which normally sweep
dust, irritants, and mucus away from the airways. Accumulating mucus and debris impair the defenses and increase the likelihood of respiratory tract infections. (See Mucus buildup in chronic bronchitis.)
dust, irritants, and mucus away from the airways. Accumulating mucus and debris impair the defenses and increase the likelihood of respiratory tract infections. (See Mucus buildup in chronic bronchitis.)
Additional effects include narrowing and widespread inflammation within the airways. Bronchial walls become inflamed and thickened from edema and accumulation of inflammatory cells, and smooth-muscle bronchospasm further narrows the lumen. Initially, only large bronchi are involved, but eventually all airways are affected. Airways become obstructed and close, especially on expiration, trapping the gas in the distal portion of the lung. Consequent hypoventilation leads to a [V with dot above]/[Q with dot above] mismatch and resultant hypoxemia and hypercapnia.
Complications
Recurrent respiratory tract infection
Cor pulmonale
Polycythemia
Assessment findings
The clinical effects of chronic bronchitis may include:
insidious onset with progressive cough and exertional dyspnea
upper respiratory infections associated with increased sputum production and worsening dyspnea, which takes progressively longer to resolve; copious gray, white, or yellow sputum
weight gain due to edema
cyanosis
tachypnea
prolonged expiratory time and use of accessory muscles of respiration.
Diagnostic test results
Arterial blood gas (ABG) analysis may show decreased partial pressure of arterial oxygen and normal or increased partial pressure of arterial carbon dioxide.
Chest X-ray may show hyperinflation and increased bronchovascular markings.
Electrocardiogram may show atrial arrhythmias; peaked P waves in leads II, III, and aVF; and, occasionally, right ventricular hypertrophy.
Pulmonary function tests show increased residual volume, decreased vital capacity and forced expiratory volumes, and normal static compliance and diffusing capacity.
Treatment
Antibiotics are given to treat infections. Avoidance of smoking and air pollutants is strongly recommended. Bronchodilators are given to relieve bronchospasm and facilitate mucociliary clearance. The patient will require adequate fluid intake and chest physiotherapy to move secretions. Ultrasonic or mechanical nebulizer treatments may be needed to loosen secretions and aid in mobilization. The patient may occasionally require corticosteroids. Diuretics may be given for edema. Oxygen will be given to the patient with hypoxemia or cor pulmonale.
Nursing interventions
Answer the patient’s questions, and encourage him and his family to express their concerns about the illness. Include the patient and his family in care decisions. Refer them to other support services, as appropriate.
Assess for changes in baseline respiratory function. Evaluate sputum quality and quantity, restlessness, increased tachypnea, and altered breath sounds. Report changes immediately.
As needed, perform chest physiotherapy, including postural drainage and chest percussion and vibration for involved lobes, several times daily.
Weigh the patient three times per week, and assess for edema.
Provide the patient with a high-calorie, protein-rich diet. Offer small, frequent meals to conserve the patient’s energy and prevent fatigue.
Make sure the patient receives adequate fluids (at least 3 qt [3 L]/day) to loosen secretions.
Schedule respiratory therapy at least 1 hour before or after meals. Provide mouth care after bronchodilator inhalation therapy.
Encourage daily activity, and provide diversional activities, as appropriate. To conserve the patient’s energy and prevent fatigue, help him to alternate periods of rest and activity.
Give medications as ordered, and note the patient’s response to them. (See Chronic bronchitis teaching topics.)
DISCHARGE TEACHING
Explain the disease process and its treatments.
Discuss the importance of not smoking and of avoiding other bronchial irritants, such as secondhand smoke, allergens, pollution, aerosol sprays, and adverse weather conditions.
Advise the patient to avoid crowds and people with infections and to obtain influenza and pneumococcal immunizations.
Warn the patient that exposure to blasts of cold air may trigger bronchospasm; suggest that he avoid cold, windy weather and that he cover his mouth and nose with a scarf or mask if he must go outside.
Explain all drugs, including their indications, dosages, adverse effects, and special considerations.
Demonstrate how to use a metered-dose inhaler.
Show the proper use of safe home oxygen therapy.
Teach the patient and his family how to perform postural drainage and chest physiotherapy.
Discuss the importance of drinking plenty of fluids to liquefy secretions.
CYSTIC FIBROSIS
Cystic fibrosis is a chronic, progressive, inherited disease that affects the exocrine (mucus-secreting) glands. The disease is transmitted as an autosomal recessive trait and is the most common fatal genetic disease of white children. When both parents are carriers of the recessive gene, they have a 25% chance of transmitting the disease with each pregnancy.
The incidence of cystic fibrosis is highest in people of northern European ancestry. The disease is less common in Blacks, Native Americans, and people of Asian ancestry. It occurs with equal frequency in both sexes.
Cystic fibrosis is incurable; however, medical research is underway to find better treatments. Life expectancy has greatly increased; it’s now about 32 years.
Pathophysiology
The gene responsible for cystic fibrosis, located on chromosome 7, encodes a membrane-associated protein called the cystic fibrosis transmembrane conductance regulator protein. The exact function of this protein remains unknown, but it appears to help regulate chloride transport across epithelial membranes. The immediate causes of symptoms are increased viscosity of bronchial, pancreatic, and other mucous gland secretions and consequent destruction of glandular ducts. Cystic fibrosis accounts for almost all cases of pancreatic enzyme deficiency in children.
Complications
Bronchiectasis
Pneumonia
Atelectasis
Hemoptysis
Dehydration
Distal intestinal obstructive syndrome
Malnutrition
Fat-soluble vitamin deficiency
Gastroesophageal reflux
Nasal polyps
Rectal prolapse
Cor pulmonale
Hepatic disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree