Fig. 1.1
Schematic illustration of anatomy of the right atrium. The right atrium (RA) is composed of the appendage (arrow head), venous component, and the vestibule. The venous component is the smooth wall of the RA and receives the SVC, IVC, and CS. The vestibule is a smooth muscle rim surrounding the tricuspid valve (TV) orifice. Note ridge of crista terminalis (thick arrows) and Eustachian valve (thin arrow). RA right atrium, SVC superior vena cava, IVC inferior vena cava, CS coronary sinus
The right atrial appendage is derived from the primitive auricle, evolving a triangular-shaped structure with trabeculation and pectinate muscles (Fig. 1.2).


Fig. 1.2
Pectinate muscle of the right atrial appendage (arrow)
The venous component is derived from the right sinus venosus, evolving the smooth wall of the RA. It receives the superior vena cava (SVC) and inferior vena cava (IVC) on its posterior surface and the coronary sinus (CS) at its junction with the atrial septum, just above the posterior interventricular groove.
The vestibule is also known as the supravalvular lamina and is a smooth muscle rim surrounding the tricuspid valve orifice.
The tricuspid valve is present between the RA and right ventricle (RV).
The sinoatrial (SA) node is present in the subepicardial side of the superior cavoatrial junction, supplied by the SA nodal artery (Figs. 1.3 and 1.4). The atrioventricular (AV) node is present at the inferior wall of the RA (Fig. 1.5), within the boundaries of Koch’s triangle near its apex (see the anatomy for electrophysiology).
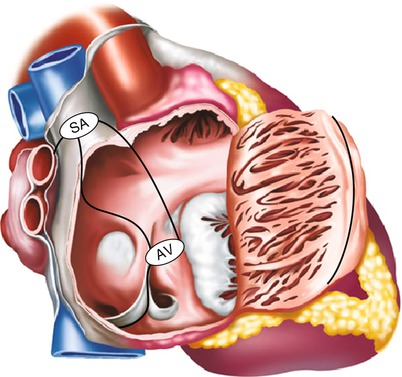
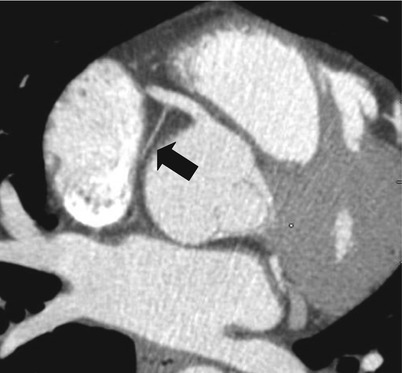
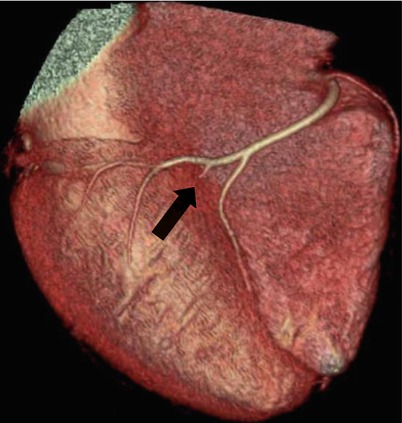
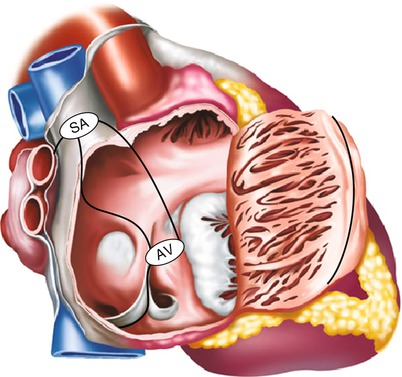
Fig. 1.3
Schematic illustration of conducting system of the right atrium. Sinoatrial node (SA) connects to the atrioventricular node (AV) through the anterior, middle, and posterior branches
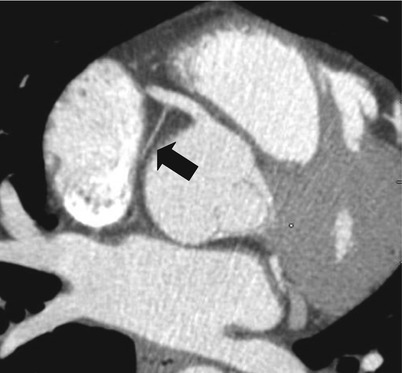
Fig. 1.4
Sinoatrial nodal branch of the RCA (arrow) indicates the location of SA node
