Normal Anatomy
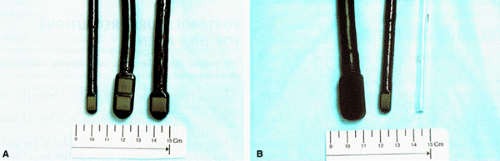
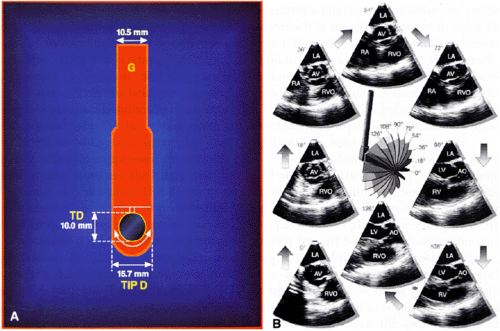
The first probes used for transesophageal echocardiography provided imaging in only a single plane. The development of the biplane probe, which had an imaging plane orthogonal to the transverse view obtained with single-plane devices, added considerably to the diagnostic information that could be obtained. The currently available multiplane probes make imaging studies much more flexible by allowing visualization of the in-between planes. In fact, the monoplane probe should now be regarded as obsolete. Smaller probes that enhance patient comfort and increase safety have become available. Images obtained with the smaller probes are usually not as good in quality as those obtained with the larger probes because the smaller probes have a smaller number of elements than do the larger probes.
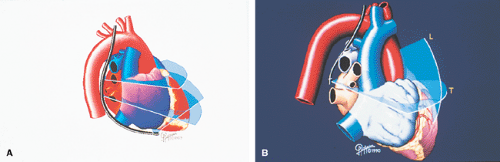
Although the planes discussed usually refer to the orientation of the transducer relative to the esophagus, the terms also apply to the heart because the esophagus is located directly behind the heart. However, the exact relationship of the esophagus to the heart varies from individual to individual so that it is not always possible to obtain in a given individual all the planes and structures described in this chapter. The position and size of air-filled structures such as the trachea and the left and right main bronchi also determine the ability to image cardiovascular structures optimally in the upper chest. As in transthoracic echocardiography, the anatomic structures imaged by the transesophageal approach are identified by comparing them to known cardiovascular anatomy and, in some instances, by the use of contrast echocardiography. Transverse plane imaging (0° angle on the multiplane probe) generally provides transverse or horizontal sections of the heart, whereas longitudinal plane imaging gives longitudinal or vertical sections. During longitudinal plane examination, clockwise rotation of the probe shifts the vertical plane to the right so that right-sided structures such as the superior vena cava and the right pulmonary veins are brought into view, whereas counterclockwise rotation results in imaging of left-sided structures such as the left atrial appendage and the left pulmonary veins. Therefore, obtaining transverse sections of the heart at various levels requires up-and-down movement of the probe; imaging of vertical sections, however, can be accomplished by mere rotation of the probe. The multiplane probe, like the biplane probe, can be moved up and down within the esophagus and can also be physically rotated in clockwise and counterclockwise directions to give both transverse and vertical sections. In addition, a manual switch on the handle rotates the transducer at the tip of the probe to provide oblique sections through the heart. Therefore, a comprehensive examination of various cardiac structures can be performed using the multiplane probe.
There is no universally agreed upon transesophageal approach for the examination of cardiac structures. In practice, however, one tends to first examine structures of immediate interest on the basis of clinical indications and transthoracic echo findings. In the awake patient, it is best not to begin examination with the probe placed high up in the esophagus or in the stomach because this may result in gagging and increased patient discomfort. We often begin examination with the probe in mid-esophagus and proceed with the examination of structures from a high esophageal or transgastric position only after the patient has relaxed, frequently toward the end of the study. However, for the sake of simplicity and convenience, the anatomic findings in this section of the Atlas are shown as if the examination commenced in the upper esophagus, with the probe advanced gradually down the esophagus into the stomach. Therefore, the great vessels and their branches or tributaries located at the base of the neck are displayed first, followed by the aortic valve and adjacent structures such as the coronary arteries and the pulmonary veins, the cardiac chambers and the atrioventricular valves, the descending thoracic aorta, and lastly, the structures visualized from the transgastric approach.
