More adults than children are now living in the United States with congenital heart disease (CHD). To accommodate the needs of this burgeoning population, there are an increasing number of centers providing care for adults with CHD. We sought to identify pertinent obstacles encountered in the development of a newly established adult CHD program. A survey regarding CHD knowledge, insurance, and cardiovascular counseling was provided to new clinic patients aged ≥18 years. Crosstab correlations were performed to identify relations among categorical variables. Of 145 subjects (54% women; mean age 31 ± 11 years), 84% had at least moderately complex CHD. Household income was <$40,000 for 51% of subjects. There were a significantly greater number of adults, aged 30 to 54 years, with public insurance compared with the national average (p = 0.005). Of 83% of subjects reporting CHD knowledge, 71% correctly identified their defect. Self-reported CHD knowledge correlated positively with higher education (p = 0.019), higher income (p = 0.036), health maintenance organization or preferred provider organization insurance (p = 0.01), and higher level of CHD complexity (p = 0.012); however, none of these factors significantly affected correct identification of one’s CHD. In fact, patients with the most complex disease were the least likely to correctly identify their defects. In general, cardiovascular and sexual health screening was lacking. In conclusion, adult patients with CHD require robust ancillary services and special attention to lifelong insurance and counseling. Implementation of a health-care strategy to identify patients’ needs can help to overcome socioeconomic obstacles and contribute to the success of the newly established adult CHD program.
The number of adults with congenital heart disease (CHD) has surpassed the number of children in the United States with CHD. The estimated number of adults with CHD in the United States now exceeds 1 million with approximately 1/2 with complex CHD. Throughout the last decade, there has been extensive discussion with respect to not only who should provide care for adults with CHD but also where this care should take place. The concept of regional centers to evaluate and treat adult patients with CHD in a collaborative environment was agreed upon by the participants of the 32nd Bethesda Conference and a consensus statement later provided by the American College of Cardiology/American Heart Association Guidelines for the Management of Adults with CHD. Despite this effort to coordinate care at regional centers, there had been no organization tasked with formally identifying these centers to bestow such recognition. Adults with CHD are a complex and diverse group of patients because of not only their underlying cardiac problems but also their medical co-morbidities, psychosocial issues, financial situations, and counseling needs. We sought to identify obstacles commonly encountered, including socioeconomic factors and health-care behaviors, which may impact on the successful development of a new adult CHD program.
Methods
A single-center, prospective, cross-sectional study was conducted at the Heart Institute, Children’s Hospital of Pittsburgh of UPMC, Adult Congenital Heart Disease Clinic from March 25, 2011 through March 20, 2012. Patients (aged ≥18 years) were asked to participate and enrolled in the study from our outpatient adult CHD clinic after providing informed consent. Participants completed the study survey before their scheduled adult CHD clinic visit. The study and survey were approved by the Institutional Review Board.
New patients comprised those who had previously followed with a pediatric cardiologist at The Heart Institute, Children’s Hospital of Pittsburgh of UPMC or those who had been seen elsewhere, by either an adult cardiologist, a pediatric cardiologist, or a primary care physician. We excluded those who had previously been seen by an adult CHD specialist to accurately assess each participant’s background knowledge regarding their CHD and pertinent previous education and counseling. Patients who lacked cognitive capability to complete questionnaires were also excluded. Demographic data obtained during chart review included age, gender, ethnicity, body mass index, zip code of residence, insurance type, and congenital heart defect. Each patient’s CHD was categorized as simple, moderately complex, or CHD of great complexity as outlined by the 32nd Bethesda Conference guidelines.
We used a subset of questions from the survey to determine if each subjects knew their congenital heart defect, and this was referred to as “CHD knowledge”. If the patient answered “yes”, a follow-up question requested the patient to name the defect. The term “CHD congruence” was used to describe when the subjects correctly identified their CHD (i.e., the answer was “congruent” or corresponded with their charted diagnosis, which was verified by the adult CHD physician). The survey also measured commonly encountered barriers to adult CHD care. Additional data collected included level of education, self-employment, annual household income, type of previous CHD care provider(s), date of last clinic visit, engagement in exercise, tobacco history, insurance concerns and previous insurance counseling, and health-care expenditure and affordability. Previous screening for cardiovascular risk factors (obesity, diabetes, hypertension, hyperlipidemia, coronary artery disease, and smoking cessation) was also assessed. Men were asked about previous counseling with respect to sexual health concerns (e.g., erectile dysfunction). Women were queried on previous education regarding contraception and pregnancy and perceived risk of pregnancy.
Answers to the survey questions were categorized by numeric assignments. Statistical analysis was performed using SPSS 13.0 for Windows (SPSS Inc., Chicago, Illinois). Patient ages were converted to categorical variables in 5-year increments up to 34 years, then 35 to 54, 55 to 64, and ≥65 years. Crosstab correlations were performed with Pearson’s chi-square test on categorical data, and the Fisher’s exact test was used for all parameters in which the expected count was <5. Crosstab correlations on ordinal data were evaluated with the gamma statistic. Comparisons between groups of continuous data were performed using the Mann-Whitney test. One-sample chi-square tests were performed to compare our data with national or regional population statistics. Statistical significance was set at a p value <0.05. Data are reported as a mean ± SD, median (interquartile range), or numbers with proportion (%).