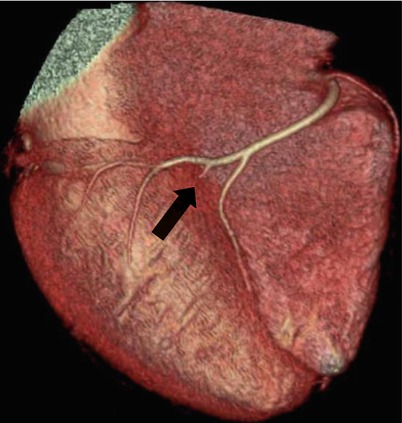
Fig. 1.5
Atrioventricular nodal branch of the RCA (arrow) indicates the location of AV node (floor of the right atrium)
1.1.2 Anatomic Pitfall and Normal Variance
1.1.2.1 Crista Terminalis
The crista terminalis is a vertically oriented, internal muscular ridge between the RA appendage and sinus venous component, representing the line of fusion between the primitive auricle and sinus venosus. It extends from the SVC to the IVC (Fig. 1.1).
The crista terminalis is often seen on routine contrast-enhanced chest CT and echocardiography, and is sometimes misinterpreted as a tumor or thrombus. Cardiac CT can easily identify the location and extension of the fibromuscular prominent structure and can differentiate it from a neoplasm or a thrombus [1] (Fig. 1.6)
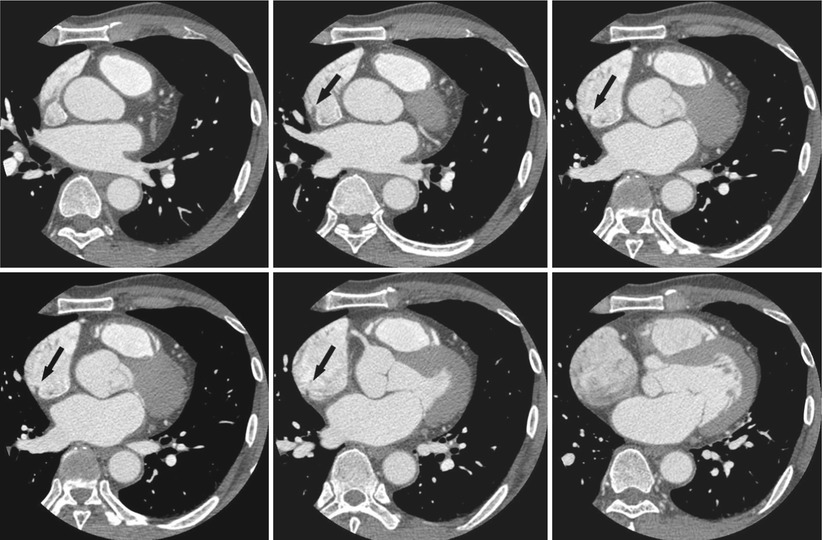
Fig. 1.6
Crista terminalis of the right atrium. Note vertically oriented internal muscular ridge (arrows) between the RA appendage and sinus venous components, from the SVC to the IVC
1.1.2.2 Eustachian Valve
The Eustachian valve, persistent of the right sinus venosus valve, is located at the junction of the IVC and RA (Fig. 1.1).
In a fetus, the Eustachian valve directs blood from the IVC to the foramen ovale. Normally, the Eustachian valve regresses during embryonic development. The lack of normal regression results in a prominent Eustachian valve or partial or complete septation of the RA, a condition referred to as cor triatriatum dexter [1, 2].
1.1.2.3 Cor Triatriatum Dexter
Cor triatriatum dexter has the same embryologic explanation as the Eustachian valve; however, cor triatriatum dexter is characterized by an attachment on the atrial septum giving the appearance of a divided atrium [4].
1.1.2.4 Thebesian Valve
The Thebesian valve, also called as the valve of the CS, is a semicircular fold of the lining membrane of the RA at the orifice of the CS. It prevents reflux from the RA into the CS during contraction. The valve varies in size [5] (Fig. 1.7).