Transesophageal examination with the probe positioned in the upper esophagus is useful in imaging the
mid- and distal portions of the ascending aorta and the aortic arch and its branches. The innominate artery is the easiest branch to visualize, but other branches can also be imaged. Color Doppler–guided pulsed Doppler interrogation is useful in distinguishing an arterial branch from an accompanying vein. Flow signals from an artery are predominantly systolic, whereas the venous flow shows prominent systolic and diastolic components. Comprehensive evaluation of the aortic arch requires meticulous examination with a multiplane probe using transverse, longitudinal, and oblique planes. Because the aortic arch courses not only to the left but also posteriorly, the first, largest, and most anterior branch is the innominate artery; the left common carotid and the left subclavian arteries are identified arising more posteriorly. We have found longitudinal plane examination most useful in the identification of the aortic branches. Clockwise rotation with the probe set at an angle of 90° moves the plane to the right, bringing the origin of the innominate artery into view. Counterclockwise rotation of the probe, on the other hand, moves the vertical plane to the left, which helps in locating and identifying the left common carotid and left subclavian arteries. The innominate artery may also be followed to its bifurcation into the right common carotid and the right subclavian branches. The vein most commonly imaged when examining the aortic arch is the left innominate vein, but other veins such as the right innominate and the subclavian veins may also be visualized. Venous valves may occasionally be imaged as linear, mobile echoes in the tributaries of the major veins and should not be mistaken for a dissection flap. The main pulmonary artery and its branches, especially the left pulmonary artery, are often imaged adjacent to the aortic arch, and the left pulmonary artery can be followed to its branching into lobar arteries. A small portion of the left atrium may also be imaged next to the aortic arch. Contrast echocardiography has proved useful in identifying anatomic structures imaged in this region.
mid- and distal portions of the ascending aorta and the aortic arch and its branches. The innominate artery is the easiest branch to visualize, but other branches can also be imaged. Color Doppler–guided pulsed Doppler interrogation is useful in distinguishing an arterial branch from an accompanying vein. Flow signals from an artery are predominantly systolic, whereas the venous flow shows prominent systolic and diastolic components. Comprehensive evaluation of the aortic arch requires meticulous examination with a multiplane probe using transverse, longitudinal, and oblique planes. Because the aortic arch courses not only to the left but also posteriorly, the first, largest, and most anterior branch is the innominate artery; the left common carotid and the left subclavian arteries are identified arising more posteriorly. We have found longitudinal plane examination most useful in the identification of the aortic branches. Clockwise rotation with the probe set at an angle of 90° moves the plane to the right, bringing the origin of the innominate artery into view. Counterclockwise rotation of the probe, on the other hand, moves the vertical plane to the left, which helps in locating and identifying the left common carotid and left subclavian arteries. The innominate artery may also be followed to its bifurcation into the right common carotid and the right subclavian branches. The vein most commonly imaged when examining the aortic arch is the left innominate vein, but other veins such as the right innominate and the subclavian veins may also be visualized. Venous valves may occasionally be imaged as linear, mobile echoes in the tributaries of the major veins and should not be mistaken for a dissection flap. The main pulmonary artery and its branches, especially the left pulmonary artery, are often imaged adjacent to the aortic arch, and the left pulmonary artery can be followed to its branching into lobar arteries. A small portion of the left atrium may also be imaged next to the aortic arch. Contrast echocardiography has proved useful in identifying anatomic structures imaged in this region.
Advancement and rotation of the probe from the position where the aortic arch and its branches are identified brings into view the ascending aorta in short axis during transverse plane (0°) examination. The main pulmonary artery and a long segment of the right pulmonary artery can be seen wrapping around the aorta in this view. The origin and proximal portion of the left pulmonary artery may also be imaged. To the right of the aorta, the superior vena cava is imaged in short axis. The superior branch of the right pulmonary artery and segments of the right pulmonary veins may also be visualized. Longitudinal plane examination images the ascending aorta in long axis and the right pulmonary artery in short axis posterior to it. Further advancement of the probe images the aortic root, with the left atrium located posteriorly and the right ventricular outflow tract and pulmonary valve located anteriorly and to the left. All three aortic leaflets and sinuses can be easily identified using a multiplane probe. This is usually best accomplished at a plane angulation between 30° and 60°. During transverse plane examination, slight adjustment of the probe with rotation to the left brings the left atrial appendage and the left pulmonary veins (usually the left upper) into view; rotation to the right is used to image the right upper pulmonary vein and its junction with the left atrium. Slight advancement of the transducer often images the right lower pulmonary vein and its junction with the left atrium. Minimal withdrawal of the probe from the aortic root position with rotation to the left and right is used to identify the origins and proximal segments of the left and right coronary arteries, respectively. Longitudinal plane (90°) examination is used to view the aortic root and the proximal ascending aorta in long axis. Counterclockwise (leftward) rotation of the probe from this position views the right ventricular outflow tract, the pulmonary valve and the proximal main pulmonary artery in long axis. The anterior and posterior (inferior) leaflets of the tricuspid valve may also be identified in this vertical section. Further counterclockwise rotation displays the two-chamber view, in which the inferior and anterior free walls of the left ventricle are imaged together with the mitral valve, the left atrium, and the left atrial appendage. The left-sided pulmonary veins can also be imaged using this approach. Further counterclockwise rotation points the probe posteriorly and images the descending thoracic aorta in long axis. Clockwise (rightward) rotation of the probe from the aortic root position moves the vertical plane to the right, displaying the superior vena cava in long axis. The atrial septum and the fossa ovalis region are also often well visualized in this plane. Further clockwise rotation images the right upper pulmonary vein in long axis.
