Atrial fibrillation (AF) and obesity have reached epidemic proportions. The impact of obesity on clinical outcomes in patients with established AF is unknown. We analyzed 2,492 patients in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study. Body mass index (BMI) was evaluated as a categorical variable (normal 18.5 to <25 kg/m 2 , overweight 25 to <30 kg/m 2 , obese ≥30 kg/m 2 ). Rate of death from any cause was higher in the normal BMI group (5.8 per 100 patient-years) than in the overweight and obese groups (3.9 and 3.7, respectively). Cardiovascular death rate was highest in the normal BMI group (3.1 per 100 patient-years), lowest in the overweight group (1.5 per 100 patient-years), and intermediate in the obese group (2.1 per 100 patient-years). After adjustment for baseline factors, differences in risk of death from any cause were no longer significant. However, overweight remained associated with a lower risk of cardiovascular death (hazard ratio 0.47, p = 0.002). Obese patients were more likely to have an uncontrolled heart rate at rest, but rhythm-control strategy success was similar across BMI categories. In each BMI category, risk of death from any cause was similar for patients randomized to a rhythm- or rate-control strategy. In conclusion, in patients with established AF, overweight and obesity do not adversely affect overall survival. Obesity does not appear to affect the relative benefit of a rate- or rhythm-control strategy.
Obesity, which is epidemic in the United States, is well established as an independent risk factor for all-cause and cardiovascular mortality in the general population. However, in patients with certain established cardiovascular conditions, including coronary heart disease and heart failure, overweight and mild obesity are associated with a lower risk of death—the “obesity paradox.” Recently, obesity has been demonstrated to be an independent risk factor for development of atrial fibrillation (AF), a condition that is also rapidly increasing in prevalence. Given this interconnection between obesity and AF, we sought to determine the relation between obesity and clinical outcomes in patients with established AF. The Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study provided a large, well-characterized cohort of patients with high-risk AF in which to do so.
Methods
Details of the AFFIRM protocol have been reported previously. Briefly, patients with AF requiring long-term treatment and with ≥1 risk factor for death or stroke were enrolled. Patients were randomized to a rate-control strategy or a rhythm-control strategy. Mean follow-up was 3.5 years (range 0 to 6). Heart rate control at rest was assessed at the 1-year visit and was considered adequate if ≤80 beats/min. Classification of all fatal events and strokes was adjudicated by an independent clinical events committee. The institutional review board of the University of Washington approved the protocol, and each clinical site obtained approval from its local institutional review board. Every patient gave signed, informed consent to participate in the study. The study was supported by the National Heart, Lung, and Blood Institute ( http://www.ClinicalTrials.gov , identifier NCT00000556 ).
Height and weight were recorded for AFFIRM participants at the baseline visit. Body mass index (BMI) was calculated by dividing weight in kilograms by the square of height in meters. BMI was categorized according to the World Health Organization/National Institutes of Health classification scheme, with normal defined as 18.5 to <25 kg/m 2 , overweight as 25 to <30 kg/m 2 , and obese as ≥30 kg/m 2 . The obese category was further subdivided into mildly obese (BMI 30 to <35 kg/m 2 ), severely obese (BMI 35 to <40 kg/m 2 ), and extremely obese (BMI ≥40 kg/m 2 ). Underweight patients (BMI <18.5 kg/m 2 ) were excluded from analysis.
Baseline characteristics were compared across the 3 BMI groups using analysis of variance. The primary end point was a comparison of death from any cause. Other clinical end points included cardiovascular death and stroke. Number of events per 100 person-years at risk was calculated for patients in each BMI group. Rate ratios were then calculated, comparing each BMI group with the other 2 groups. Corresponding p values were calculated using Fisher’s 2-tailed exact chi-square test. Cox proportional hazards modeling, using a stepwise regression procedure, was used to determine the independent relation between BMI category and clinical events. Covariables that remained statistically significant and those that were deemed clinically relevant were included in the final model. These included age; gender; history of hypertension, diabetes mellitus, smoking, coronary artery disease, heart failure, or stroke; rhythm at randomization; left ventricular ejection fraction; and randomized treatment group.
In the rate-control arm, we assessed mean heart rate at rest and the proportion of patients with uncontrolled heart rate at rest (>80 beats/min) at the 1-year visit in patients remaining in AF. In the rhythm-control arm, we assessed the proportion of patients never achieving sinus rhythm, the proportion of patients with ≥1 episode of AF during the study period, and the proportion of electrical cardioversions that were successful in restoring sinus rhythm. All analyses were conducted using SAS 8.2 (SAS Institute, Cary, North Carolina). A 2-sided p value <0.05 was considered to represent statistical significance.
Results
BMI was available for 2,518 of 4,060 patients enrolled in AFFIRM. After exclusion of underweight patients (n = 26), the cohort for this analysis consisted of 2,492 patients (61.4% of total AFFIRM population). Baseline characteristics of patients with and without missing BMI data were generally similar, although patients with missing BMI data were significantly more likely to have a history of coronary artery disease (40% vs 37%) and heart failure (26% vs 21%) and were less likely to be enrolled after a first episode of AF (31% vs 38%).
