PCI, percutaneous coronary intervention.
All values are given in minutes. P < 0.05 considered statistically significant.
Modified from Schaufele TG, Grunebaum JP, Lippe B., Breidenbach T, von Hodenbery, E. Radial access versus conventional femoral puncture: Outcome and resource effectiveness in a daily routine. The RAPTOR-Trial. Paper presented at the Scientific Sessions of the American Heart Association 2009, Orlando, FL.
TABLE 25-2 Staff Workload
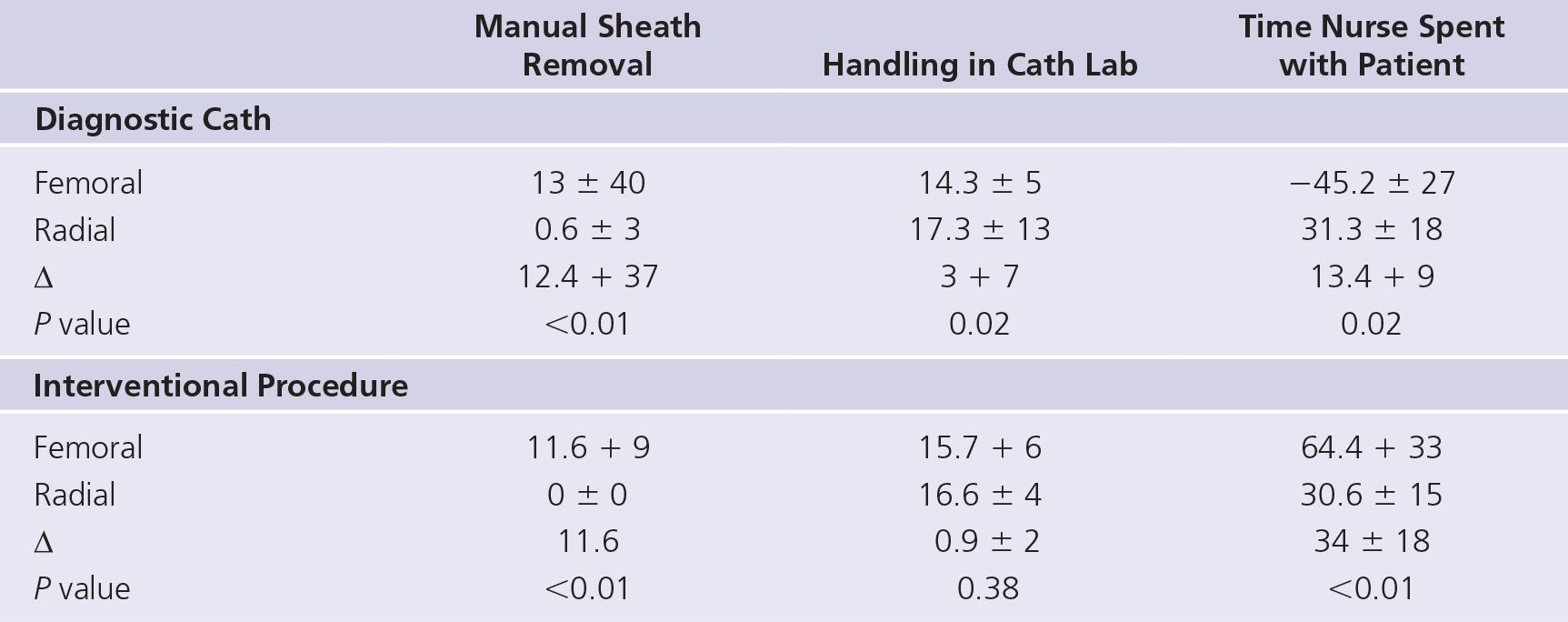
Time is given in minutes.
Modified from Schaufele TG, Grunebaum JP, Lippe B, et al. Radial access versus conventional femoral puncture: outcome and resource effectiveness in a daily routine. The RAPTOR-Trial. Paper presented at the Scientific Sessions of the American Heart Association 2009, Orlando, FL.