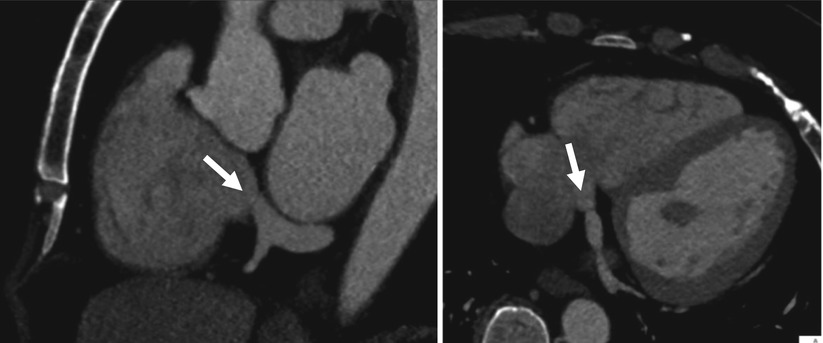
Fig. 1.7
Thebesian valve. Note the thin valve at the orifice of the coronary sinus (arrows)
Recently, the recognition of the Thebesian valve is more emphasized because it may cause difficulties during cardiac catheterization for cardiac resynchronization therapy [6].
1.2 Right Ventricle
1.2.1 Normal Anatomy
The right ventricle (RV) is composed of an inlet with the tricuspid valve, an apical trabecular component, and a subpulmonic outflow tract.
The inlet potion of the RV surrounds and supports the tricuspid valve and its tension apparatus. The tricuspid valve has three leaflets: septal (medial, conal), anterosuperior, and posterior (inferior). The septal leaflet attaches to the right ventricle septum, which makes the tricuspid valve distinguishable from the mitral valve. The valve leaflets connect to three papillary muscles through the chordae tendineae.
The anterior papillary muscle has chordae tendineae that attach to the anterior and posterior cusps of the tricuspid valve, the posterior papillary muscle has chordae tendineae that attach to the posterior (inferior) and septal cusps, and the medial papillary muscle has chordae tendineae that attach to the anterior and septal cusps.
The apical trabecular portion is continuous with the apparatus of the tricuspid valve. A well-known prominent trabeculation is the septomarginal trabeculation (septal band). The body of the septomarginal trabeculation runs to the apex of the ventricle, where it gives rise to the anterior papillary muscle before splitting into the general apical trabeculation. The anterior papillary muscle continues as the moderator band to the parietal wall of the RV. The moderator band contains the right bundle branch.
Heavy trabeculation, coarse septal surface, and moderator band are the unique distinguishing features of the right ventricle (Figs. 1.8 and 1.9).
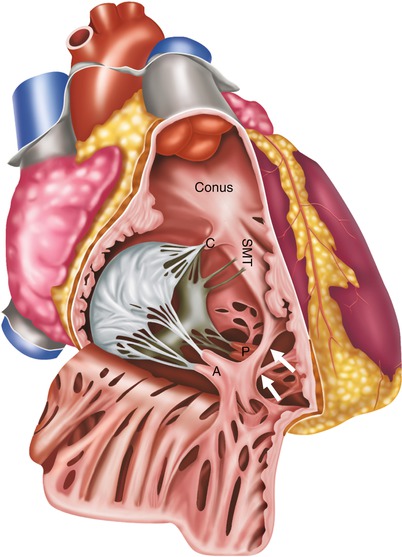
Fig. 1.8
Schematic illustration of anatomy of the right ventricle. Note the septomarginal trabeculation that gives rise to the anterior papillary muscle (A) and anterior papillary muscle continues as the moderator band (arrows). C conal papillary muscle, A anterior papillary muscle, P posterior papillary muscle, SMT septomarginal trabeculation

Fig. 1.9
Moderator band of the right ventricle on axial image (arrow)
The subpulmonic outflow tract, known as the pulmonary infundibulum (conus), is a tubular muscular structure that supports the leaflets of the pulmonary valve. The posterior wall of the infundibulum is formed by a prominent muscular ridge, known as the crista supraventricularis, that separates the tricuspid and pulmonary valves. It is also a unique feature of the RV because in the left ventricle, the aortic and mitral valves have fibrous continuity (Fig. 1.10).