Advancement of the probe from the aortic root position during transverse plane (0°) examination usually displays the five-chamber view, in which the left ventricular outflow tract, aortic root, left atrium, mitral valve, right ventricle, and right atrium are imaged. Further advancement gives the four-chamber view, in which both the mitral (anterior and posterior leaflets) and tricuspid (anterior and septal leaflets) valves are imaged, in addition to the atrial septum, ventricular septum, both atria, and both ventricles. From this position, further advancement with some clockwise rotation during transverse plane (0°) imaging brings into view the openings of the inferior vena cava and coronary sinus into the right atrium, together with the eustachian and thebesian valves, the right atrial appendage, and the tricuspid inflow region. Leftward probe rotation may image the mitral valve in short axis. It is important to realize that at this point the transducer is close to the esophageal–gastric junction. Rotation of the probe with the transducer pointing posteriorly permits comprehensive examination of the descending thoracic aorta in the long, short, and oblique axes, and at all levels, by moving the transducer up and down the entire length of the esophagus. Azygos and hemiazygos veins and intercostal arteries and veins can be imaged. Higher up in the esophagus, the intervertebral discs together with
the spinal canal and the “pulsating” spinal cord within may also be viewed.
the spinal canal and the “pulsating” spinal cord within may also be viewed.
The probe can then be advanced into the stomach to view both the left and right ventricular cavities, the mitral and tricuspid valves, the chordae, and the papillary muscles in the long, short, and oblique axes. The aortic root, proximal ascending aorta, right ventricular outflow tract, and pulmonary valve may also be imaged from the transgastric approach. The abdominal aorta and its branches, for example, the celiac, superior mesenteric, and renal arteries and veins, as well as other abdominal structures, for example, the kidneys, spleen, pancreas, liver, and stomach, have been imaged using the transgastric approach.
Transesophageal Echocardiographic Examination
Indications
Transesophageal echocardiographic examination (TEE) is indicated in the following circumstances: to determine the cardiac source of an embolism; to diagnose or rule out suspected endocarditis; to check suspected prosthetic valve dysfunction; to assess for aortic dissection; to assess the severity of valvular regurgitation; to compensate for a poor acoustic window; and to detect congenital cardiac lesions.
Intraoperative Indications
TEE is used during surgery to assess the adequacy of a valve repair; to assess prosthetic valve or ring regurgitation; to monitor ventricular function; to evaluate removal of air from the heart; and to assess the adequacy of repair of congenital heart lesions.
Contraindications
TEE is contraindicated in the presence of esophageal tumor, stricture, diverticulum, fistulas, and previous esophageal surgery.
Esophageal varices and severe cervical spine problems are relative contraindications.
Complications
Complications are rare, but include esophageal bleeding, esophageal rupture, oropharyngeal injury, supraventricular tachycardia, laryngospasm, methemoglobinemia, and problems related to oversedation.
Performance of Transesophageal Echocardiography
Transesophageal echocardiography is now a well-developed procedure. There is no substitute for adequate training under expert supervision. Our recommended approach to the performance of transesophageal echocardiography is described in the following paragraphs.
Prerequisites
The physicians/cardiologists performing transesophageal echocardiography must have expertise in two-dimensional and conventional and color Doppler echocardiography.
They also must be fully trained in intubating the esophagus.
Procedure Room Setup
When performing TEE, the physician echocardiographer, a technologist echocardiographer or fellow, and a nurse are in attendance.
The procedure room is equipped with an examination table, an ultrasound machine, TEE probes, a bite guard, tongue depressors, gloves, a flashlight, a stethoscope, an intravenous (IV) setup, wall oxygen, suction apparatus, a fingertip oximeter, and a Dinamap (for blood pressure [BP] monitoring). Cardiopulmonary resuscitation (CPR) equipment and medications must be available. Sedatives and other medications must be on hand. Facilities for probe cleaning and sterilization are necessary.