TABLE 25-3 Economic Impact of Staff Involvement
| Time: Diagnostic Cath 1 Sheath Removal | Time: Diagnostic 1 PCI 1 Sheath Removal |
Femoral | 72.5 + 36 | 91.7 + 36 |
Radial | 54.6 ± 14 | 47.2 ± 12 |
Time saved by radial access | 17.9 ± 30 | 47.2 ± 24 |
P value | <0.01 | <0.01 |
Time is given in minutes; 3,000 procedures/yr; 1,000 PCIs change staff involvement by 1,383 hr = 36.4 wk.
Modified from Schaufele TG, Grunebaum JP, Lippe B, et al. Radial access versus conventional femoral puncture: outcome and resource effectiveness in a daily routine. The RAPTOR-Trial. Paper presented at the Scientific Sessions of the American Heart Association 2009, Orlando, FL.
Postprocedural Nursing
There are many factors that can influence the NWL after a coronary procedure:
• Care needed for compression of the arterial puncture
• Workload required for visualization and evaluation of the access site
• Supervision and management of bleeding complications
• Basic bedside needs, i.e., assistance with eating, elimination
• Baseline independence of the patient
• Type of recovery unit
• Length of stay postprocedure
• Type of coronary procedure (diagnostic vs interventional)
TABLE 25-4 Ward NWL According to Clinical, Procedural, In-hospital Variables, and Arterial Access
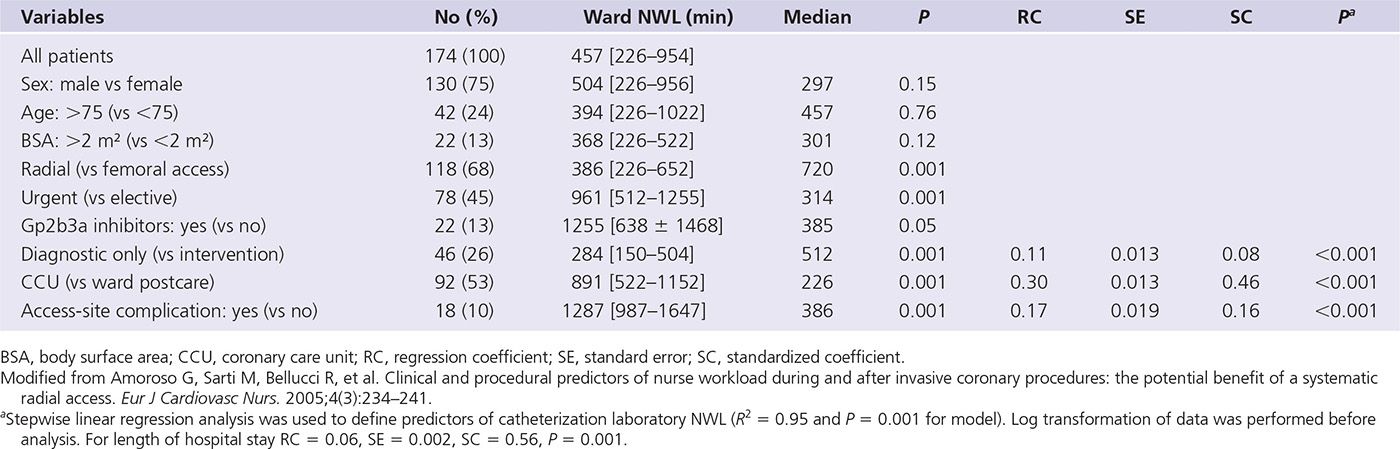
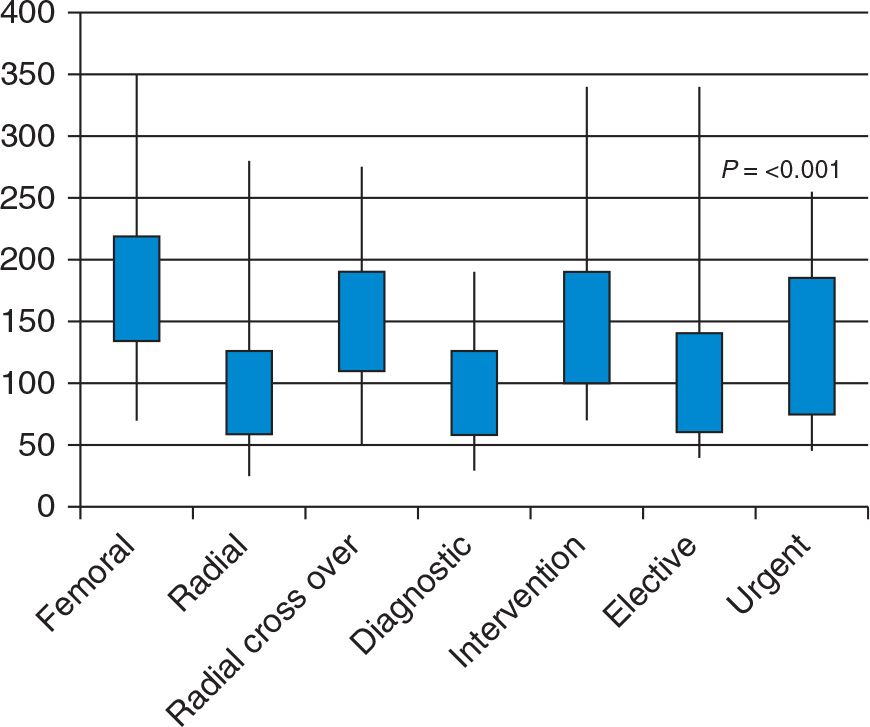
FIGURE 25-1 Differences in catheterization laboratory NWL, according to arterial access (radial vs femoral), procedure performed (diagnostic vs intervention), or procedure type (urgent vs elective). The values for nursing workload are given by the midrange (25th and 75th percentiles) by the hinges of the boxes and the 5th and 95th percentiles by the whiskers. (Modified from Amoroso G, Sarti M, Bellucci R, et al. Clinical and procedural predictors of nurse workload during and after invasive coronary procedures: the potential benefit of a systematic radial access. Eur J Cardiovasc Nurs. 2005;4(3):234–241.)
In the case of the transradial procedure, hemostasis is usually achieved by manual compression and maintained by means of a compression band (Fig. 25-2). In most cases a single individual can easily manage the care of one or more transradial patients. Carrington et al.11 studied nurse engagement in the recovery area utilizing different surveillance