Results
A total of 145 new patients aged ≥18 years were enrolled. The cohort comprised of 78 women (54%) with a mean and median age of 31.4 ± 11.3 and 28.4 years (interquartile range 15.6), respectively. Baseline characteristics are listed in Table 1 .
| Variable | n (%) |
|---|---|
| Age (yrs) | 31.4 ± 11.3 |
| Women | 78 (54) |
| Weight (kg) | 77.5 ± 24.3 |
| Body mass index (kg/m 2 ) | 27.4 ± 7.2 |
| <18.5 | 2 (1.4) |
| 18.5–24.9 | 66 (45.5) |
| 25–29.9 | 37 (25.5) |
| ≥30 | 40 (27.6) |
| Ethnicity | |
| European American | 131 (91) |
| African-American | 10 (7) |
| Asian Pacific American | 2 (1.4) |
| Other | 1 (0.7) |
| CHD complexity | |
| Simple | 23 (16) |
| Moderate | 70 (48) |
| Severe | 52 (36) |
| Education (highest level) | |
| High school | 66 (46) |
| Some college, vocational | 41 (29) |
| Bachelor’s degree | 24 (17) |
| Graduate degree | 12 (8) |
| Income | |
| <$40,000 | 71 (51) |
| $40,000–80,000 | 41 (30) |
| >$80,000 | 26 (18) |
| Insurance type | |
| HMO or PPO | 101 (70) |
| Medicaid/Medicare | 38 (26) |
| Uninsured | 3 (2.1) |
| Self-pay | 3 (2.1) |
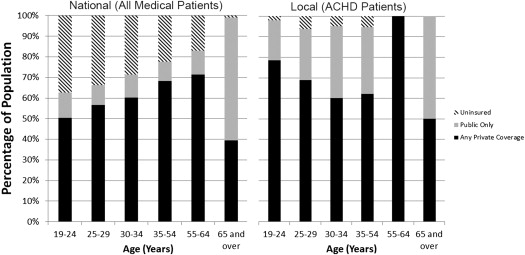
Only 25% of our subjects had completed degrees in postsecondary education, which is comparable with the national average of 27% (p = 0.31) but <38% of adult patients with CHD with bachelor’s or graduate degrees as reported in a recent multicenter trial by Gurvitz et al. In 2011, the median household income for all races was $50,054 ; however, 51% of our subjects had an income of <$40,000. Because most of our cohort was Caucasian, this income difference is more striking compared with the 2011 median income ($55,412) for non-Hispanic whites. Despite only 14% of subjects reporting previous insurance counseling, 96% of patients had some form of insurance (private: health maintenance organization or preferred provider organization, 70%; public: Medicare or Medicaid, 26%). There were a significantly greater number of adults in the 30- to 54-year age group with public insurance compared with the national average (p = 0.005; Figure 1 ).
In our cohort, there was a predominance of moderately severe CHD (48%) and CHD of great complexity (36%), with only 16% of patients having simple CHD. Some of the conditions with the highest prevalence in our study group included tetralogy of Fallot (21%), d-transposition of the great arteries (14%), bicuspid aortic valve (10%), atrioventricular septal defect (7%), ventricular septal defect (6%), coarctation of the aorta (6%), double outlet right ventricle (4%), and pulmonary stenosis (4%).
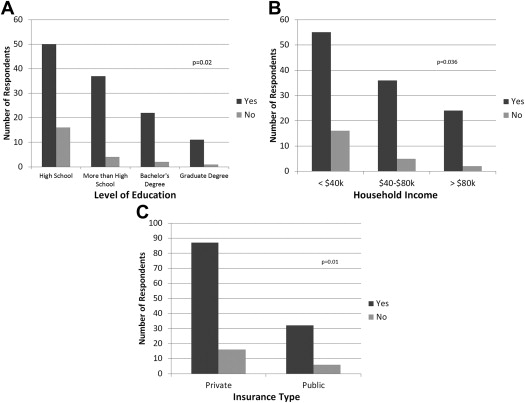
Of the total cohort, 121 (83%) reported knowing the name of their congenital heart defect (CHD knowledge). Self-reported CHD knowledge correlated positively with higher education (p = 0.019), higher income (p = 0.036), and private (health maintenance organization or preferred provider organization) insurance (p = 0.01; Figure 2 ). Of the subjects who reported knowledge of their CHD, only 71% correctly identified their underlying defects (CHD congruence). CHD congruence, or correct identification of the congenital heart defect by the patient, did not correlate with higher education (p = 0.51), higher income (p = 0.14), or private insurance (p = 0.33). Another factor that corresponded to greater self-reported CHD knowledge was CHD complexity level (p = 0.012). With increasing level of complexity, patients were more likely to report knowing the name of their CHD; however, there was no statistically significant connection between complexity level and CHD congruence. In fact, the rate of congruence was lowest (63%) in the most complex CHD group compared with 77% in the simple CHD group and 75% in the moderately severe CHD group. Gender, ethnicity, and previous provider type (primary care physician, pediatric cardiologist, general or adult cardiologist, or other subspecialty doctor) had no statistically significant influence on either self-reported CHD knowledge or CHD congruence.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