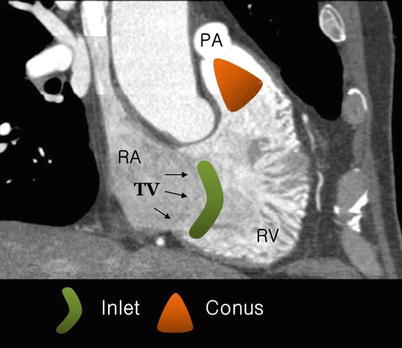
Fig. 1.10
Inlet and outlet (conus) of the right ventricle on oblique coronal image. Note heavy trabeculation of the right ventricular wall. RA right atrium, RV right ventricle, TV tricuspid valve
The RV wall is normally very thin, approximately 3 mm in thickness.
The pulmonary valve is composed of three leaflets: left, right, and posterior leaflets (Fig. 1.11).
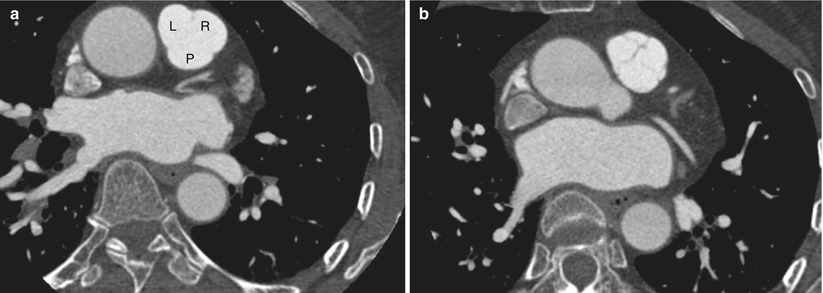
Fig. 1.11
Pulmonary valve with three leaflets (a, b): left (L), right (R), and posterior (P)
1.2.2 Anatomic Pitfall and Normal Variance
1.2.2.1 Fat Deposition of the Right Ventricle
Right ventricular fat infiltration is not rare in asymptomatic elderly patient. According to Kim et al. [7], RV fat infiltration occurs in about 17 % of asymptomatic subjects on CT. Fat infiltrations were most frequently seen in the superior wall of the base, middle segments, and the right ventricular outlow tract with normal or increased thickness (Fig. 1.12).
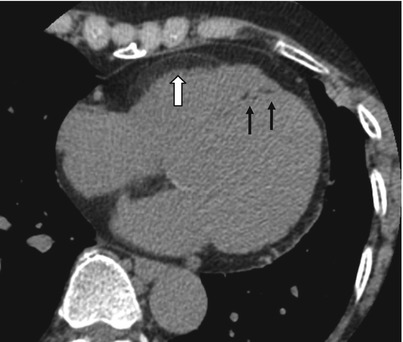
Fig. 1.12
Fat deposition of the right ventricle in a 75-year-old asymptomatic woman. Note fat deposition at right ventricular free wall (white arrow) and papillary muscles (thin arrows)
The clinical significance of RV fat is not clear. Because autopsy studies indicate that the frequency and degree of RV myocardial fat increase with age, its development is considered as a part of aging process. The relationship between RV myocardial fat and other factors, such as gender and obesity, is disputed [8].
Arrhythmogenic right ventricular dysplasia (ARVD) should be excluded when right ventricular fat infiltration is found in a symptomatic, young patient. The RV free wall of ARVD is usually almost thin because of fibrofatty replacement extending from the epicardium toward the endocardium. In contrast, with physiologic fat, the RV free wall maintains normal thickness or is sometimes thickened [8].
1.3 Left Atrium
1.3.1 Normal Anatomy
The left atrium (LA) also consists of a venous component, appendage, and a supravalvular vestibule like the RA.
The smooth-walled venous component is posteriorly located and receives blood from the four pulmonary veins.
The LA appendage is derived from the primitive atrium and has pectinate muscle. It is a potential space for thrombus deposition because of its narrow neck with the LA. The vestibule supports the leaflets of the mitral valve.
The mitral valve has anterior and posterior leaflets and shares the fibrous continuity with the aortic valve. The mitral valve annulus embedded in the myocardium is part of the cardiac skeleton (Fig. 1.13).