Before Starting the Procedure
Before TEE is begun, discuss the case and the indications for the study with the referring physician. Ascertain that the probe has been sterilized as follows: (a) clean the probe with a mild cleansing agent and water, (b) immerse the probe in 2% glutaraldehyde (Cidex) or metricide for 20 minutes.
Remember
Transesophageal echocardiography is modestly invasive but is safe and feasible in 98% to 99% of patients. This procedure is well tolerated by critically ill patients and also by elderly patients.
Establish rapport with the patient. Explain the procedure fully, including its benefits and risks. Obtain informed consent. Verify that the patient has been fasting for the preceding 4 to 6 hours.
Question the patient closely about any dysphagia; esophageal problems (e.g., diverticula, strictures, rings, carcinoma); operations on the esophagus, throat, or chest, especially in childhood; any thoracic radiation; hematemesis; or allergies. If there is a question of dysphagia or the history is not clear-cut, perform a barium swallow to make sure the esophagus is normal.
Determine whether the patient has severe pulmonary disease, including chronic obstructive pulmonary disease (COPD) or bronchial asthma.
Perform a brief cardiovascular examination, check vital signs, and perform auscultation of the lungs. Check O2 saturation with fingertip oximetry. Check the mouth and throat. Look for loose teeth and remove any dentures. If the patient’s BP is too high, nifedipine, 5 to 10 mg sublingually, can help bring it down.
Inspect the CPR equipment. Insert an IV line, or, if one is already in place, check its patency. Give prophylactic antibiotics if the patient has a prosthetic valve or any other internal device such as a defibrillator, if the patient is at increased risk for endocarditis (e.g., bad teeth or gums, previous history of endocarditis), or if the referring physician recommends them. Follow American Heart Association (AHA) guidelines for endoscopy procedures when giving antibiotics.
Prophylactic Antibiotics. The gastroenterology and infectious disease literature suggests no serious bacteremia or increased chances of endocarditis for endoscopy procedures without biopsy. No evidence has been adduced that mandates bacterial endocarditis prophylaxis for this procedure, and it is reasonable to use none. Nevertheless, many physicians prefer to employ antibiotics in an attempt to forestall endocarditis, particularly if the patient has a prosthetic valve. In this event, give ampicillin, 2 g intravenously in 50 mL of D5W (5% dextrose in water) or 0.9% NaCl, and then gentamycin 1.5 mg/kg intravenously in the same manner after vigorously flushing the IV system, 30 minutes before the procedure. This may be repeated in 8 hours. If the patient is allergic to penicillin, give gentamycin first, flush the IV system vigorously, and then give vancomycin 1 g intravenously over 60 minutes in 50 mL D5W or 0.9% NaCl. This may be repeated in 8 to 12 hours. For children, follow the same technique but adjust the dosages as follows: ampicillin 50 mg/kg, gentamycin 2.0 mg/kg, vancomycin 20 mg/kg.
Anesthesia and Sedation. Check the suction apparatus. Anesthetize the pharynx with 20% benzocaine spray to suppress the gag reflex and retching. Each spray should be 1 second in duration, and the patient should gargle for at least 1 minute before swallowing. Two or three sprays are usually sufficient to suppress the gag reflex, which should be tested using a tongue depressor following each spray. In some patients, the gag reflex is suppressed immediately after using the spray; in others the effect may be delayed for as long as 5 minutes. The duration of gag reflex suppression also varies from individual to individual, from a few minutes to several minutes. It is advisable not to use too much of the spray because potentially fatal methemoglobinemia resulting in oxygen desaturation and cyanosis may occur in susceptible patients. If methemoglobinemia is suspected, do a blood gas analysis to confirm it and immediately give methylene blue intravenously. If necessary, give an anticholinergic agent such as glycopyrrolate, 0.2 mg intravenously, to reduce salivary and gastroenterologic secretions.
Give IV sedation if the patient is very apprehensive. Begin with low doses, and increase if necessary. If the patient has pulmonary disease or is elderly, give no or minimal sedation. No sedation should be given if the patient plans to drive home.
The most commonly used sedative is midazolam (Versed), 0.5 to 5 mg. This causes anterograde amnesia, but respiratory arrest can occur. The effect of midazolam can be reversed by flumazenil (Romazicon), 1.0 mg. Other commonly used sedatives are morphine, 1 to 4 mg; Phenergan, 12.5 to 25 mg; diazepam (Valium), 1 to 5 mg; and meperidine (Demerol), 12.5 to 50 mg. The effect of Demerol can be reversed by naloxone (Narcaine), 0.4 to 0.8 mg. More sedation is desirable to lower the patient’s BP if aortic dissection is suspected, because BP often increases following benzocaine spray.