protocols. When hemostasis was achieved utilizing the TR Band device (Terumo, Tokyo, Japan), the patients were reclassified into a lower nurse supervision level. Patients were then placed in an accelerated (1-hour) or a conventional (2-hour) weaning process. The accelerated arm showed no difference in complication rates, compared to the conventional arm. However, there was a 50% decrease in the surveillance phase because of the accelerated protocol. This decrease equates to one-quarter to one-third of the average recovery length of stay. Owing to the decreased length of stay, there is a reduction in nursing time spent in the care of the patient, thus decreasing the costs of the procedure.

FIGURE 25-2 Compression of the radial artery by means of Terumo TR band.
Caputo12 supplied a cost perspective in which nurses’ salaries were considered. A cardiac catheterization nurse’s hourly wage was reported as $41.70 and a recovery nurse’s hourly wage was reported as $36.54. The routine recovery time was 3 hours for TRA and 6 hours for TFA. For a catheterization laboratory performing 1,000 radial cases a year (versus femoral cases), this equates to a cost savings of $109,620 per year in the recovery process alone. Roussanov et al.9 reported a similar time savings for TRA versus TFA care in the recovery period. In their study, the patients enrolled in the TRA group had a shorter recovery stay (126 ± 36 minutes) than did those in the TFA group utilizing a vascular closure device (150 ± 48 minutes: P <0.04). The findings also noted that the recovery time for the TRA group was nearly half that for the TFA group in which manual pressure was utilized for hemostasis (240 ± 42 minutes: P < 0.0001). A cost savings of 33% was noted with TRA cases in comparison with femoral closure device cases ($185 ± $52 vs $208 ± $70.4: P < 0.001). In cases where transradial hemostasis with a compression band is compared with transfemoral closure with a device, there is a savings of 24 minutes of nursing time. When transradial hemostasis with a compression band is compared with manual transfemoral hemostasis, a savings of 114 minutes can be gained. Nursing time represents a huge cost component of the invasive coronary procedure. Steinbrook13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