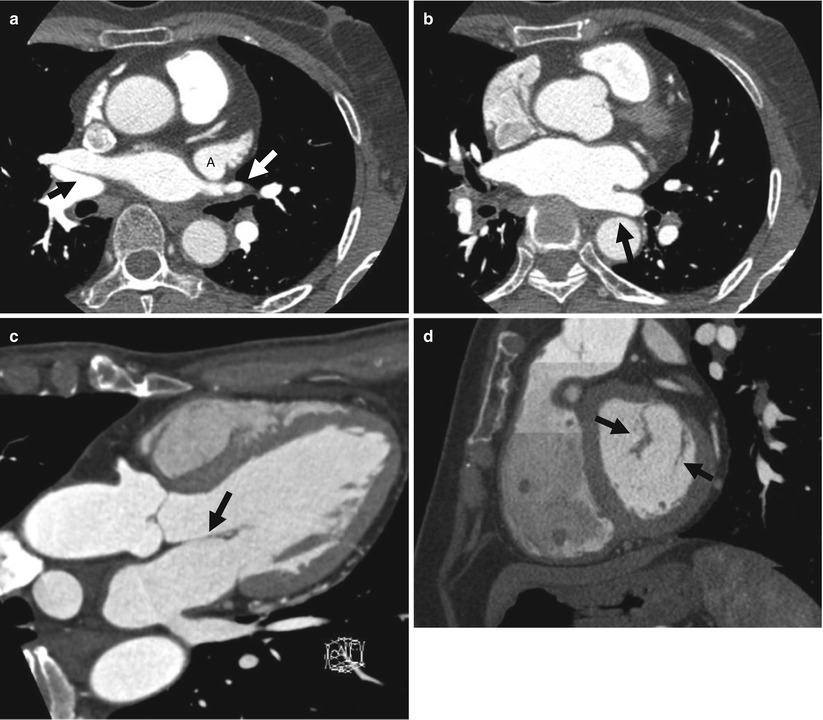
Fig. 1.13
Anatomy of the left atrium. (a, b) LA appendage (A) with pectinate muscle and posterior venous component draining pulmonary veins (arrows). (c) The mitral valve shares the fibrous continuity with the aortic valve (arrows). (d) Anterior and posterior leaflets of mitral valve on sagittal image (arrows)
1.3.2 Anatomic Pitfall and Normal Variance
1.3.2.1 Accessory Left Atrial Appendage and Left Atrial Diverticulum
Accessory left atrial appendage is an outpouching with a discernible ostium, neck, and body that display irregular contours suggestive of the pectinate muscles. Accessory appendages share a common embryonic origin from the primitive atrium with the LA appendage and have significant contractile function [9] (Fig. 1.14).
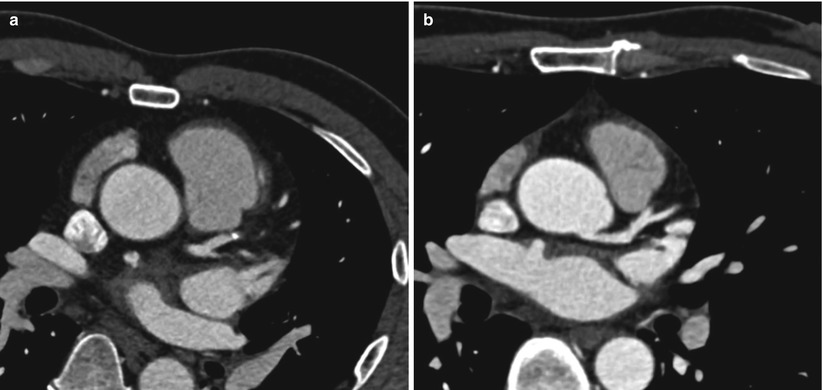
Fig. 1.14
Accessory left atrial appendage and left atrial diverticulum. (a) Accessory left atrial appendage. Note discernible ostium, neck, and irregular contoured body, suggesting pectinate muscle. (b) Saclike outpouching with broad base, suggesting left atrial diverticulum
Left atrial diverticulum is a saclike outpouching with a relatively broad-based ostium and a smooth contour of the body. LA diverticulum is thought to represent remnants of the cardinal venous system during embryologic development. Histologically diverticula contain normal myocardial wall structure and contract in synchrony with the rest of the atrium. However, a rare type of diverticulum that does not contain myocytes and does not exhibit contractile properties has also been found and is often classified as aneurysm [9] (Fig. 1.14).< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