Mean BMI was 29.0 ± 5.9 kg/m 2 . The normal BMI, overweight, and obese groups included 637 patients (25.5%), 965 patients (38.7%), and 890 patients (35.7%), respectively. Of patients in the obese group, 556 were mildly obese (22.3% of total), 207 were severely obese (8.3% of total), and 127 were extremely obese (5.1% of total). Significant differences between BMI groups were noted with respect to numerous baseline co-morbidities and medications ( Table 1 ).
| Variable | BMI (kg/m 2 ) | p Value | ||
|---|---|---|---|---|
| 18.5–<25 | 25–<30 | ≥30 | ||
| (n = 637) | (n = 965) | (n = 890) | ||
| Age (years), mean ± SD | 72.4 ± 7.1 | 70.7 ± 7.5 | 66.4 ± 8.4 | <0.001 |
| Body mass index (kg/m 2 ), mean ± SD | 22.7 ± 1.6 | 27.5 ± 1.5 | 35.2 ± 5.1 | <0.001 |
| Women | 321 (50%) | 305 (32%) | 353 (40%) | <0.001 |
| Rate control group | 310 (49%) | 499 (52%) | 440 (49%) | 0.4 |
| Hypertension | 392 (62%) | 658 (68%) | 724 (81%) | <0.001 |
| Diabetes mellitus | 73 (12%) | 163 (17%) | 264 (30%) | <0.001 |
| Smoking | 86 (14%) | 99 (10%) | 104 (12%) | 0.1 |
| History of coronary artery disease | 201 (32%) | 404 (42%) | 319 (36%) | <0.001 |
| Previous myocardial infarction | 87 (14%) | 185 (19%) | 141 (16%) | 0.01 |
| Previous heart failure | 124 (20%) | 190 (20%) | 217 (24%) | 0.02 |
| Previous stroke or transient ischemic attack | 98 (15%) | 123 (13%) | 93 (11%) | 0.02 |
| First episode of atrial fibrillation | 214 (34%) | 358 (37%) | 943 (38%) | 0.005 |
| Atrial fibrillation at randomization | 288 (46%) | 444 (46%) | 396 (45%) | 0.8 |
| Systolic blood pressure (mm Hg), mean ± SD | 136 ± 18.5 | 134 ± 18.8 | 134 ± 18.6 | 0.07 |
| Ejection fraction (%), mean ± SD | 55.9 ± 7.9 | 55.7 ± 7.3 | 55.3 ± 7.8 | 0.5 |
| Left atrial dimension >4 cm | 424 (67%) | 702 (73%) | 716 (76%) | <0.001 |
| Warfarin | 555 (87%) | 844 (87%) | 771 (87%) | 0.9 |
| Angiotensin-converting enzyme inhibitor | 208 (33%) | 371 (38%) | 411 (46%) | <0.001 |
| β blocker | 266 (42%) | 451 (47%) | 404 (45%) | 0.1 |
| Calcium channel blocker | 142 (23%) | 195 (21%) | 234 (27%) | 0.06 |
| Digoxin | 286 (47%) | 351 (39%) | 375 (44%) | 0.005 |
| Amiodarone | 122 (19%) | 188 (19%) | 178 (20%) | 0.6 |
| Sotalol | 104 (16%) | 147 (15%) | 152 (17%) | 0.5 |
| Class I antiarrhythmic drug | 93 (15%) | 108 (12%) | 90 (11%) | 0.02 |
Clinical event rates are presented in Table 2 . There was no significant difference in the rate of stroke in patients in any of the BMI categories. Death from any cause occurred in 304 patients (12.2%) during the study period. Observed death rate was significantly higher in patients in the normal BMI group (5.8 deaths per 100 patient-years) than in those in the overweight group (3.9 deaths per 100 patient-years, p = 0.005) and obese group (3.7 deaths per 100 patient-years, p = 0.002). Of patients in the obese group, death rates were 3.5 per 100 patient-years in mildly obese patients, 4.4 per 100 patient-years in severely obese patients, and 3.3 per 100 patient-years in extremely obese patients (p = NS for comparisons among these groups).
| Normal | Overweight | Obese | |
|---|---|---|---|
| (n = 637) | (n = 965) | (n = 890) | |
| Death from any cause per 100 person-years (95% CI) | 5.8 (4.8–7.1) | 3.9 (3.3–4.7) ⁎ | 3.7 (3.0–4.5) ⁎ |
| Cardiovascular death per 100 person-years (95% CI) | 3.1 (2.4–4.0) | 1.5 (1.1–2.0) ⁎ | 2.1 (1.6–2.8) |
| Stroke per 100 person-years (95% CI) | 1.1 (0.7–1.8) | 1.2 (0.8–1.7) | 1.2 (0.8–1.7) |
Cardiovascular death occurred in 148 patients (5.9%). Observed cardiovascular death rate was highest in patients in the normal BMI group (3.1 per 100 patient-years), lowest in those in the overweight group (1.5 per 100 patient-years, p = 0.001 vs normal BMI group), and intermediate in those in the obese group (2.1 per 100 patient-years, p = 0.07 vs normal BMI group). Of patients in the obese group, cardiovascular death rates were 1.9 per 100 patient-years in mildly obese patients, 2.7 per 100 patient-years in severely obese patients, and 2.2 per 100 patient-years ing extremely obese patients (p = NS for comparisons among these groups).