Final Preparations. Select the appropriate probe. Check for any breakage, and make sure the probe is sterilized. Check whether the transducers are operational and the echo system is in appropriate working condition. Unlock it if it is locked. Stop IV heparin at least 2 hours before the procedure.
Performance of the Procedure
Flex the patient’s neck with the patient in the left lateral decubitus position. Place a bite guard in the patient’s mouth. Apply gel liberally to the probe, up to at least 15 to 20 cm, flex it slightly, insert it in the patient’s mouth through the bite guard, and ask the patient to swallow when he or she feels it at the back of the throat. If necessary, guide the probe by inserting one finger along the side of the bite guard. This prevents the patient from biting the operator’s fingers or damaging the probe. An alternative approach is to ask the patient to open his or her mouth, grasp the probe near the transducer between the index and middle fingers, and direct it at the back of the pharynx, asking the patient to swallow it. A bite-block, previously placed on the probe, is then advanced into the mouth.
Remember that patient cooperation is required for swallowing the probe. If too much of sedation is given, the patient may not be able to cooperate.
Gently advance the probe into the esophagus up to 30 or 35 cm. Then stop to let the patient get used to the probe for 1 to 3 minutes, especially if he or she is retching or gagging. Keeping the probe stationary allows any gagging to pass. It also allows the patient’s heart rate and BP to revert toward baseline. Monitor the patient’s vital signs and O2 saturation with Dinamap, fingertip oximetry, and one-lead electrocardiography (ECG) on the echo monitor while the probe is being passed and afterward. Suction intermittently and as required. Give oxygen if needed.
Never advance the probe if any resistance is encountered. Warn the patient not to swallow secretions after probe passage and to signal if suctioning is needed. Withdrawing the probe into the esophagus is helpful if nausea or vomiting occurs when it is in the stomach. If a vasovagal episode or hypotension occurs, lower the
head end of the table and give atropine, 0.5 to 1.0 mg intravenously, and run IV fluids and IV pressor agents.
head end of the table and give atropine, 0.5 to 1.0 mg intravenously, and run IV fluids and IV pressor agents.
Perform a multiplane examination of each chamber and structure using various angulations from 0° to 180°. A good approach is to begin by addressing the problem that precipitated the examination in case the patient is not able to tolerate the probe and the procedure has to be terminated early.
The Intubated Patient
It may be difficult to pass a probe beyond an inflated endotracheal cuff in an intubated patient. In such a case, briefly deflate the cuff as the probe meets resistance from the cuff and then immediately reinflate it when the probe has passed beyond it. Extending the patient’s neck often is helpful in passing the probe when the cuff is not deflated. A good rule is to keep the probe parallel and close to the endotracheal tube while advancing it. Some physicians also remove any nasogastric tube to facilitate probe passage. In the very uncooperative intubated patient, temporary pharmacologic paralysis may facilitate performance of the procedure.
After the Procedure
Check the tip of the probe for any evidence of bleeding. Check the patient’s mouth and pharynx for any abrasions or other trauma. Monitor vital signs for 20 to 30 minutes. The patient can leave with a caregiver once the sedative effect has worn off.
Postprocedure Precautions for the Patient
The patient should be given the following instructions after the procedure:
Do not swallow, eat, or drink for 1 to 2 hours after the procedure.
Do not drive or operate machinery for at least 12 hours after the procedure.
Have another person drive home if sedation was used.
Report to physician if sore throat persists for >2 days.
See a physician immediately if bleeding occurs from the mouth, the IV site becomes painful and inflamed, or fever or other symptoms develop.
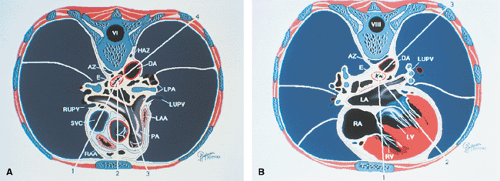 FIGURE 1.4. Transverse sections. A and B show sections obtained at the level of the sixth (A) and eighth (B) vertebrae. AZ, azygos; DA, descending thoracic aorta; E, esophagus; HAZ, hemiazygos vein; LA, left atrium; LAA, left atrial appendage; LPA, left pulmonary artery; LUPV, left upper pulmonary vein; LV, left ventricle; PA, main pulmonary artery; RA, right atrium; RAA
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|