Results of multivariable Cox proportional hazards models are presented in Table 3 . After adjustment for relevant covariables, neither overweight nor obesity was significantly associated with risk of death from any cause. Overweight was significantly associated with a lower risk of cardiovascular death (hazard ratio [HR] 0.47, p = 0.002).
| Variable | HR (95% CI) | p Value |
|---|---|---|
| Death from any cause | ||
| Overweight | 0.74 (0.53–1.03) | 0.07 |
| Obese | 0.82 (0.57–1.18) | 0.3 |
| Age (per year) | 1.06 (1.04–1.08) | <0.001 |
| Female gender | 0.85 (0.63–1.15) | 0.3 |
| Hypertension | 1.29 (0.94–1.75) | 0.12 |
| Diabetes | 1.99 (1.48–2.66) | <0.001 |
| Smoking | 1.84 (1.27–2.65) | 0.001 |
| Coronary artery disease | 1.82 (1.37–2.42) | <0.001 |
| Congestive heart failure | 2.05 (1.53–2.76) | <0.001 |
| Stroke | 1.69 (1.20–2.39) | 0.003 |
| Ejection fraction <50% | 1.17 (1.01–1.36) | 0.04 |
| Atrial fibrillation at randomization | 0.82 (0.63–1.07) | 0.14 |
| Rhythm-control arm | 1.23 (0.94–1.6) | 0.14 |
| Cardiovascular death | ||
| Overweight | 0.47 (0.29–0.76) | 0.002 |
| Obese | 0.69 (0.42–1.14) | 0.15 |
| Age (per year) | 1.04 (1.01–1.07) | 0.005 |
| Female gender | 1.12 (0.74–1.71) | 0.6 |
| Hypertension | 1.36 (0.86–2.16) | 0.2 |
| Diabetes | 2.36 (1.57–3.57) | <0.001 |
| Smoking | 1.55 (0.92–2.63) | 0.10 |
| Coronary artery disease | 1.80 (1.20–2.72) | 0.005 |
| Congestive heart failure | 2.56 (1.69–3.89) | <0.001 |
| Stroke | 1.97 (1.19–3.24) | 0.008 |
| Ejection fraction <50% | 1.41 (1.16–1.72) | <0.001 |
| Atrial fibrillation at randomization | 0.80 (0.55–1.17) | 0.3 |
| Rhythm-control arm | 1.14 (0.78–1.66) | 0.5 |
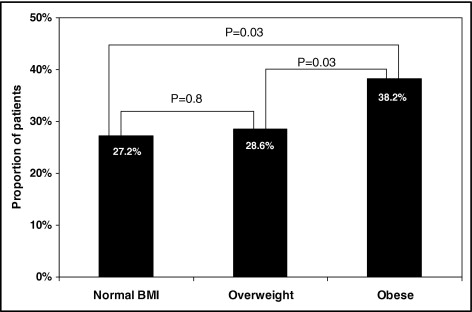
Complete data were available for 1,249 patients randomized to a rate-control strategy. There were 522 patients (42%) in AF at the time of the baseline visit, and mean heart rate at rest was similar in patients in each BMI group (normal 80.7 ± 14.8 beats/min, overweight 80.0 ± 13.4 beats/min, obese 80.7 ± 14.3 beats/min, p = 0.9). At the 1 year visit, the number of patients in AF increased to 642, comprising 56% of patients with available 1-year follow-up. The proportion of patients receiving β blockers and calcium channel blockers at 1 year was similar in each BMI group, whereas digoxin use was significantly lower in overweight patients (normal BMI 59.2%, overweight 44.1%, obese 53.7%, p <0.01). For patients in AF, mean heart rate at rest at 1 year was significantly higher in obese patients (78.7 ± 13.2 beats/min) than in patients in the normal BMI group (75.1 ± 12.8 beats/min, p = 0.02) and tended to be higher than in overweight patients (76.1 ± 12.5 beats/min, p = 0.06). The proportion of patients in AF with uncontrolled heart rate at rest (>80 beats/min) at 1 year was significantly higher in obese patients than in patients in each of the other BMI groups ( Figure 1 ). After adjustment for baseline differences and rate-control medication use at 1 year, obese patients remained more likely to have an uncontrolled heart rate at rest compared to patients in the normal BMI group (HR 1.9, 95% confidence interval [CI] 1.1 to 3.1, p = 0.01). Few patients in AF had a heart rate at rest >100 beats/min at the 1-year visit (5 in normal BMI group, 3.4%; 9 in overweight group, 3.4%; 11 in obese group, 4.6%; p = NS for all comparisons).